EpiPen
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
EpiPen is a non-selective alpha and beta-adrenergic receptor agonist that is FDA approved for the {{{indicationType}}} of allergic reactions (Type I) including anaphylaxis. Common adverse reactions include anxiety, apprehensiveness, restlessness, tremor, weakness, dizziness, sweating, palpitations, pallor, nausea and vomiting, headache, and/or respiratory difficulties..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Emergency Treatment Of Allergic Reactions (Type I)
- EpiPen and EpiPen Jr are indicated in the emergency treatment of allergic reactions (Type I) including anaphylaxis to stinging insects (e.g., order Hymenoptera, which include bees, wasps, hornets, yellow jackets and fire ants) and biting insects (e.g., triatoma, mosquitoes), allergen immunotherapy, foods, drugs, diagnostic testing substances (e.g., radiocontrast media) and other allergens, as well as idiopathic anaphylaxis or exercise-induced anaphylaxis.
- EpiPen and EpiPen Jr are intended for immediate administration in patients who are determined to be at increased risk for anaphylaxis, including individuals with a history of anaphylactic reactions.
- Anaphylactic reactions may occur within minutes after exposure and consist of flushing, apprehension, syncope, tachycardia, thready or unobtainable pulse associated with a fall in blood pressure, convulsions, vomiting, diarrhea and abdominal cramps, involuntary voiding, wheezing, dyspnea due to laryngeal spasm, pruritus, rashes, urticaria or angioedema.
- EpiPen and EpiPen Jr are intended for immediate administration as emergency supportive therapy only and are not a substitute for immediate medical care.
- Dosing Information
- Selection of the appropriate dosage strength (EpiPen 0.3 mg or EpiPen Jr 0.15 mg) is determined according to patient body weight.
- Patients greater than or equal to 30 kg (approximately 66 pounds or more): EpiPen 0.3 mg
- Patients 15 to 30 kg (33 pounds to 66 pounds): EpiPen Jr 0.15 mg
- Inject EpiPen or EpiPen Jr intramuscularly or subcutaneously into the anterolateral aspect of the thigh, through clothing if necessary.
- Each EpiPen or EpiPen Jr contains a single dose of epinephrine for single-use injection. Since the doses of epinephrine delivered from EpiPen or EpiPen Jr are fixed, consider using other forms of injectable epinephrine if doses lower than 0.15 mg are deemed necessary.
- Selection of the appropriate dosage strength (EpiPen 0.3 mg or EpiPen Jr 0.15 mg) is determined according to patient body weight.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Acute Symptomatic Bradyarrhythmia
- Developed by: ACC/AHA
- Class of Recommendation: Class IIb
- Strength of Evidence: Category B
- If atropine is ineffective for the treatment of bradycardia with a pulse, then epinephrine or dopamine may be used, especially, with associated hypotension.[1]
Non–Guideline-Supported Use
Gastrointestinal Hemorrhage
- Endoscopic injection of epinephrine is effective in the treatment of upper gastrointestinal hemorrhage.[2][3][4]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Emergency Treatment Of Allergic Reactions (Type I)
- EpiPen and EpiPen Jr are indicated in the emergency treatment of allergic reactions (Type I) including anaphylaxis to stinging insects (e.g., order Hymenoptera, which include bees, wasps, hornets, yellow jackets and fire ants) and biting insects (e.g., triatoma, mosquitoes), allergen immunotherapy, foods, drugs, diagnostic testing substances (e.g., radiocontrast media) and other allergens, as well as idiopathic anaphylaxis or exercise-induced anaphylaxis.
- EpiPen and EpiPen Jr are intended for immediate administration in patients who are determined to be at increased risk for anaphylaxis, including individuals with a history of anaphylactic reactions.
- Anaphylactic reactions may occur within minutes after exposure and consist of flushing, apprehension, syncope, tachycardia, thready or unobtainable pulse associated with a fall in blood pressure, convulsions, vomiting, diarrhea and abdominal cramps, involuntary voiding, wheezing, dyspnea due to laryngeal spasm, pruritus, rashes, urticaria or angioedema.
- EpiPen and EpiPen Jr are intended for immediate administration as emergency supportive therapy only and are not a substitute for immediate medical care.
- Dosing Information
- Selection of the appropriate dosage strength (EpiPen 0.3 mg or EpiPen Jr 0.15 mg) is determined according to patient body weight.
- Patients greater than or equal to 30 kg (approximately 66 pounds or more): EpiPen 0.3 mg
- Patients 15 to 30 kg (33 pounds to 66 pounds): EpiPen Jr 0.15 mg
- Inject EpiPen or EpiPen Jr intramuscularly or subcutaneously into the anterolateral aspect of the thigh, through clothing if necessary.
- Each EpiPen or EpiPen Jr contains a single dose of epinephrine for single-use injection. Since the doses of epinephrine delivered from EpiPen or EpiPen Jr are fixed, consider using other forms of injectable epinephrine if doses lower than 0.15 mg are deemed necessary.
- Selection of the appropriate dosage strength (EpiPen 0.3 mg or EpiPen Jr 0.15 mg) is determined according to patient body weight.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of EpiPen in pediatric patients.
Non–Guideline-Supported Use
Croup
- Aerosolized levo-epinephrine (1:1000) is at least as effective as racemic epinephrine (2.25%) in the treatment of laryngotracheitis in children (6 months to 6 years of age) with moderate to severe croup.[5]
Wheezing
- Subcutaneous epinephrine is effective in the treatment of acute wheezing in children less than 2 years of age.[6]
Contraindications
- None
Warnings
Precautions
- Emergency Treatment
- EpiPen and EpiPen Jr are intended for immediate administration as emergency supportive therapy and are not intended as a substitute for immediate medical care. In conjunction with the administration of epinephrine, the patient should seek immediate medical or hospital care. More than two sequential doses of epinephrine should only be administered under direct medical supervision.
- Incorrect Locations of Injection
- EpiPen and EpiPen Jr should only be injected into the anterolateral aspect of the thigh [see Dosage and Administration (2) and Patient Counseling Information (17)].
- Do not inject intravenously. Large doses or accidental intravenous injection of epinephrine may result in cerebral hemorrhage due to sharp rise in blood pressure. Rapidly acting vasodilators can counteract the marked pressor effects of epinephrine if there is such inadvertent administration.
- Do not inject into buttock. Injection into the buttock may not provide effective treatment of anaphylaxis. Advise the patient to go immediately to the nearest emergency room for further treatment of anaphylaxis. Additionally, injection into the buttock has been associated with gas gangrene. Cleansing with alcohol does not kill bacterial spores, and therefore, does not lower this risk.
- Do not inject into digits, hands or feet. Since epinephrine is a strong vasoconstrictor, accidental injection into the digits, hands or feet may result in loss of blood flow to the affected area. Advise the patient to go immediately to the nearest emergency room and to inform the healthcare provider in the emergency room of the location of the accidental injection. Treatment of such inadvertent administration should consist of vasodilation, in addition to further appropriate treatment of anaphylaxis [ see Adverse Reactions (6)].
- EpiPen and EpiPen Jr should only be injected into the anterolateral aspect of the thigh [see Dosage and Administration (2) and Patient Counseling Information (17)].
- Allergic Reactions Associated With Sulfite
- The presence of a sulfite in this product should not deter administration of the drug for treatment of serious allergic or other emergency situations even if the patient is sulfite-sensitive.
- Epinephrine is the preferred treatment for serious allergic reactions or other emergency situations even though this product contains sodium metabisulfite, a sulfite that may, in other products, cause allergic-type reactions including anaphylactic symptoms or life-threatening or less severe asthmatic episodes in certain susceptible persons.
- The alternatives to using epinephrine in a life-threatening situation may not be satisfactory.
- Disease Interactions
- Some patients may be at greater risk for developing adverse reactions after epinephrine administration. Despite these concerns, it should be recognized that the presence of these conditions is not a contraindication to epinephrine administration in an acute, life-threatening situation. Therefore, patients with these conditions, and/or any other person who might be in a position to administer EpiPen or EpiPen Jr to a patient experiencing anaphylaxis should be carefully instructed in regard to the circumstances under which epinephrine should be used.
- Patients with Heart Disease
- Epinephrine should be administered with caution to patients who have heart disease, including patients with cardiac arrhythmias, coronary artery or organic heart disease, or hypertension. In such patients, or in patients who are on drugs that may sensitize the heart to arrhythmias, epinephrine may precipitate or aggravate angina pectoris as well as produce ventricular arrhythmias.
- Other Patients and Diseases
- Epinephrine should be administered with caution to patients with hyperthyroidism, diabetes, elderly individuals, and pregnant women. Patients with Parkinson’s disease may notice a temporary worsening of symptoms.
Adverse Reactions
Clinical Trials Experience
- Due to the lack of randomized, controlled clinical trials of epinephrine for the treatment of anaphylaxis, the true incidence of adverse reactions associated with the systemic use of epinephrine is difficult to determine. Adverse reactions reported in observational trials, case reports, and studies are listed below.
- Common adverse reactions to systemically administered epinephrine include anxiety; apprehensiveness; restlessness; tremor; weakness; dizziness; sweating; palpitations; pallor; nausea and vomiting; headache; and/or respiratory difficulties. These symptoms occur in some persons receiving therapeutic doses of epinephrine, but are more likely to occur in patients with hypertension or hyperthyroidism [see Warnings and Precautions (5.4)].
- Arrhythmias, including fatal ventricular fibrillation, have been reported, particularly in patients with underlying cardiac disease or those receiving certain drugs [see Warnings and Precautions (5.4) and Drug Interactions (7)].
- Rapid rises in blood pressure have produced cerebral hemorrhage, particularly in elderly patients with cardiovascular disease [see Warnings and Precautions (5.4)].
- Angina may occur in patients with coronary artery disease [see Warnings and Precautions (5.4)].
- Accidental injection into the digits, hands or feet may result in loss of blood flow to the affected area [see Warnings and Precautions (5.2)].
- Adverse events experienced as a result of accidental injections may include increased heart rate, local reactions including injection site pallor, coldness and hypoesthesia or injury at the injection site resulting in bruising, bleeding, discoloration, erythema or skeletal injury.
- Injection into the buttock has resulted in cases of gas gangrene.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of EpiPen in the drug label.
Drug Interactions
- Patients who receive epinephrine while concomitantly taking cardiac glycosides, diuretics, or anti-arrhythmics should be observed carefully for the development of cardiac arrhythmias [see Warnings and Precautions (5.4)].
- The effects of epinephrine may be potentiated by tricyclic antidepressants, monoamine oxidase inhibitors, levothyroxine sodium, and certain antihistamines, notably chlorpheniramine, tripelennamine, and diphenhydramine.
- The cardiostimulating and bronchodilating effects of epinephrine are antagonized by beta- adrenergic blocking drugs, such as propranolol.
- The vasoconstricting and hypertensive effects of epinephrine are antagonized by alpha- adrenergic blocking drugs, such as phentolamine.
- Ergot alkaloids may also reverse the pressor effects of epinephrine.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- There are no adequate and well controlled studies of the acute effect of epinephrine in pregnant women.
- Epinephrine was teratogenic in rabbits, mice and hamsters. Epinephrine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus (fetal anoxia, spontaneous abortion, or both).
- Epinephrine has been shown to have teratogenic effects when administered subcutaneously in rabbits at approximately 30 times the maximum recommended daily subcutaneous or intramuscular dose (on a mg/m2 basis at a maternal dose of 1.2 mg/kg/day for two to three days), in mice at approximately 7 times the maximum daily subcutaneous or intramuscular dose (on a mg/m2 basis at a maternal subcutaneous dose of 1 mg/kg/day for 10 days), and in hamsters at approximately 5 times the maximum recommended daily subcutaneous or intramuscular dose (on a mg/m2 basis at a maternal subcutaneous dose of 0.5 mg/kg/day for 4 days).
- These effects were not seen in mice at approximately 3 times the maximum recommended daily subcutaneous or intramuscular dose (on a mg/m2 basis at a subcutaneous maternal dose of 0.5 mg/kg/day for 10 days).
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of EpiPen in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of EpiPen during labor and delivery.
Nursing Mothers
- It is not known whether epinephrine is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when EpiPen is administered to a nursing woman.
Pediatric Use
- EpiPen or EpiPen Jr may be administered to pediatric patients at a dosage appropriate to body weight. Clinical experience with the use of epinephrine suggests that the adverse reactions seen in children are similar in nature and extent to those both expected and reported in adults. Since the doses of epinephrine delivered from EpiPen and EpiPen Jr are fixed, consider using other forms of injectable epinephrine if doses lower than 0.15 mg are deemed necessary.
Geriatic Use
- Clinical studies for the treatment of anaphylaxis have not been performed in subjects aged 65 and over to determine whether they respond differently from younger subjects. However, other reported clinical experience with use of epinephrine for the treatment of anaphylaxis has identified that geriatric patients may be particularly sensitive to the effects of epinephrine. Therefore, EpiPen should be administered with caution in elderly individuals, who may be at greater risk for developing adverse reactions after epinephrine administration.
Gender
There is no FDA guidance on the use of EpiPen with respect to specific gender populations.
Race
There is no FDA guidance on the use of EpiPen with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of EpiPen in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of EpiPen in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of EpiPen in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of EpiPen in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intramuscular
Monitoring
There is limited information regarding Monitoring of EpiPen in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of EpiPen in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Overdosage of epinephrine may produce extremely elevated arterial pressure, which may result in cerebrovascular hemorrhage, particularly in elderly patients. Overdosage may also result in pulmonary edema because of peripheral vascular constriction together with cardiac stimulation. Treatment consists of rapidly acting vasodilators or alpha-adrenergic blocking drugs and/or respiratory support.
- Epinephrine overdosage can also cause transient bradycardia followed by tachycardia, and these may be accompanied by potentially fatal cardiac arrhythmias. Premature ventricular contractions may appear within one minute after injection and may be followed by multifocal ventricular tachycardia (prefibrillation rhythm). Subsidence of the ventricular effects may be followed by atrial tachycardia and occasionally by atrioventricular block. Treatment of arrhythmias consists of administration of a beta-adrenergic blocking drug such as propranolol.
- Overdosage sometimes results in extreme pallor and coldness of the skin, metabolic acidosis, and kidney failure.
Management
- Suitable corrective measures must be taken in such situations.
Chronic Overdose
There is limited information regarding Chronic Overdose of EpiPen in the drug label.
Pharmacology
| |
EpiPen
| |
| Systematic (IUPAC) name | |
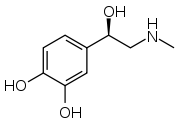
| (R)-4-(1-Hydroxy-2-(methylamino)ethyl)benzene-1,2-diol | |
| Identifiers | |
| CAS number | |
| ATC code | A01 B02BC09 (WHO) C01CA24 (WHO) R01AA14 (WHO) R03AA01 (WHO) S01EA01 (WHO) |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 183.204 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | adrenergic synapse (MAO and COMT) |
| Half life | 2 minutes |
| Excretion | Urine |
| Therapeutic considerations | |
| Pregnancy cat. |
C(US) |
| Legal status | |
| Routes | IV, IM, endotracheal, IC, Nasal Ophthalmic |
Mechanism of Action
- Epinephrine acts on both alpha- and beta-adrenergic receptors.
Structure
- EpiPen (epinephrine injection, USP) 0.3 mg and EpiPen Jr (epinephrine injection, USP) 0.15 mg are auto-injectors and combination products containing drug and device components.
- Each EpiPen Auto-Injector, 0.3 mg delivers a single dose of 0.3 mg epinephrine from epinephrine injection, USP 1:1000 (0.3 mL) in a sterile solution.
- Each EpiPen Jr Auto-Injector, 0.15 mg delivers a single dose of 0.15 mg epinephrine from epinephrine injection, USP 1:2000 (0.3 mL) in a sterile solution.
- The EpiPen and EpiPen Jr each contain 2 mL epinephrine solution. Approximately 1.7 mL remains in the auto-injector after activation, but is not available for future use, and should be discarded.
- Each 0.3 mL in the EpiPen Auto-Injector contains 0.3 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2–5.0.
- Each 0.3 mL in the EpiPen Jr Auto-Injector contains 0.15 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0.
- Epinephrine is a sympathomimetic catecholamine. Chemically, epinephrine is (-)-3,4- Dihydroxy-α-[(methylamino)methyl]benzyl alcohol with the following structure:
- Epinephrine solution deteriorates rapidly on exposure to air or light, turning pink from oxidation to adrenochrome and brown from the formation of melanin. Replace EpiPen and EpiPen Jr if the epinephrine solution appears discolored (pinkish or brown color), cloudy, or contains particles.
- Thoroughly review the patient instructions and operation of EpiPen or EpiPen Jr with patients and caregivers prior to use.
Pharmacodynamics
- Through its action on alpha-adrenergic receptors, epinephrine lessens the vasodilation and increased vascular permeability that occurs during anaphylaxis, which can lead to loss of intravascular fluid volume and hypotension.
- Through its action on beta-adrenergic receptors, epinephrine causes bronchial smooth muscle relaxation and helps alleviate bronchospasm, wheezing and dyspnea that may occur during anaphylaxis.
- Epinephrine also alleviates pruritus, urticaria, and angioedema and may relieve gastrointestinal and genitourinary symptoms associated with anaphylaxis because of its relaxer effects on the smooth muscle of the stomach, intestine, uterus and urinary bladder.
- When given subcutaneously or intramuscularly, epinephrine has a rapid onset and short duration of action.
Pharmacokinetics
There is limited information regarding Pharmacokinetics of EpiPen in the drug label.
Nonclinical Toxicology
- Long-term studies to evaluate the carcinogenic potential of epinephrine have not been conducted.
- Epinephrine and other catecholamines have been shown to have mutagenic potential in vitro and to be an oxidative mutagen in a WP2 bacterial reverse mutation assay.
- Epinephrine was positive in the DNA Repair test with B. subtilis (REC) assay, but was not mutagenic in the Salmonella bacterial reverse mutation assay.
- The potential for epinephrine to impair fertility has not been evaluated.
Clinical Studies
There is limited information regarding Clinical Studies of EpiPen in the drug label.
How Supplied
- EpiPen Auto-Injectors (epinephrine injections, USP, 1:1000, 0.3 mL) are available as EpiPen 2-Pak®, NDC 49502-500-02, a pack that contains two EpiPen Auto-Injectors (epinephrine injections, USP, 1:1000, 0.3 mL) and one EpiPen Auto-Injector trainer device.
- EpiPen Jr Auto-Injectors (epinephrine injections, USP, 1:2000, 0.3 mL) are available as EpiPen Jr 2-Pak®, NDC 49502-501-02, a pack that contains two EpiPen Jr Auto-Injectors (epinephrine injections, USP, 1:2000, 0.3 mL) and one EpiPen Auto-Injector trainer device.
- EpiPen 2-Pak® and EpiPen Jr 2-Pak® also includes an S-clip to clip two carrier tubes together.
- Storage and Handling
- Protect from light. Epinephrine is light sensitive and should be stored in the carrier tube provided to protect it from light. Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) (See USP Controlled Room Temperature). Do not refrigerate. Before using, check to make sure the solution in the auto-injector is clear and colorless. Replace the auto-injector if the solution is discolored (pinkish or brown color), cloudy, or contains particles.
Storage
There is limited information regarding EpiPen Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::EpiPen |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::EpiPen |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- A healthcare provider should review the patient instructions and operation of EpiPen and EpiPen Jr in detail, with the patient or caregiver.
- Epinephrine is essential for the treatment of anaphylaxis. Patients who are at risk of or with a history of severe allergic reactions (anaphylaxis) to insect stings or bites, foods, drugs, and other allergens, as well as idiopathic and exercise-induced anaphylaxis, should be carefully instructed about the circumstances under which epinephrine should be used.
- Administration and Training
- Patients and/or caregivers should be instructed in the appropriate use of EpiPen and EpiPen Jr. EpiPen should be injected into the middle of the outer thigh (through clothing, if necessary). Each device is a single-use injection. Advise patients to seek immediate medical care in conjunction with administration of EpiPen.
- Complete patient information, including dosage, directions for proper administration and precautions can be found inside each EpiPen or EpiPen Jr carton. A printed label on the surface of EpiPen shows instructions for use and a diagram depicting the injection process.
- Patients and/or caregivers should be instructed to use the Trainer to familiarize themselves with the use of EpiPen in an allergic emergency. The Trainer may be used multiple times. A Trainer device is provided in 2-Pak cartons.
- Adverse Reactions
- Epinephrine may produce symptoms and signs that include an increase in heart rate, the sensation of a more forceful heartbeat, palpitations, sweating, nausea and vomiting, difficulty breathing, pallor, dizziness, weakness or shakiness, headache, apprehension, nervousness, or anxiety. These signs and symptoms usually subside rapidly, especially with rest, quiet and recumbency. Patients with hypertension or hyperthyroidism may develop more severe or persistent effects, and patients with coronary artery disease could experience angina. Patients with diabetes may develop increased blood glucose levels following epinephrine administration. Patients with Parkinson’s disease may notice a temporary worsening of symptoms.
- Accidental Injection
- Advise patients to seek immediate medical care in the case of accidental injection. Since epinephrine is a strong vasoconstrictor when injected into the digits, hands, or feet, treatment should be directed at vasodilatation if there is such an accidental injection to these areas.
- Storage and Handling
- Instruct patients to inspect the epinephrine solution visually through the clear window of the auto-injector periodically. EpiPen and EpiPen Jr should be replaced if the epinephrine solution appears discolored (pinkish or brown color), cloudy, or contains particles. Epinephrine is light sensitive and should be stored in the carrier tube provided to protect it from light. The carrier tube is not waterproof. Patients should be instructed that EpiPen and EpiPen Jr must be used or properly disposed once the blue safety release is removed or after use.
Precautions with Alcohol
- Alcohol-EpiPen interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- EpiPen®[7]
Look-Alike Drug Names
- EPINEPHrine® — ePHEDrine®[8]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Neumar, Robert W. (2010-11-02). "Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): –729-767. doi:10.1161/CIRCULATIONAHA.110.970988. ISSN 1524-4539. PMID 20956224. Unknown parameter
|coauthors=ignored (help) - ↑ Chung, S. C. (1988-06-11). "Endoscopic injection of adrenaline for actively bleeding ulcers: a randomised trial". British Medical Journal (Clinical Research Ed.). 296 (6637): 1631–1633. ISSN 0267-0623. PMC 2546160. PMID 3135047. Unknown parameter
|coauthors=ignored (help) - ↑ Hirao, M. (1988-06). "Endoscopic resection of early gastric cancer and other tumors with local injection of hypertonic saline-epinephrine". Gastrointestinal Endoscopy. 34 (3): 264–269. ISSN 0016-5107. PMID 3391382. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Folwaczny, C. (1997-01). "Influence of prophylactic local administration of epinephrine on bleeding complications after polypectomy". Endoscopy. 29 (1): 31–33. doi:10.1055/s-2007-1004058. ISSN 0013-726X. PMID 9083734. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Waisman, Y. (1992-02). "Prospective randomized double-blind study comparing L-epinephrine and racemic epinephrine aerosols in the treatment of laryngotracheitis (croup)". Pediatrics. 89 (2): 302–306. ISSN 0031-4005. PMID 1734400. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Lowell, D. I. (1987-06). "Wheezing in infants: the response to epinephrine". Pediatrics. 79 (6): 939–945. ISSN 0031-4005. PMID 3295741. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Empty citation (help)
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=EpiPen |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=EpiPen |Label Name=EpiPen04.png
}}
{{#subobject:
|Label Page=EpiPen |Label Name=EpiPen05.png
}}
{{#subobject:
|Label Page=EpiPen |Label Name=EpiPen06.png
}}
{{#subobject:
|Label Page=EpiPen |Label Name=EpiPen07.png
}}
{{#subobject:
|Label Page=EpiPen |Label Name=EpiPen08.png
}}


