Wolff-Parkinson-White syndrome medical therapy: Difference between revisions
Ahmed Zaghw (talk | contribs) |
Rim Halaby (talk | contribs) No edit summary |
||
| Line 15: | Line 15: | ||
| language = Italian }}</ref> If radiofrequency catheter ablation is successfully performed, the patient is generally considered cured. Recurrence rates are typically less than 5% after a successful ablation.<ref name = Pappone_et_al_1993 /> The one caveat is that individuals with underlying [[Ebstein's anomaly]] may develop additional accessory pathways during progression of their disease. | | language = Italian }}</ref> If radiofrequency catheter ablation is successfully performed, the patient is generally considered cured. Recurrence rates are typically less than 5% after a successful ablation.<ref name = Pappone_et_al_1993 /> The one caveat is that individuals with underlying [[Ebstein's anomaly]] may develop additional accessory pathways during progression of their disease. | ||
== | ==Acute Treatment== | ||
===Atrioventricular Reentrant Tachycardia (AVRT)=== | |||
==Atrial Fibrillation== | ===Atrial Fibrillation=== | ||
* Patients can experience high rates during [[Atrial fibrillation|AFib]] because of conduction over the accessory pathway which can have a very short refractory period. | * Patients can experience high rates during [[Atrial fibrillation|AFib]] because of conduction over the accessory pathway which can have a very short refractory period. | ||
* Mean ventricular rates in these patients range from 160 to 300 BPM. | * Mean ventricular rates in these patients range from 160 to 300 BPM. | ||
| Line 37: | Line 26: | ||
* If the ventricular rate during the [[Atrial fibrillation|AFib]] is not > 200, then you could try [[procainamide]], [[disopyramide]], or [[quinidine]] which may prolong the refractory period of the accessory pathway. | * If the ventricular rate during the [[Atrial fibrillation|AFib]] is not > 200, then you could try [[procainamide]], [[disopyramide]], or [[quinidine]] which may prolong the refractory period of the accessory pathway. | ||
== | ==Long Term Management== | ||
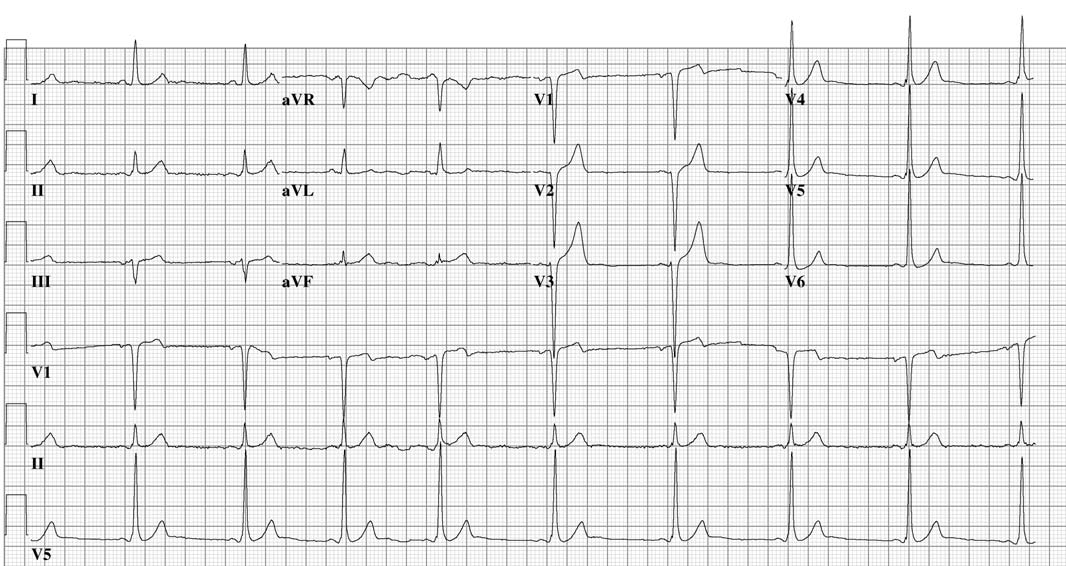
Shown below is an EKG of a 24 years old man with Mahaim type of preexcitation. | Shown below is an EKG of a 24 years old man with Mahaim type of preexcitation. | ||
Revision as of 03:08, 17 April 2014
|
Wolff-Parkinson-White syndrome Microchapters |
|
Differentiating Wolff-Parkinson-White syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Wolff-Parkinson-White syndrome medical therapy On the Web |
|
Risk calculators and risk factors for Wolff-Parkinson-White syndrome medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Acutely, people with WPW who are experiencing a tachydysrhythmia may require electrical cardioversion if their condition is critical, or, if more stable, medical treatment may be used. Patients with atrial fibrillation and rapid ventricular response are often treated with amiodarone orprocainamide to stabilize their heart rate. Adenosine and other AV node blockers should be avoided in Atrial fibriliiatin with WPW; this inlcudes adenosine, diltiazem, verapamil,other calcium channel blockers and Beta-blockers. Patients with a rapid heart beat with narrow QRS complexes (circus movement tachycardias) may also be cardioverted, alternatively, adenosine may be administered if equipment for cardioversion is immediately available as a backup.
The definitive treatment of WPW syndrome is a destruction of the abnormal electrical pathway by radiofrequency catheter ablation. This procedure is performed almost exclusively by cardiac electrophysiologists. Radiofrequency catheter ablation is not performed in all individuals with WPW syndrome because there are inherent risks involved in the procedure. Adeosine is contraindicated for patients in atrial fibrillation or atrial flutter with a history of WPW
When performed by an experienced electrophysiologist, radiofrequency ablation has a high success rate.[1] If radiofrequency catheter ablation is successfully performed, the patient is generally considered cured. Recurrence rates are typically less than 5% after a successful ablation.[1] The one caveat is that individuals with underlying Ebstein's anomaly may develop additional accessory pathways during progression of their disease.
Acute Treatment
Atrioventricular Reentrant Tachycardia (AVRT)
Atrial Fibrillation
- Patients can experience high rates during AFib because of conduction over the accessory pathway which can have a very short refractory period.
- Mean ventricular rates in these patients range from 160 to 300 BPM.
- During these attacks there is not only the risk of hemodynamic compromise but also a risk of degenerate into VF.
- As a rule dig should be avoided in these patients.
- Cardioversion is the tx of choice. If the patient is receiving drugs that promote asystole following electrical cardioversion (e.g. verapamil, beta-blockers, and probably amiodarone) then a temporary pacer should be positioned in the RV before the cardioversion.
- If the ventricular rate during the AFib is not > 200, then you could try procainamide, disopyramide, or quinidine which may prolong the refractory period of the accessory pathway.
Long Term Management
Shown below is an EKG of a 24 years old man with Mahaim type of preexcitation.

Shown below is an EKG of the same patient after Mahaim bundle ablation