Brugada syndrome classification: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
{{Brugada syndrome}} | {{Brugada syndrome}} | ||
{{CMG}} | {{CMG}} | ||
==Overview== | ==Overview== | ||
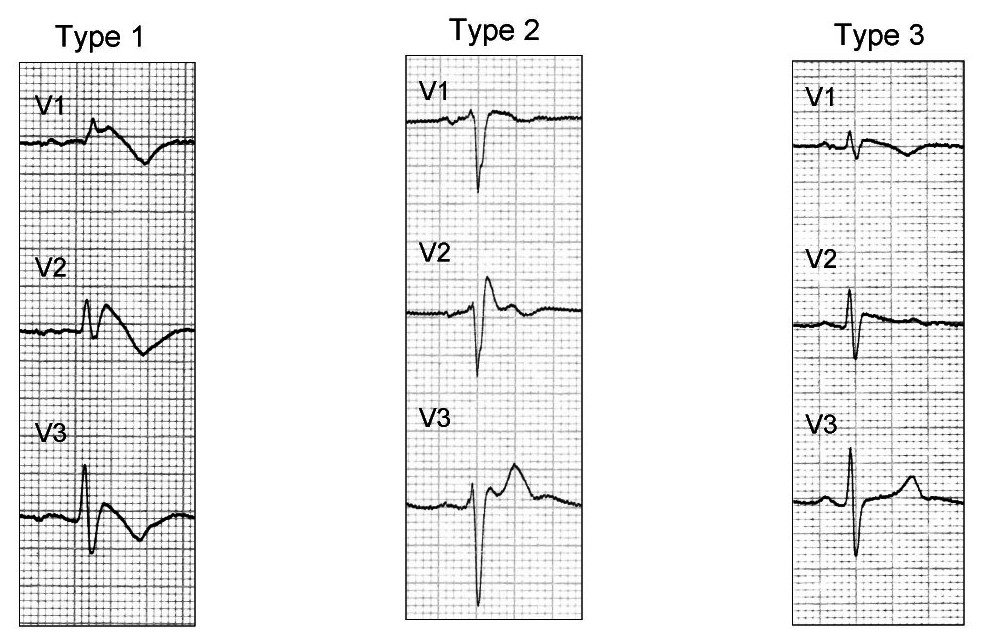
There are three electrocardiographic patterns associated with Brugada syndrome: Type I, Type II and Type III. The diagnosis of Brugada syndrome is based upon the presence of Type I EKG changes. Patients with Type II or Type III Brugada patterns can convert to a Type I Brugada pattern following the administration of sodium channel blockers such as [[ajmaline]] and [[flecainide]]. Type 1 Brugada syndrome may always be present on the EKG, or it may be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels such as [[ajmaline]], [[flecainide]]) or it may be unmasked by various [[Brugada syndrome risk factors|triggers]] or [[Brugada syndrome risk factors|risk factors]]. | There are three electrocardiographic patterns associated with Brugada syndrome: Type I, Type II and Type III. The diagnosis of Brugada syndrome is based upon the presence of Type I EKG changes. Patients with Type II or Type III Brugada patterns can convert to a Type I Brugada pattern following the administration of sodium channel blockers such as [[ajmaline]] and [[flecainide]]. Type 1 Brugada syndrome may always be present on the EKG, or it may be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels such as [[ajmaline]], [[flecainide]]) or it may be unmasked by various [[Brugada syndrome risk factors|triggers]] or [[Brugada syndrome risk factors|risk factors]]. | ||
Revision as of 21:21, 14 October 2012
|
Brugada syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Brugada syndrome classification On the Web |
|
American Roentgen Ray Society Images of Brugada syndrome classification |
|
Risk calculators and risk factors for Brugada syndrome classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
There are three electrocardiographic patterns associated with Brugada syndrome: Type I, Type II and Type III. The diagnosis of Brugada syndrome is based upon the presence of Type I EKG changes. Patients with Type II or Type III Brugada patterns can convert to a Type I Brugada pattern following the administration of sodium channel blockers such as ajmaline and flecainide. Type 1 Brugada syndrome may always be present on the EKG, or it may be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels such as ajmaline, flecainide) or it may be unmasked by various triggers or risk factors.
Type 1 Brugada pattern is characterized by ST elevations in leadsV1-V3 with a right bundle branch block (RBBB). A prolongation of the PR interval is also frequently seen. The EKG changes of Brugada syndrome can vary over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the ST segment elevation, while vagal stimulation worsens it. The administration of class Ia, Ic and III drugs increases the ST segment elevation, as does fever. Exercise decreases ST segment elevation in some patients but increases it in others (after exercise when the body temperature has risen). The changes in heart rate induced by atrial pacing are accompanied by changes in the degree of ST segment elevation. When the heart rate decreases, the ST segment elevation increases and when the heart rate increases the ST segment elevation decreases.
The three patterns of Brugada syndrome (Type I,II,III) are shown below:
The table below is from ECGpedia and is adapted from Wilde et al.[1]
| Type I | Type II | Type III | |
|---|---|---|---|
| J wave amplitude | >= 2mm | >= 2mm | >= 2mm |
| T wave | Negative | Positive or biphasis | Positive |
| ST-T configuration | Coved type | Saddleback | Saddleback |
| ST segment (terminal portion) | Gradually descending | Elevated >= 1mm | Elevated < 1mm |
References
- ↑ Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, Corrado D, Hauer RN, Kass RS, Nademanee K, Priori SG, Towbin JA (2002). "Proposed diagnostic criteria for the Brugada syndrome: consensus report". Circulation. 106 (19): 2514–9. PMID 12417552. Retrieved 2012-10-14. Unknown parameter
|month=ignored (help)