Macrocytic anemia: Difference between revisions
| Line 74: | Line 74: | ||
==[[Macrocytic anemia case study one|Case #1]]== | ==[[Macrocytic anemia case study one|Case #1]]== | ||
==Classification== | ==Classification== | ||
Revision as of 14:34, 21 September 2012
For patient information click here
| Macrocytic anemia | |
 | |
|---|---|
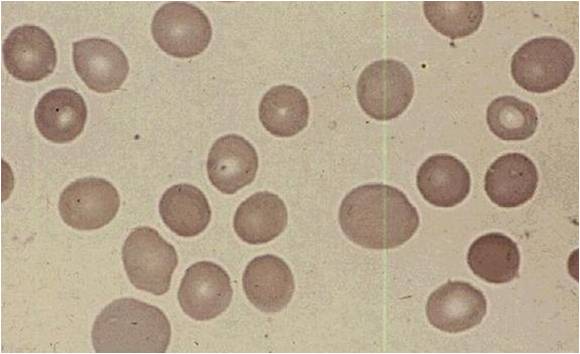
| Megaloblastic anemia blood smear | |
| ICD-10 | D51.1, D52.0, D53.1 |
| ICD-9 | 281 |
| DiseasesDB | 29507 |
| MeSH | D000749 |
|
Macrocytic anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Macrocytic anemia On the Web |
|
American Roentgen Ray Society Images of Macrocytic anemia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Macrocytic anemia from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications and Prognosis
Diagnosis
History and Symptoms
Physical Examination
Laboratory Findings
Electrocardiogram
Chest X Ray
CT
MRI
Echocardiography or Ultrasound
Other Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
Surgery
Primary Prevention
Secondary Prevention
Cost-Effectiveness of Therapy
Future or Investigational Therapies
Case Studies
Case #1
Classification
Megaloblastic anemias (DNA replication disorders)
- Commonest cause of macrocytic anemia.
- In megaloblastic anemias cells are larger because they cannot produce DNA quickly enough to divide at the right time as they grow, and thus grow too large before division.
- Causes for the DNA synthetic problem range from lack of certain vitamins needed to produce DNA (notably folate and B12), to poisons or inhibitors of DNA replication, such as some kinds of antiviral drugs and chemotherapeutic agents.
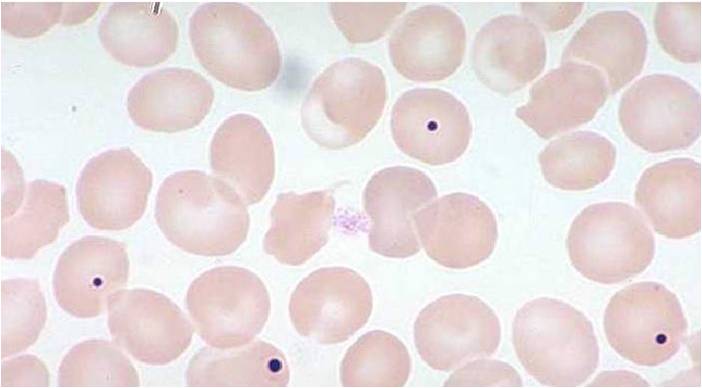
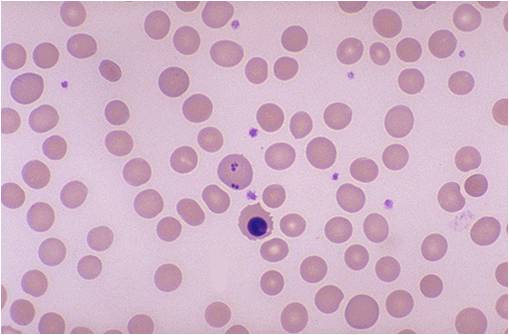
- The pathognomonic findings of megaloblastic anemia are: megaloblasts in bone marrow, ovalocytes in the (peripheral) blood smear, and hypersegmented neutrophils.
Non megaloblastic macrocytic anemias
- Non megaloblastic macrocytic anemias, are disorders associated with increased red cell membrane surface area
- It is commonly associated with pathologies of the liver and spleen which produce codocytes or "target cells" which have a central collection of hemoglobin surrounded by a pallor (a thin area) then followed by a thicker collection of hemoglobin at the rim of the cell.
Alcohol
- Round macrocytes which are not codocytes are produced in chronic alcoholism (which produces a mild macrocytosis even in the absence of vitamin deficiency), apparently as a direct toxic effect of alcohol specifically on the bone marrow.
Association with rapid red cell turnover and reticulocytosis
Mild macrocytocis is a common finding associated with rapid blood restoration or production, since in general, "fresh" or newly-produced red cells (reticulocytes) are larger than the mean (average) size, due to slow shrinkage of normal cells over a normal red cell circulating lifetime. Thus, chronic obstructive pulmonary disease (COPD), in which which red cells are rapidly produced in response to low oxygen levels in the blood, often produces mild macrocytosis. Also, rapid blood replacement from the marrow after a traumatic blood loss, or rapid red blood cell turnover from rapid hemolysis, also often produces mild macrocytosis in the associated anemia. ==Diagnosis==
History and Symptoms
- The major manifestations of Folate or B12 deficiency are related to the anemia and gastrointestinal dysfunction. Only B12 deficiency causes neurologic dysfunction. Constitutional symptoms related to anemia such as fatigue, dyspnea, lightheadedess, and anorexia occur. High output cardiac failure and angina are also consequences.
Symptoms mostly related to GI mucosal abnormalities. Tend to be worse in folate rather than B12 deficiency. Diarrhea, cheilosis and glossitis can be noted.
- The classic picture of B12 deficiency is subacute combined degeneration of the dorsal columns. Specific for B12 deficiency, the patient will present with a broad based gait, ataxic, irritable, forgetful with numbness or paresthesias. Rhomberg and Babinski’s can be noted. Dementia may progress to frank “Megaloblastic Madness”. Remember, hematological abnormalities can occur without neurologic manifestations in B12 deficiency.
Hematological findings
MCV is often >110. Hct can often be as low as 15. Elevated LDH and bilirubin are seen since dyserythopoesis leads to destruction of >90% of RBC precursors. Hypersegmentation of PMNs is quite sensitive (>5% with 5 or more lobes or >1% with 6 lobes). Reticulocyte, WBC and platelets are low to normal. In one series of patients with B12 deficiency, 64% had a MCV greater than 100, and only 29% had anemia. In general the blood film can point towards vitamin deficiency:
- Decreased red blood cell (RBC) count and hemoglobin levels
- Increased mean corpuscular volume (MCV >95 fl often >110) and mean corpuscular hemoglobin (MCH)
- The reticulocyte count is normal
- The platelet count may be reduced.
- Neutrophil granulocytes may show multisegmented nuclei ("senile neutrophil"). This is thought to be due to decreased production and a compensatory prolonged lifespan for circulating neutrophils.
- Anisocytosis (increased variation in RBC size) and poikilocytosis (abnormally shaped RBCs).
- Macrocytes (larger than normal RBCs) are present.
- Ovalocytes (oval shaped RBCs) are present.
- Bone marrow (not normally checked in a patient suspected of megaloblastic anemia) shows megaloblastic hyperplasia.
- Howell-Jolly bodies (chromosomal remnant) also present.
Blood chemistries will also show:
- Increased homocysteine and methylmalonic acid in B12 deficiency
- Increased homocysteine in folate defiency
Analysis
The Schilling test was performed in the past to determine the nature of the vitamin B12 deficiency, but due to the lack of available radioactive B12, it is now largely a historical artifact. Vitamin BTemplate:Ssub is a necessary prosthetic group to the enzyme methylmalonyl-coenzyme A mutase. BTemplate:Ssub deficiency leads to dysfunction of this enzyme and a buildup of its substrate, methylmalonic acid, the elevated level of which can be detected in the urine and blood. Since the level of methylmalonic acid is not elevated in folic acid deficiency, this test provides a one tool in differentiating the two. However, since the test for elevated methylmalonic acid is not specific enough, the gold standard for the diagnosis of B12 deficiency is a low blood level of B12. Unlike the Shilling test, which often included B12 with intrinsic factor, a low level of blood B12 gives no indication as to the etiology of the low B12, which may result from a number of mechanisms.
Treatment
- Folate is administered 1mg QD. Higher doses may be required in malabsorptive syndromes. It is empirically given to those with SCD and those on HD.
- B12 must be given as a load then maintenance. Most advocate 1000 mcg IM Qweek x4 then 100mcg/month.
- LDH falls in 2 days. Hypokalemia requiring replacement can occur in the acute phase as new cells are being generated rapidly.
- A reticulocytosis begins in 3-5 days and peaks in 10 days. The HCT will rise within 10days. If it does not, suspect another disorder. Hypersegmented PMNs disappear in 10-14 days.
- Neurologic abnormalities may take up to 6 months to resolve if ever. The longer the disease has been present, the worse is the prognosis for recovery.
- Persons with PA have a 2x risk of gastric CA (in some studies). Screen for occult blood.
el:Μακροκυτταρική αναιμία sq:Anemi makrocitike
References
gl:Anemia megaloblástica he:אנמיה מגלובלסטית it:Anemia megaloblastica sl:Megaloblastna anemija sr:Мегалобластна анемија