Pancreas divisum: Difference between revisions
| Line 80: | Line 80: | ||
==References== | ==References== | ||
{{reflist}} | {{reflist}} | ||
==See Also== | |||
*[[Anomalous pancreaticobiliary junction]] | |||
*[[Annular pancreas]] | |||
==External links== | ==External links== | ||
Revision as of 18:57, 15 March 2009
| Pancreas divisum | |
| ICD-10 | Q45.3 |
|---|---|
| ICD-9 | 751.7 |
| DiseasesDB | 31894 |
| MedlinePlus | 000247 |
| eMedicine | radio/520 |
|
WikiDoc Resources for Pancreas divisum |
|
Articles |
|---|
|
Most recent articles on Pancreas divisum Most cited articles on Pancreas divisum |
|
Media |
|
Powerpoint slides on Pancreas divisum |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Pancreas divisum at Clinical Trials.gov Trial results on Pancreas divisum Clinical Trials on Pancreas divisum at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pancreas divisum NICE Guidance on Pancreas divisum
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pancreas divisum Discussion groups on Pancreas divisum Patient Handouts on Pancreas divisum Directions to Hospitals Treating Pancreas divisum Risk calculators and risk factors for Pancreas divisum
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pancreas divisum |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Contributors: Cafer Zorkun M.D., PhD.
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Pancreas or Pancreatic divisum is a congenital anomaly in the anatomy of the ducts of the pancreas in which a single pancreatic duct is not formed, but rather remains as two distinct dorsal and ventral ducts.
- Variant of the pancreatic ductal system and occurs in 4%–10% of the population.
- Dorsal and ventral anlagen of the pancreas fail to fuse.
- The dorsal duct drains most of the glandular parenchyma through the minor papilla
- The smaller ventral duct drains a portion of the pancreatic head, including the uncinate process, through the major papilla.
- Clinical relevance of pancreas divisum remains controversial.
- Most patients with pancreas divisum are asymptomatic.
- In some patients, this anomaly is associated with recurrent episodes of pancreatitis.
- Postulated that in pancreas divisum, the duct of Santorini and the minor ampulla are too small to adequately drain the secretions produced by the pancreatic body and tail.
Causes
The human embryo begins life with two ducts in the pancreas, these are the ventral duct and the dorsal duct. Normally, the two ducts will fuse together to form one main pancreatic duct; this occurs in more than 90% of embryos. In approximately 10% of embryos the ventral and dorsal ducts fail to fuse together, resulting in pancreas divisum. In utero, the majority of the pancreas is drained by the dorsal duct which opens up into the minor papilla. The ventral duct drains the minority of the pancreas and opens into the major papilla. In adults however, this situation is reversed whereby 70% of the pancreas is drained by the ventral duct. Therefore in pancreas divisum, where fusion of the ducts does not occur, the major drainage of the pancreas is done by the dorsal duct which opens up into the minor papilla.
This is the embryologic progression of the pancreas formation. The 4th picture is a normal pancreas. The duct of santorini or minor papilla was closed and the dorsal pancreas drains into the ventral duct. In pancreas divisum, the last step (4th picture) does not happen. The pancreas formation is halted at the 3rd picture.
Symptoms
A majority of individuals born with pancreas divisum will never have symptoms for their entire life. In most cases, pancreas divisum is only detected during an autopsy of a person that is deceased. However, approximately 1% of those with pancreas divisum will develop symptoms during their lifetime. Symptoms commonly include abdominal pain, nausea and/or vomiting, and pancreatitis. A small number of individuals may develop chronic pancreatitis.
Diagnosis
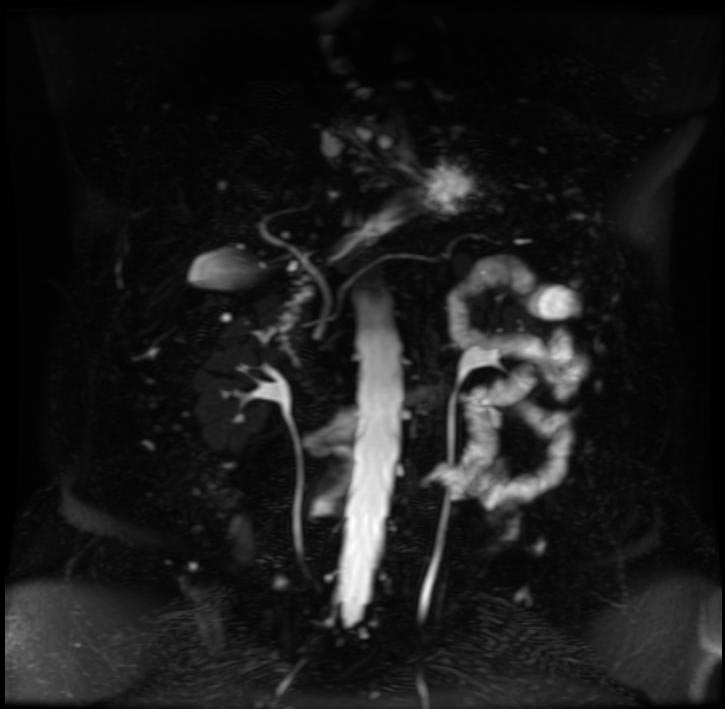
The most common and accurate way of diagnosing an individual with this anomaly is by an ERCP. This test can demonstrate the presence of two separately draining ducts within the pancreas. Other tests can assist doctors with diagnosis, such as a CT scan and an MRI.
Diagnostic Findings
- The dorsal duct drains most of the glandular parenchyma through the minor papilla
- The smaller ventral duct drains a portion of the pancreatic head, including the uncinate process, through the major papilla.
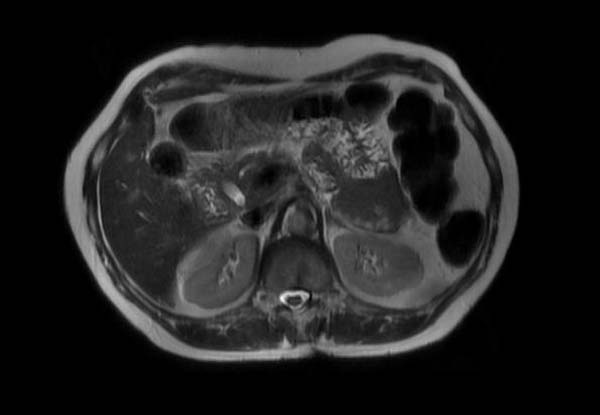
Patient #1
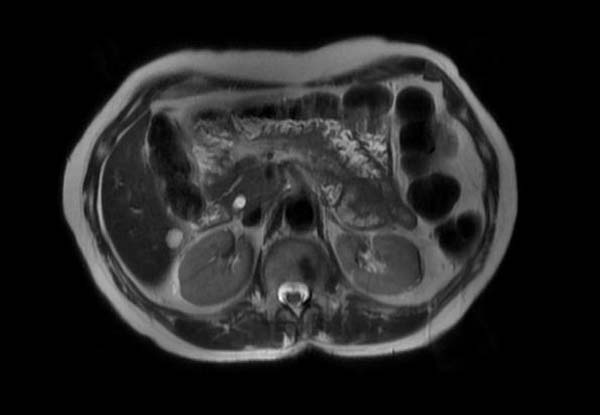
Patient #2
-
MRCP
Treatment
Pancreas Divisum in individuals with no symptoms do not need treatment. Treatment of those with symptoms varies and has not been very well established. A surgeon may attempt a sphincterotomy by cutting the minor papilla to enlarge the opening and allow pancreas enzymes to flow normally. During surgery, a stent may be inserted into the duct to ensure that the duct will not close causing a blockage. As with any surgery, this operation is not risk-free. This surgery can cause pancreatitis in patients, or in rare cases, kidney failure and death.
An association with adenoma of the minor papilla has been reported.[1]
References
See Also
External links
Template:Congenital malformations and deformations of digestive system Template:SIB de:Pankreas divisum