Tuberculosis historical perspective: Difference between revisions
Mashal Awais (talk | contribs) |
Mohamed riad (talk | contribs) |
||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
[[Tuberculosis]] has been present in humans since ancient times. The earliest unambiguous detection of ''[[Mycobacterium tuberculosis]]'' was in the remains of bison, dated 18,000 BC.<ref name=Rothschild_2001>{{cite journal |author=Rothschild B, Martin L, Lev G, Bercovier H, Bar-Gal G, Greenblatt C, Donoghue H, Spigelman M, Brittain D |title=Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present |journal=Clin Infect Dis |volume=33 |issue=3 |pages=305-11 |year=2001 | pmid = 11438894}}</ref> However, whether [[tuberculosis]] originated in cattle and then transferred to humans, or diverged from a common ancestor, is unclear.<ref name=Pearce-Duvet_2006>{{cite journal |author=Pearce-Duvet J |title=The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease |journal=Biol Rev Camb Philos Soc |volume=81 |issue=3 |pages=369-82 |year=2006 | pmid = 16672105}}</ref> Through history [[tuberculosis]] has had many names including ''phthisis'' and ''Wasting disease'', which were mostly derived from its [[symptoms]]. The ''[[Mycobacterium tuberculosis]]'' was only identified in 1882 by [[Robert Koch]]. In the 19th and early 20th centuries, [[tuberculosis]] caused the most widespread public concern, which is considered an endemic disease of the urban poor. It was only in 1946, with the development of the [[antibiotic]] [[streptomycin]], that effective treatment and cure became possible. Since the rise of [[Antibiotic resistant|drug-resistant]] strains in the 1980s, hopes that the disease could be completely eliminated have been dashed. | [[Tuberculosis]] has been present in humans since ancient times. The earliest unambiguous detection of ''[[Mycobacterium tuberculosis]]'' was in the remains of bison, dated 18,000 BC.<ref name="Rothschild_2001">{{cite journal |author=Rothschild B, Martin L, Lev G, Bercovier H, Bar-Gal G, Greenblatt C, Donoghue H, Spigelman M, Brittain D |title=Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present |journal=Clin Infect Dis |volume=33 |issue=3 |pages=305-11 |year=2001 | pmid = 11438894}}</ref> However, whether [[tuberculosis]] originated in cattle and then transferred to humans, or diverged from a common ancestor, is unclear.<ref name="Pearce-Duvet_2006">{{cite journal |author=Pearce-Duvet J |title=The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease |journal=Biol Rev Camb Philos Soc |volume=81 |issue=3 |pages=369-82 |year=2006 | pmid = 16672105}}</ref> Through history [[tuberculosis]] has had many names including ''phthisis'' and ''Wasting disease'', which were mostly derived from its [[symptoms]]. The ''[[Mycobacterium tuberculosis]]'' was only identified in 1882 by [[Robert Koch]]. In the 19th and early 20th centuries, [[tuberculosis]] caused the most widespread public concern, which is considered an endemic disease of the urban poor. It was only in 1946, with the development of the [[antibiotic]] [[streptomycin]], that effective treatment and cure became possible. Since the rise of [[Antibiotic resistant|drug-resistant]] strains in the 1980s, hopes that the disease could be completely eliminated have been dashed. | ||
==Historical Perspective== | ==Historical Perspective== | ||
[[Image:TB history 1.png|left|thumb|400px|Tubercular decay has been found in the spines of Egyptian mummies. Pictured: Egyptian mummy in the British Museum<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:Mummy_at_British_Museum.jpg | [[Image:TB history 1.png|left|thumb|400px|Tubercular decay has been found in the spines of Egyptian mummies. Pictured: Egyptian mummy in the British Museum<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:Mummy_at_British_Museum.jpg Adapted from Wikimedia Commons]''<ref name="Wikimedia Commons">{{Cite web | title = Wikimedia Commons | url = http://commons.wikimedia.org/wiki/File:Mummy_at_British_Museum.jpg}}</ref></SMALL></SMALL>]] | ||
Prehistoric humans –evidenced by skeletal remains- (4000 BC) were infected with TB, in addition to the spines of mummies showing tubercular decay from 3000-2400 BC.<ref name="Zink_2003">{{cite journal |author=Zink A, Sola C, Reischl U, Grabner W, Rastogi N, Wolf H, Nerlich A |title=Characterization of Mycobacterium tuberculosis complex DNAs from Egyptian mummies by spoligotyping |journal=J Clin Microbiol |volume=41 |issue=1 |pages=359-67 |year=2003 | pmid = 12517873}}</ref> Phthisis is a Greek term for [[tuberculosis]]; around 460 BC. In terms of Hippocrates point of view, phthisis was the most widespread disease of the time involving fever and coughing up blood, which was almost always fatal.<ref>Hippocrates. [http://web.archive.org/web/20050211173218/http://classics.mit.edu/Hippocrates/aphorisms.mb.txt Aphorisms.] Accessed 07 October 2006.</ref> TB was present in South America for about 2,000 years evidenced by some genetic studies.<ref name="Konomi_2002">{{cite journal |author=Konomi N, Lebwohl E, Mowbray K, Tattersall I, Zhang D |title=Detection of mycobacterial DNA in Andean mummies |journal=J Clin Microbiol |volume=40 |issue=12 |pages=4738–40 |year=2002 | pmid = 12454182}}</ref> In South America, the earliest evidence of [[tuberculosis]] was linked to the Paracas-Caverna culture (circa 750 BC to circa 100 AD).<ref>[http://memorias.ioc.fiocruz.br/98sup/6psa.html "South America: Prehistoric Findings"]. ''Memorias do Instituto Oswaldo Cruz'', Vol. 98 (Suppl.I) January 2003. Retrieved on [[2007-02-08]].</ref> | |||
Previously, tuberculosis was named consumption, because it was like consumption of the affected people from within, with fever, bloody cough, pallor, and severe wasting. Other names are:<ref name="Britannica1911">[http://www.1911encyclopedia.org/Tuberculosis Tuberculosis] ''Encyclopedia Britannica,'' 11th ed.</ref><ref>[http://www.antiquusmorbus.com/English/English.htm Rudy's List of Archaic Medical Terms] English Glossary of Archaic Medical Terms, Diseases and Causes of Death. Accessed 09 Oct 06</ref><ref name="Britannica1911" /><ref>[http://www.nlm.nih.gov/medlineplus/ency/article/000624.htm Disseminated tuberculosis] NIH Medical Encyclopedia. Accessed 09 Oct 06</ref> | |||
* ''Phthisis'' (Greek for consumption) | |||
* ''Phthisis pulmonalis'' | *''Phthisis'' (Greek for consumption) | ||
* ''[[Scrofula]]'' (in adults) - affecting the | *''Phthisis pulmonalis'' | ||
* ''Tabes mesenterica'' - [[TB]] of the [[abdomen]] | *''[[Scrofula]]'' (in adults) - affecting the lymphatic system, resulting in swollen cervical lymph nodes | ||
* ''[[Lupus vulgaris]]'' - [[TB]] of the [[skin]] | *''Tabes mesenterica'' - [[TB]] of the [[abdomen]] | ||
* ''Wasting disease'' | *''[[Lupus vulgaris]]'' - [[TB]] of the [[skin]] | ||
* ''White plague'' - because sufferers appeared markedly pale | *''Wasting disease'' | ||
* ''King's evil'' - | *''White plague'' - because sufferers appeared markedly pale | ||
* ''[[Pott's disease]]'' | *''King's evil'' - as people had a false belief that that scrofula would heal by the king’s touch | ||
* [[Miliary tuberculosis]] – now commonly known as ''[[disseminated TB]]'', occurs when the [[infection]] invades the | *''[[Pott's disease]]'' - TB of the spine | ||
*[[Miliary tuberculosis]] – now commonly known as ''[[disseminated TB]]'', occurs when the [[infection]] invades the blood stream, resulting in lesions with the appearance of millet seeds on [[x-ray]]. | |||
===Folklore=== | ===Folklore=== | ||
Before the industrial revolution, [[tuberculosis]] may sometimes have been regarded as vampirism. When one member of a family died from it, the other members that were [[infected]] would lose their health slowly. People believed that this was caused by the original victim draining the life from the other family members. Furthermore, people who had [[TB]] exhibited [[symptoms]] similar to what people considered to be vampire traits. People with [[TB]] often have [[symptoms]] such as red, swollen [[red eye|eyes]] (which also creates a sensitivity to bright light), pale [[skin]] and [[coughing blood]]. This suggested the idea that the only way for the afflicted to replenish this loss of [[blood]] was by sucking [[blood]].<ref name=Sledzik_1994>{{cite journal |author=Sledzik P, Bellantoni N |title=Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief |journal=Am J Phys Anthropol |volume=94 |issue=2 |pages=269-74 |year=1994 |url=http://users.net1plus.com/vyrdolak/tableone.htm | pmid = 8085617}}</ref> Another folk belief attributed it to being forced, nightly, to attend fairy revels, so that the victim wasted away owing to lack of rest; this belief was most common when a strong connection was seen between the fairies and the dead.<ref name=Briggs>[[Katharine Mary Briggs|Katharine Briggs]], ''An Encyclopedia of Fairies'' "Consumption" ([[Pantheon Books]], 1976) p. 80. ISBN 0-394-73467-X</ref> Similarly, but less commonly, it was attributed to the victims being 'hagridden' - being transformed into horses by witches (hags) to travel to their nightly meetings, again resulting in a lack of rest.<ref name=Briggs/> | Before the industrial revolution, [[tuberculosis]] may sometimes have been regarded as vampirism. When one member of a family died from it, the other members that were [[infected]] would lose their health slowly. People believed that this was caused by the original victim draining the life from the other family members. Furthermore, people who had [[TB]] exhibited [[symptoms]] similar to what people considered to be vampire traits. People with [[TB]] often have [[symptoms]] such as red, swollen [[red eye|eyes]] (which also creates a sensitivity to bright light), pale [[skin]] and [[coughing blood]]. This suggested the idea that the only way for the afflicted to replenish this loss of [[blood]] was by sucking [[blood]].<ref name="Sledzik_1994">{{cite journal |author=Sledzik P, Bellantoni N |title=Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief |journal=Am J Phys Anthropol |volume=94 |issue=2 |pages=269-74 |year=1994 |url=http://users.net1plus.com/vyrdolak/tableone.htm | pmid = 8085617}}</ref> Another folk belief attributed it to being forced, nightly, to attend fairy revels, so that the victim wasted away owing to lack of rest; this belief was most common when a strong connection was seen between the fairies and the dead.<ref name="Briggs">[[Katharine Mary Briggs|Katharine Briggs]], ''An Encyclopedia of Fairies'' "Consumption" ([[Pantheon Books]], 1976) p. 80. ISBN 0-394-73467-X</ref> Similarly, but less commonly, it was attributed to the victims being 'hagridden' - being transformed into horses by witches (hags) to travel to their nightly meetings, again resulting in a lack of rest.<ref name="Briggs" /> | ||
[[TB]] was romanticized in the nineteenth century. Many at the time believed [[TB]] produced feelings of euphoria referred to as 'Spes phthisica' or 'hope of the consumptive'. It was believed that [[TB]] sufferers who were artists had bursts of creativity as the disease progressed. It was also believed that [[TB]] sufferers acquired a final burst of energy just before they died which made women more beautiful and men more creative.<ref name="StudiesLiteraryImagination-Clark">Lawlor, Clark. "Transatlantic Consumptions: Disease, Fame and Literary Nationalism in the Davidson Sisters, Southey, and Poe". ''Studies in the Literary Imagination'', Fall 2003. Available at [http://findarticles.com/p/articles/mi_qa3822/is_200310/ai_n9310101 findarticles.com.] Retrieved on [[2007-06-08]].</ref> | [[TB]] was romanticized in the nineteenth century. Many at the time believed [[TB]] produced feelings of euphoria referred to as 'Spes phthisica' or 'hope of the consumptive'. It was believed that [[TB]] sufferers who were artists had bursts of creativity as the disease progressed. It was also believed that [[TB]] sufferers acquired a final burst of energy just before they died which made women more beautiful and men more creative.<ref name="StudiesLiteraryImagination-Clark">Lawlor, Clark. "Transatlantic Consumptions: Disease, Fame and Literary Nationalism in the Davidson Sisters, Southey, and Poe". ''Studies in the Literary Imagination'', Fall 2003. Available at [http://findarticles.com/p/articles/mi_qa3822/is_200310/ai_n9310101 findarticles.com.] Retrieved on [[2007-06-08]].</ref> | ||
===Study and Treatment=== | ===Study and Treatment=== | ||
[[Image:TB history 2.png|left|thumb|200px|Dr. Robert Koch discovered the tuberculosis bacilli.<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:RobertKoch.jpg | [[Image:TB history 2.png|left|thumb|200px|Dr. Robert Koch discovered the tuberculosis bacilli.<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:RobertKoch.jpg Adapted from Wikimedia Commons]''<ref name="Wikimedia Commons">{{Cite web | title = Wikimedia Commons | url = http://commons.wikimedia.org/wiki/File:RobertKoch.jpg}}</ref></SMALL></SMALL>]]The study of [[tuberculosis]] dates back to ''[[The Canon of Medicine]]'' written by [[Avicenna|Ibn Sina]] (Avicenna) in the 1020s. He was the first physician to identify [[pulmonary tuberculosis]] as a [[Infectious disease|contagious disease]] and suggest that it could spread through contact with soil and [[water]].<ref>Y. A. Al-Sharrah (2003), "The Arab Tradition of Medical Education and its Relationship with the European Tradition", ''Prospects'' '''33''' (4), [[Springer Science+Business Media|Springer]].</ref><ref>[[George Sarton]], ''Introduction to the History of Science''. <br> ([[cf.]] Dr. A. Zahoor and Dr. Z. Haq (1997). [http://www.cyberistan.org/islamic/Introl1.html Quotations From Famous Historians of Science], Cyberistan.)</ref> He developed the method of [[quarantine]] in order to limit the spread of [[tuberculosis]].<ref>David W. Tschanz, MSPH, PhD (August 2003). "Arab Roots of European Medicine", ''Heart Views'' '''4''' (2).</ref> | ||
Although it was established that the [[pulmonary]] form was associated with 'tubercles' by [[Dr Richard Morton]] in 1689,<ref name="WhoNamedIt-Calmette">Who Named It? [http://www.whonamedit.com/doctor.cfm/2413.html Léon Charles Albert Calmette.] Retrieved on 6 October 2006.</ref><ref name="MedHist1970-Trail">{{cite journal |author=Trail R |title=Richard Morton (1637–1698) |journal=Med Hist |volume=14 |issue=2 |pages=166-74 |year=1970 | pmid = 4914685}}</ref> due to the variety of its [[symptoms]], [[TB]] was not identified as a single disease until the 1820s and was not named '[[tuberculosis]]' until 1839 by [[Johann Lukas Schönlein|J. L. Schönlein]].<ref>Zur Pathogenie der Impetigines. Auszug aus einer brieflichen Mitteilung an den Herausgeber. [Müller’s] ''Archiv für Anatomie, Physiologie und wissenschaftliche Medicin''. 1839, page 82.</ref> During the years 1838-1845, Dr. John Croghan, the owner of Mammoth Cave, brought a number of [[tuberculosis]] sufferers into the cave in the hope of curing the disease with the constant temperature and purity of the cave air: they died within a year.<ref>[http://edition.cnn.com/2004/TRAVEL/DESTINATIONS/02/26/mammoth.cave.ap/index.html Kentucky: Mammoth Cave long on history.] ''[[CNN]]''. 27 February 2004. Accessed 08 October 2006.</ref> The first [[TB]] [[sanatorium]] opened in 1859 in Görbersdorf, Germany (today Sokołowsko, Poland) by Hermann Brehmer.<ref name =sanatoria>{{cite journal |author=McCarthy OR |title=The key to the sanatoria |journal=J R Soc Med |volume=94 |issue=8 |pages=413-7 |year=2001 | pmid = 11461990}}</ref> | Although it was established that the [[pulmonary]] form was associated with 'tubercles' by [[Dr Richard Morton]] in 1689,<ref name="WhoNamedIt-Calmette">Who Named It? [http://www.whonamedit.com/doctor.cfm/2413.html Léon Charles Albert Calmette.] Retrieved on 6 October 2006.</ref><ref name="MedHist1970-Trail">{{cite journal |author=Trail R |title=Richard Morton (1637–1698) |journal=Med Hist |volume=14 |issue=2 |pages=166-74 |year=1970 | pmid = 4914685}}</ref> due to the variety of its [[symptoms]], [[TB]] was not identified as a single disease until the 1820s and was not named '[[tuberculosis]]' until 1839 by [[Johann Lukas Schönlein|J. L. Schönlein]].<ref>Zur Pathogenie der Impetigines. Auszug aus einer brieflichen Mitteilung an den Herausgeber. [Müller’s] ''Archiv für Anatomie, Physiologie und wissenschaftliche Medicin''. 1839, page 82.</ref> During the years 1838-1845, Dr. John Croghan, the owner of Mammoth Cave, brought a number of [[tuberculosis]] sufferers into the cave in the hope of curing the disease with the constant temperature and purity of the cave air: they died within a year.<ref>[http://edition.cnn.com/2004/TRAVEL/DESTINATIONS/02/26/mammoth.cave.ap/index.html Kentucky: Mammoth Cave long on history.] ''[[CNN]]''. 27 February 2004. Accessed 08 October 2006.</ref> The first [[TB]] [[sanatorium]] opened in 1859 in Görbersdorf, Germany (today Sokołowsko, Poland) by Hermann Brehmer.<ref name="sanatoria">{{cite journal |author=McCarthy OR |title=The key to the sanatoria |journal=J R Soc Med |volume=94 |issue=8 |pages=413-7 |year=2001 | pmid = 11461990}}</ref> | ||
In regard to this claim, ''The Times'' for January 15, 1859, page 5, column 5, carries an advertisement seeking funds for the Bournemouth Sanatorium for Consumption, referring to the balance sheet for the past year, and offering an annual report to prospective donors, implying that this [[sanatorium]] was in existence at least in 1858. The [[bacillus]] causing [[tuberculosis]], ''[[Mycobacterium tuberculosis]]'', was identified and described on March 24, 1882 by [[Robert Koch]]. He received the [[Nobel Prize in physiology or medicine]] in 1905 for this discovery.<ref>[[Nobel Foundation]]. [http://nobelprize.org/nobel_prizes/medicine/laureates/1905/ The Nobel Prize in Physiology or Medicine 1905.] Accessed 07 October 2006.</ref> Koch did not believe that bovine (cattle) and human [[tuberculosis]] were similar, which delayed the recognition of [[infected]] milk as a source of [[infection]]. Later, this source was eliminated by the [[pasteurization]] process. Koch announced a [[glycerine]] extract of the tubercle [[bacilli]] as a remedy for [[tuberculosis]] in 1890, calling it 'tuberculin'. It was not effective, but was later adapted as a test for pre-symptomatic [[tuberculosis]].<ref name=Waddington_2004>{{cite journal |author=Waddington K |title=To stamp out "so terrible a malady": bovine tuberculosis and tuberculin testing in Britain, 1890–1939 |journal=Med Hist |volume=48 |issue=1 |pages=29–48 |year=2004 | pmid = 14968644}}</ref> | In regard to this claim, ''The Times'' for January 15, 1859, page 5, column 5, carries an advertisement seeking funds for the Bournemouth Sanatorium for Consumption, referring to the balance sheet for the past year, and offering an annual report to prospective donors, implying that this [[sanatorium]] was in existence at least in 1858. The [[bacillus]] causing [[tuberculosis]], ''[[Mycobacterium tuberculosis]]'', was identified and described on March 24, 1882 by [[Robert Koch]]. He received the [[Nobel Prize in physiology or medicine]] in 1905 for this discovery.<ref>[[Nobel Foundation]]. [http://nobelprize.org/nobel_prizes/medicine/laureates/1905/ The Nobel Prize in Physiology or Medicine 1905.] Accessed 07 October 2006.</ref> Koch did not believe that bovine (cattle) and human [[tuberculosis]] were similar, which delayed the recognition of [[infected]] milk as a source of [[infection]]. Later, this source was eliminated by the [[pasteurization]] process. Koch announced a [[glycerine]] extract of the tubercle [[bacilli]] as a remedy for [[tuberculosis]] in 1890, calling it 'tuberculin'. It was not effective, but was later adapted as a test for pre-symptomatic [[tuberculosis]].<ref name="Waddington_2004">{{cite journal |author=Waddington K |title=To stamp out "so terrible a malady": bovine tuberculosis and tuberculin testing in Britain, 1890–1939 |journal=Med Hist |volume=48 |issue=1 |pages=29–48 |year=2004 | pmid = 14968644}}</ref> | ||
The first genuine success in immunizing against [[tuberculosis]] was developed from attenuated bovine-strain [[tuberculosis]] by [[Albert Calmette]] and [[Camille Guerin]] in 1906. It was called 'BCG' ([[Bacillus Calmette-Guérin|Bacillus of Calmette and Guerin]]). The [[BCG vaccine]] was first used on humans in 1921 in France, but it wasn't until after World War II that [[BCG]] received widespread acceptance in the USA, Great Britain, and Germany. | The first genuine success in immunizing against [[tuberculosis]] was developed from attenuated bovine-strain [[tuberculosis]] by [[Albert Calmette]] and [[Camille Guerin]] in 1906. It was called 'BCG' ([[Bacillus Calmette-Guérin|Bacillus of Calmette and Guerin]]). The [[BCG vaccine]] was first used on humans in 1921 in France, but it wasn't until after World War II that [[BCG]] received widespread acceptance in the USA, Great Britain, and Germany. | ||
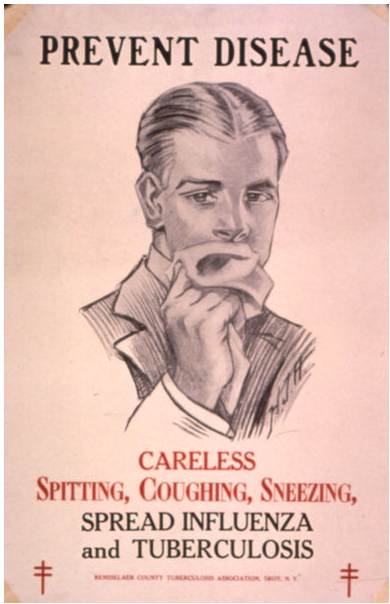
[[Tuberculosis]], or 'consumption' as it was commonly known, caused the most widespread public concern in the 19th and early 20th centuries as an [[endemic (epidemiology)|endemic]] disease of the urban poor. In 1815, one in four deaths in England was of consumption; by 1918 one in six deaths in France were still caused by [[TB]]. In the 20th century, [[tuberculosis]] killed an estimated 100 million people.<ref>[http://birdflubook.com/a.php?id=40&t=p Torrey EF and Yolken RH. 2005. Their bugs are worse than their bite. Washington Post, April 3, p. B01.]</ref> After the establishment in the 1880s that the disease was [[contagious]], [[TB]] was made a [[List of notifiable diseases|notifiable disease]] in Britain; there were campaigns to stop spitting in public places, and the [[infected]] poor were encouraged to enter [[sanatorium|sanatoria]] that resembled prisons; the [[sanatorium|sanatoria]] for the middle and upper classes offered excellent care and constant medical attention.<ref name =sanatoria/> Whatever the purported benefits of the fresh air and labor in the [[sanatorium|sanatoria]], even under the best conditions, 50% of those who entered were dead within five years (1916).<ref name =sanatoria/> | [[Tuberculosis]], or 'consumption' as it was commonly known, caused the most widespread public concern in the 19th and early 20th centuries as an [[endemic (epidemiology)|endemic]] disease of the urban poor. In 1815, one in four deaths in England was of consumption; by 1918 one in six deaths in France were still caused by [[TB]]. In the 20th century, [[tuberculosis]] killed an estimated 100 million people.<ref>[http://birdflubook.com/a.php?id=40&t=p Torrey EF and Yolken RH. 2005. Their bugs are worse than their bite. Washington Post, April 3, p. B01.]</ref> After the establishment in the 1880s that the disease was [[contagious]], [[TB]] was made a [[List of notifiable diseases|notifiable disease]] in Britain; there were campaigns to stop spitting in public places, and the [[infected]] poor were encouraged to enter [[sanatorium|sanatoria]] that resembled prisons; the [[sanatorium|sanatoria]] for the middle and upper classes offered excellent care and constant medical attention.<ref name="sanatoria" /> Whatever the purported benefits of the fresh air and labor in the [[sanatorium|sanatoria]], even under the best conditions, 50% of those who entered were dead within five years (1916).<ref name="sanatoria" /> | ||
[[Image:TB history 3.png|left|thumb|200px|Public health campaigns tried to halt the spread of TB<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:TB_poster.jpg | [[Image:TB history 3.png|left|thumb|200px|Public health campaigns tried to halt the spread of TB<SMALL><SMALL>''[http://commons.wikimedia.org/wiki/File:TB_poster.jpg Adapted from Wikimedia Commons]''<ref name="Wikimedia Commons">{{Cite web | title = Wikimedia Commons | url = http://commons.wikimedia.org/wiki/File:TB_poster.jpg}}</ref></SMALL></SMALL>]] | ||
The promotion of [[Christmas Seals]] began in Denmark during 1904, as a way to raise money for [[tuberculosis]] programs. It expanded to the United States and Canada in 1907–08 to help the National Tuberculosis Association (later called the [[American Lung Association]]). | The promotion of [[Christmas Seals]] began in Denmark during 1904, as a way to raise money for [[tuberculosis]] programs. It expanded to the United States and Canada in 1907–08 to help the National Tuberculosis Association (later called the [[American Lung Association]]). | ||
| Line 46: | Line 47: | ||
In Europe, deaths from [[TB]] fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in [[public health]] were reducing [[tuberculosis]] even before the arrival of [[antibiotics]], although the disease remained a significant threat to [[public health]]. When the [[Medical Research Council (UK)|Medical Research Council]] was formed in Britain in 1913 its initial focus was [[tuberculosis]] research.<ref>[[Medical Research Council (UK)|]]. [http://www.mrc.ac.uk/YourHealth/StoriesDiscovery/Tuberculosis/index.htm MRC's contribution to Tuberculosis research.] Accessed 02 July 2007.</ref> | In Europe, deaths from [[TB]] fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in [[public health]] were reducing [[tuberculosis]] even before the arrival of [[antibiotics]], although the disease remained a significant threat to [[public health]]. When the [[Medical Research Council (UK)|Medical Research Council]] was formed in Britain in 1913 its initial focus was [[tuberculosis]] research.<ref>[[Medical Research Council (UK)|]]. [http://www.mrc.ac.uk/YourHealth/StoriesDiscovery/Tuberculosis/index.htm MRC's contribution to Tuberculosis research.] Accessed 02 July 2007.</ref> | ||
It was not until 1946 with the development of the [[antibiotic]] [[streptomycin]] that effective treatment and cure became possible. Prior to the introduction of this drug, the only treatment besides [[sanatorium|sanatoria]] were [[surgical]] interventions, including the [[pneumothorax]] technique - collapsing an [[infected]] [[lung]] to rest it and allow lesions to heal - a technique that was of little benefit and was largely discontinued by the 1950s.<ref name=Wolfart_1990>{{cite journal |author=Wolfart W |title=[Surgical treatment of tuberculosis and its modifications—collapse therapy and resection treatment and their present-day sequelae] |journal=Offentl Gesundheitswes |volume=52 |issue=8–9 |pages=506-11 |year=1990 | pmid = 2146567}}</ref> The emergence of [[multidrug-resistant TB]] has again introduced surgery as part of the treatment for these [[infections]]. Here, [[surgical]] removal of [[lung]] cavities will reduce the number of [[bacteria]] in the [[lungs]], as well as increase the exposure of the remaining [[bacteria]] to drugs in the [[bloodstream]], which is thought to increase the effectiveness of the [[chemotherapy]].<ref name=Lalloo_2006>{{cite journal |author=Lalloo U, Naidoo R, Ambaram A |title=Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis |journal=Curr Opin Pulm Med |volume=12 |issue=3 |pages=179-85 |year=2006 | pmid = 16582672}}</ref> | It was not until 1946 with the development of the [[antibiotic]] [[streptomycin]] that effective treatment and cure became possible. Prior to the introduction of this drug, the only treatment besides [[sanatorium|sanatoria]] were [[surgical]] interventions, including the [[pneumothorax]] technique - collapsing an [[infected]] [[lung]] to rest it and allow lesions to heal - a technique that was of little benefit and was largely discontinued by the 1950s.<ref name="Wolfart_1990">{{cite journal |author=Wolfart W |title=[Surgical treatment of tuberculosis and its modifications—collapse therapy and resection treatment and their present-day sequelae] |journal=Offentl Gesundheitswes |volume=52 |issue=8–9 |pages=506-11 |year=1990 | pmid = 2146567}}</ref> The emergence of [[multidrug-resistant TB]] has again introduced surgery as part of the treatment for these [[infections]]. Here, [[surgical]] removal of [[lung]] cavities will reduce the number of [[bacteria]] in the [[lungs]], as well as increase the exposure of the remaining [[bacteria]] to drugs in the [[bloodstream]], which is thought to increase the effectiveness of the [[chemotherapy]].<ref name="Lalloo_2006">{{cite journal |author=Lalloo U, Naidoo R, Ambaram A |title=Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis |journal=Curr Opin Pulm Med |volume=12 |issue=3 |pages=179-85 |year=2006 | pmid = 16582672}}</ref> | ||
Hopes that the disease could be completely eliminated have been dashed since the rise of [[Antibiotic resistant|drug-resistant]] strains in the 1980s. For example, [[tuberculosis]] cases in Britain, numbering around 117,000 in 1913, had fallen to around 5,000 in 1987, but cases rose again, reaching 6,300 in 2000 and 7,600 cases in 2005.<ref>{{cite web | url =http://www.hpa.org.uk/infections/topics_AZ/tb/epidemiology/table1.htm | title = Tuberculosis – Respiratory and Non-respiratory Notifications, England and Wales, 1913-2005 | publisher = Health Protection Agency Centre for Infections | date = 21 March 2007 | accessdate = 2007-08-01}}</ref> Due to the elimination of [[public health]] facilities in New York and the emergence of [[HIV]], there was a resurgence in the late 1980s.<ref name=Paolo_2004>{{cite journal |author=Paolo W, Nosanchuk J |title=Tuberculosis in New York city: recent lessons and a look ahead |journal=Lancet Infect Dis |volume=4 |issue=5 |pages=287-93 |year=2004 | pmid = 15120345}}</ref> The number of those failing to complete their course of drugs is high. NY had to cope with more than 20,000 unnecessary [[TB]]-patients with [[Multidrug resistance|multidrug-resistant]] strains (resistant to, at least, both [[Rifampin]] and [[Isoniazid]] . The resurgence of [[tuberculosis]] resulted in the declaration of a global health emergency by the [[World Health Organization]] in 1993.<ref>[[World Health Organization]] (WHO). [http://www.who.int/tb/hiv/faq/en/index.html Frequently asked questions about TB and HIV.] Retrieved 6 October 2006.</ref> | Hopes that the disease could be completely eliminated have been dashed since the rise of [[Antibiotic resistant|drug-resistant]] strains in the 1980s. For example, [[tuberculosis]] cases in Britain, numbering around 117,000 in 1913, had fallen to around 5,000 in 1987, but cases rose again, reaching 6,300 in 2000 and 7,600 cases in 2005.<ref>{{cite web | url =http://www.hpa.org.uk/infections/topics_AZ/tb/epidemiology/table1.htm | title = Tuberculosis – Respiratory and Non-respiratory Notifications, England and Wales, 1913-2005 | publisher = Health Protection Agency Centre for Infections | date = 21 March 2007 | accessdate = 2007-08-01}}</ref> Due to the elimination of [[public health]] facilities in New York and the emergence of [[HIV]], there was a resurgence in the late 1980s.<ref name="Paolo_2004">{{cite journal |author=Paolo W, Nosanchuk J |title=Tuberculosis in New York city: recent lessons and a look ahead |journal=Lancet Infect Dis |volume=4 |issue=5 |pages=287-93 |year=2004 | pmid = 15120345}}</ref> The number of those failing to complete their course of drugs is high. NY had to cope with more than 20,000 unnecessary [[TB]]-patients with [[Multidrug resistance|multidrug-resistant]] strains (resistant to, at least, both [[Rifampin]] and [[Isoniazid]] . The resurgence of [[tuberculosis]] resulted in the declaration of a global health emergency by the [[World Health Organization]] in 1993.<ref>[[World Health Organization]] (WHO). [http://www.who.int/tb/hiv/faq/en/index.html Frequently asked questions about TB and HIV.] Retrieved 6 October 2006.</ref> | ||
<br clear="left"/> | <br clear="left" /> | ||
==References== | ==References== | ||
Revision as of 03:52, 25 January 2021
|
Tuberculosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tuberculosis historical perspective On the Web |
|
American Roentgen Ray Society Images of Tuberculosis historical perspective |
|
Risk calculators and risk factors for Tuberculosis historical perspective |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mashal Awais, M.D.[2]; João André Alves Silva, M.D. [3]
Overview
Tuberculosis has been present in humans since ancient times. The earliest unambiguous detection of Mycobacterium tuberculosis was in the remains of bison, dated 18,000 BC.[1] However, whether tuberculosis originated in cattle and then transferred to humans, or diverged from a common ancestor, is unclear.[2] Through history tuberculosis has had many names including phthisis and Wasting disease, which were mostly derived from its symptoms. The Mycobacterium tuberculosis was only identified in 1882 by Robert Koch. In the 19th and early 20th centuries, tuberculosis caused the most widespread public concern, which is considered an endemic disease of the urban poor. It was only in 1946, with the development of the antibiotic streptomycin, that effective treatment and cure became possible. Since the rise of drug-resistant strains in the 1980s, hopes that the disease could be completely eliminated have been dashed.
Historical Perspective
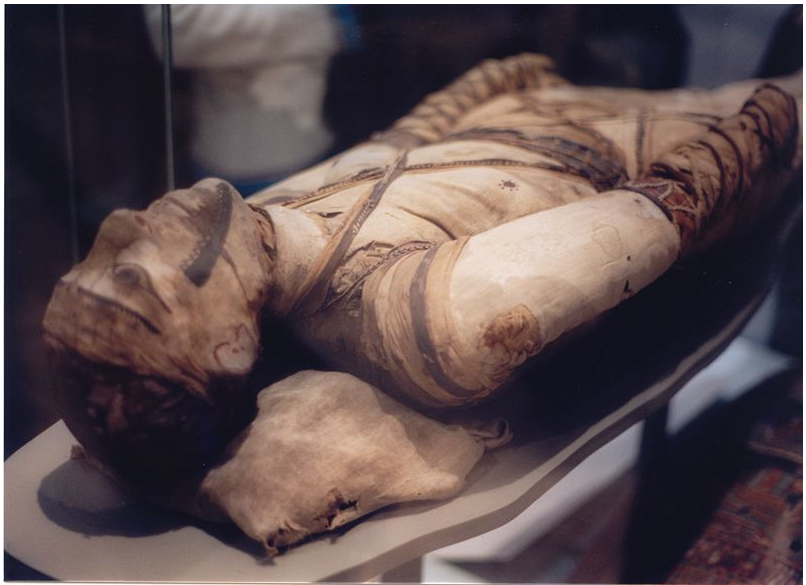
Prehistoric humans –evidenced by skeletal remains- (4000 BC) were infected with TB, in addition to the spines of mummies showing tubercular decay from 3000-2400 BC.[4] Phthisis is a Greek term for tuberculosis; around 460 BC. In terms of Hippocrates point of view, phthisis was the most widespread disease of the time involving fever and coughing up blood, which was almost always fatal.[5] TB was present in South America for about 2,000 years evidenced by some genetic studies.[6] In South America, the earliest evidence of tuberculosis was linked to the Paracas-Caverna culture (circa 750 BC to circa 100 AD).[7]
Previously, tuberculosis was named consumption, because it was like consumption of the affected people from within, with fever, bloody cough, pallor, and severe wasting. Other names are:[8][9][8][10]
- Phthisis (Greek for consumption)
- Phthisis pulmonalis
- Scrofula (in adults) - affecting the lymphatic system, resulting in swollen cervical lymph nodes
- Tabes mesenterica - TB of the abdomen
- Lupus vulgaris - TB of the skin
- Wasting disease
- White plague - because sufferers appeared markedly pale
- King's evil - as people had a false belief that that scrofula would heal by the king’s touch
- Pott's disease - TB of the spine
- Miliary tuberculosis – now commonly known as disseminated TB, occurs when the infection invades the blood stream, resulting in lesions with the appearance of millet seeds on x-ray.
Folklore
Before the industrial revolution, tuberculosis may sometimes have been regarded as vampirism. When one member of a family died from it, the other members that were infected would lose their health slowly. People believed that this was caused by the original victim draining the life from the other family members. Furthermore, people who had TB exhibited symptoms similar to what people considered to be vampire traits. People with TB often have symptoms such as red, swollen eyes (which also creates a sensitivity to bright light), pale skin and coughing blood. This suggested the idea that the only way for the afflicted to replenish this loss of blood was by sucking blood.[11] Another folk belief attributed it to being forced, nightly, to attend fairy revels, so that the victim wasted away owing to lack of rest; this belief was most common when a strong connection was seen between the fairies and the dead.[12] Similarly, but less commonly, it was attributed to the victims being 'hagridden' - being transformed into horses by witches (hags) to travel to their nightly meetings, again resulting in a lack of rest.[12]
TB was romanticized in the nineteenth century. Many at the time believed TB produced feelings of euphoria referred to as 'Spes phthisica' or 'hope of the consumptive'. It was believed that TB sufferers who were artists had bursts of creativity as the disease progressed. It was also believed that TB sufferers acquired a final burst of energy just before they died which made women more beautiful and men more creative.[13]
Study and Treatment
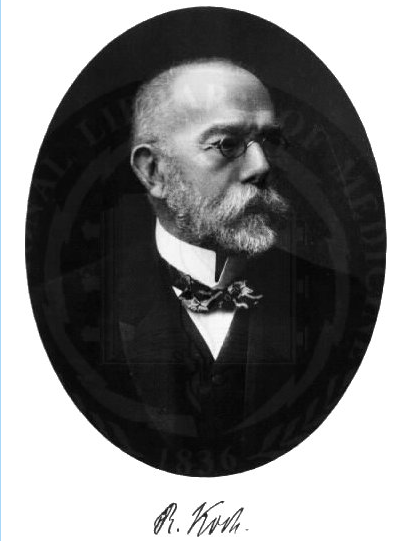
The study of tuberculosis dates back to The Canon of Medicine written by Ibn Sina (Avicenna) in the 1020s. He was the first physician to identify pulmonary tuberculosis as a contagious disease and suggest that it could spread through contact with soil and water.[14][15] He developed the method of quarantine in order to limit the spread of tuberculosis.[16]
Although it was established that the pulmonary form was associated with 'tubercles' by Dr Richard Morton in 1689,[17][18] due to the variety of its symptoms, TB was not identified as a single disease until the 1820s and was not named 'tuberculosis' until 1839 by J. L. Schönlein.[19] During the years 1838-1845, Dr. John Croghan, the owner of Mammoth Cave, brought a number of tuberculosis sufferers into the cave in the hope of curing the disease with the constant temperature and purity of the cave air: they died within a year.[20] The first TB sanatorium opened in 1859 in Görbersdorf, Germany (today Sokołowsko, Poland) by Hermann Brehmer.[21]
In regard to this claim, The Times for January 15, 1859, page 5, column 5, carries an advertisement seeking funds for the Bournemouth Sanatorium for Consumption, referring to the balance sheet for the past year, and offering an annual report to prospective donors, implying that this sanatorium was in existence at least in 1858. The bacillus causing tuberculosis, Mycobacterium tuberculosis, was identified and described on March 24, 1882 by Robert Koch. He received the Nobel Prize in physiology or medicine in 1905 for this discovery.[22] Koch did not believe that bovine (cattle) and human tuberculosis were similar, which delayed the recognition of infected milk as a source of infection. Later, this source was eliminated by the pasteurization process. Koch announced a glycerine extract of the tubercle bacilli as a remedy for tuberculosis in 1890, calling it 'tuberculin'. It was not effective, but was later adapted as a test for pre-symptomatic tuberculosis.[23]
The first genuine success in immunizing against tuberculosis was developed from attenuated bovine-strain tuberculosis by Albert Calmette and Camille Guerin in 1906. It was called 'BCG' (Bacillus of Calmette and Guerin). The BCG vaccine was first used on humans in 1921 in France, but it wasn't until after World War II that BCG received widespread acceptance in the USA, Great Britain, and Germany.
Tuberculosis, or 'consumption' as it was commonly known, caused the most widespread public concern in the 19th and early 20th centuries as an endemic disease of the urban poor. In 1815, one in four deaths in England was of consumption; by 1918 one in six deaths in France were still caused by TB. In the 20th century, tuberculosis killed an estimated 100 million people.[24] After the establishment in the 1880s that the disease was contagious, TB was made a notifiable disease in Britain; there were campaigns to stop spitting in public places, and the infected poor were encouraged to enter sanatoria that resembled prisons; the sanatoria for the middle and upper classes offered excellent care and constant medical attention.[21] Whatever the purported benefits of the fresh air and labor in the sanatoria, even under the best conditions, 50% of those who entered were dead within five years (1916).[21]
The promotion of Christmas Seals began in Denmark during 1904, as a way to raise money for tuberculosis programs. It expanded to the United States and Canada in 1907–08 to help the National Tuberculosis Association (later called the American Lung Association).
In the United States, concern about the spread of tuberculosis played a role in the movement to prohibit public spitting except into spittoons.
In Europe, deaths from TB fell from 500 out of 100,000 in 1850 to 50 out of 100,000 by 1950. Improvements in public health were reducing tuberculosis even before the arrival of antibiotics, although the disease remained a significant threat to public health. When the Medical Research Council was formed in Britain in 1913 its initial focus was tuberculosis research.[25]
It was not until 1946 with the development of the antibiotic streptomycin that effective treatment and cure became possible. Prior to the introduction of this drug, the only treatment besides sanatoria were surgical interventions, including the pneumothorax technique - collapsing an infected lung to rest it and allow lesions to heal - a technique that was of little benefit and was largely discontinued by the 1950s.[26] The emergence of multidrug-resistant TB has again introduced surgery as part of the treatment for these infections. Here, surgical removal of lung cavities will reduce the number of bacteria in the lungs, as well as increase the exposure of the remaining bacteria to drugs in the bloodstream, which is thought to increase the effectiveness of the chemotherapy.[27]
Hopes that the disease could be completely eliminated have been dashed since the rise of drug-resistant strains in the 1980s. For example, tuberculosis cases in Britain, numbering around 117,000 in 1913, had fallen to around 5,000 in 1987, but cases rose again, reaching 6,300 in 2000 and 7,600 cases in 2005.[28] Due to the elimination of public health facilities in New York and the emergence of HIV, there was a resurgence in the late 1980s.[29] The number of those failing to complete their course of drugs is high. NY had to cope with more than 20,000 unnecessary TB-patients with multidrug-resistant strains (resistant to, at least, both Rifampin and Isoniazid . The resurgence of tuberculosis resulted in the declaration of a global health emergency by the World Health Organization in 1993.[30]
References
- ↑ Rothschild B, Martin L, Lev G, Bercovier H, Bar-Gal G, Greenblatt C, Donoghue H, Spigelman M, Brittain D (2001). "Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present". Clin Infect Dis. 33 (3): 305–11. PMID 11438894.
- ↑ Pearce-Duvet J (2006). "The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease". Biol Rev Camb Philos Soc. 81 (3): 369–82. PMID 16672105.
- ↑ 3.0 3.1 3.2 "Wikimedia Commons".
- ↑ Zink A, Sola C, Reischl U, Grabner W, Rastogi N, Wolf H, Nerlich A (2003). "Characterization of Mycobacterium tuberculosis complex DNAs from Egyptian mummies by spoligotyping". J Clin Microbiol. 41 (1): 359–67. PMID 12517873.
- ↑ Hippocrates. Aphorisms. Accessed 07 October 2006.
- ↑ Konomi N, Lebwohl E, Mowbray K, Tattersall I, Zhang D (2002). "Detection of mycobacterial DNA in Andean mummies". J Clin Microbiol. 40 (12): 4738–40. PMID 12454182.
- ↑ "South America: Prehistoric Findings". Memorias do Instituto Oswaldo Cruz, Vol. 98 (Suppl.I) January 2003. Retrieved on 2007-02-08.
- ↑ 8.0 8.1 Tuberculosis Encyclopedia Britannica, 11th ed.
- ↑ Rudy's List of Archaic Medical Terms English Glossary of Archaic Medical Terms, Diseases and Causes of Death. Accessed 09 Oct 06
- ↑ Disseminated tuberculosis NIH Medical Encyclopedia. Accessed 09 Oct 06
- ↑ Sledzik P, Bellantoni N (1994). "Brief communication: bioarcheological and biocultural evidence for the New England vampire folk belief". Am J Phys Anthropol. 94 (2): 269–74. PMID 8085617.
- ↑ 12.0 12.1 Katharine Briggs, An Encyclopedia of Fairies "Consumption" (Pantheon Books, 1976) p. 80. ISBN 0-394-73467-X
- ↑ Lawlor, Clark. "Transatlantic Consumptions: Disease, Fame and Literary Nationalism in the Davidson Sisters, Southey, and Poe". Studies in the Literary Imagination, Fall 2003. Available at findarticles.com. Retrieved on 2007-06-08.
- ↑ Y. A. Al-Sharrah (2003), "The Arab Tradition of Medical Education and its Relationship with the European Tradition", Prospects 33 (4), Springer.
- ↑ George Sarton, Introduction to the History of Science.
(cf. Dr. A. Zahoor and Dr. Z. Haq (1997). Quotations From Famous Historians of Science, Cyberistan.) - ↑ David W. Tschanz, MSPH, PhD (August 2003). "Arab Roots of European Medicine", Heart Views 4 (2).
- ↑ Who Named It? Léon Charles Albert Calmette. Retrieved on 6 October 2006.
- ↑ Trail R (1970). "Richard Morton (1637–1698)". Med Hist. 14 (2): 166–74. PMID 4914685.
- ↑ Zur Pathogenie der Impetigines. Auszug aus einer brieflichen Mitteilung an den Herausgeber. [Müller’s] Archiv für Anatomie, Physiologie und wissenschaftliche Medicin. 1839, page 82.
- ↑ Kentucky: Mammoth Cave long on history. CNN. 27 February 2004. Accessed 08 October 2006.
- ↑ 21.0 21.1 21.2 McCarthy OR (2001). "The key to the sanatoria". J R Soc Med. 94 (8): 413–7. PMID 11461990.
- ↑ Nobel Foundation. The Nobel Prize in Physiology or Medicine 1905. Accessed 07 October 2006.
- ↑ Waddington K (2004). "To stamp out "so terrible a malady": bovine tuberculosis and tuberculin testing in Britain, 1890–1939". Med Hist. 48 (1): 29–48. PMID 14968644.
- ↑ Torrey EF and Yolken RH. 2005. Their bugs are worse than their bite. Washington Post, April 3, p. B01.
- ↑ [[Medical Research Council (UK)|]]. MRC's contribution to Tuberculosis research. Accessed 02 July 2007.
- ↑ Wolfart W (1990). "[Surgical treatment of tuberculosis and its modifications—collapse therapy and resection treatment and their present-day sequelae]". Offentl Gesundheitswes. 52 (8–9): 506–11. PMID 2146567.
- ↑ Lalloo U, Naidoo R, Ambaram A (2006). "Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis". Curr Opin Pulm Med. 12 (3): 179–85. PMID 16582672.
- ↑ "Tuberculosis – Respiratory and Non-respiratory Notifications, England and Wales, 1913-2005". Health Protection Agency Centre for Infections. 21 March 2007. Retrieved 2007-08-01.
- ↑ Paolo W, Nosanchuk J (2004). "Tuberculosis in New York city: recent lessons and a look ahead". Lancet Infect Dis. 4 (5): 287–93. PMID 15120345.
- ↑ World Health Organization (WHO). Frequently asked questions about TB and HIV. Retrieved 6 October 2006.