Nephrologic Disorders and COVID-19: Difference between revisions
Jump to navigation
Jump to search
| Line 23: | Line 23: | ||
====Clinical Features of AKI by SARS-CoV-2==== | ====Clinical Features of AKI by SARS-CoV-2==== | ||
*Patients in the early stages of kidney failure may be asymptomatic. If left untreated, patients may progress to develop [[Azotemia]] and [[Uremia]], which occur due to the buildup of waste materials in the blood. | |||
*Symptoms of kidney injury include<ref name=Skorecki>{{cite book |vauthors=Skorecki K, Green J, Brenner BM |veditors=Kasper DL, Braunwald E, Fauci AS |title=Harrison's Principles of Internal Medicine|url=https://archive.org/details/harrisonsprincip00kasp |url-access=limited |edition=16th |year=2005 |publisher=McGraw-Hill |location=New York, NY |isbn=978-0-07-139140-5 |pages=[https://archive.org/details/harrisonsprincip00kasp/page/n1681 1653]–63 |chapter=Chronic renal failure|display-editors=etal}}</ref>: | |||
**Nausea and Vomiting | |||
**Weakness | |||
**Fatigue | |||
**Confusion | |||
**Weight loss | |||
**Loss of appetite | |||
**[[Oliguria]] or [[Anuria]] | |||
**Fluid retention, leading [[edema]] and swelling of face, extremities | |||
**Electrolyte imbalance; High level of [[Potassium]] which leads to [[cardiac arrhythmia]] | |||
====Treatment==== | ====Treatment==== | ||
*Management of [[AKI]] following [[COVID-19]] includes treatment of infection, identifying electrolyte disorders, and [[intravenous fluid]] administration. | *Management of [[AKI]] following [[COVID-19]] includes treatment of infection, identifying electrolyte disorders, and [[intravenous fluid]] administration. | ||
Revision as of 02:57, 22 June 2020
To go to the COVID-19 project topics list, click here.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sogand Goudarzi, MD [2] Nasrin Nikravangolsefid, MD-MPH [3]
Overview
Nephrologic_Disorders of COVID-19
Nephrologic_Disorders risk factors of COVID-19
Complications
AKI
Pathophysiology
- Angiotensin-converting enzyme 2 (ACE2), which is a primary receptor for SARS-CoV-2 entry into cells, mostly presents in renal tubular epithelial cells as well as lungs and heart.[1]
- Despite kidney injury following COVID-19 infection is less frequent than severe lung injury, ACE2: ACE ratio is higher in the kidneys compared to the respiratory system. (1:1 in the kidneys VS 1:20 in the respiratory system)[1]
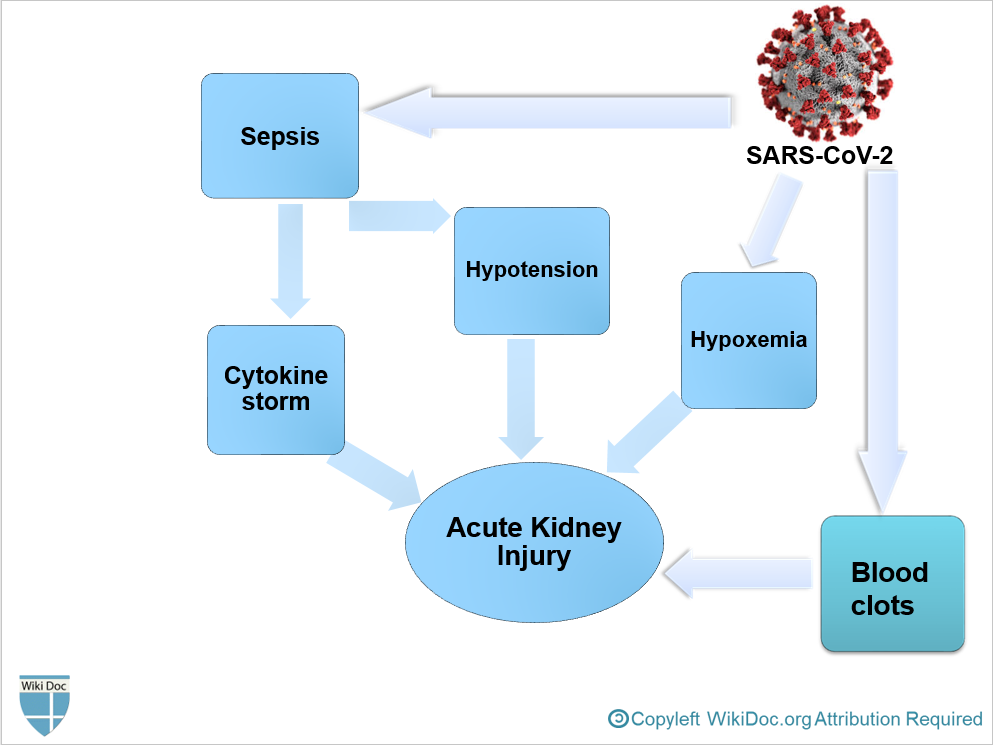
- After SARS-CoV-2 enters through the nasal cavity, it may travel to the kidneys and enters the bloodstream leading to severe inflammatory response activation and cytokine storm.
- It is thought that AKI following COVID-19 is the result of[1]
- Sepsis
- Hypovolemia and Hypotension
- Hypoxemia
- Blood clots formation, leading to impaired blood flow in the renal arterioles.
- AKI often occurs at later stages in critically ill patients with COVID-19 following multiple organ failure.
Clinical Features of AKI by SARS-CoV-2
- Patients in the early stages of kidney failure may be asymptomatic. If left untreated, patients may progress to develop Azotemia and Uremia, which occur due to the buildup of waste materials in the blood.
- Symptoms of kidney injury include[2]:
- Nausea and Vomiting
- Weakness
- Fatigue
- Confusion
- Weight loss
- Loss of appetite
- Oliguria or Anuria
- Fluid retention, leading edema and swelling of face, extremities
- Electrolyte imbalance; High level of Potassium which leads to cardiac arrhythmia
Treatment
- Management of AKI following COVID-19 includes treatment of infection, identifying electrolyte disorders, and intravenous fluid administration.
- Treatment of AKI following COVID-19 includes[3]:
- Correction of hypovolemia and hypotension by the administration of adequate intravenous fluid
- Correction of electrolyte disturbances
- Renal Replacement Therapy
- If AKI is unresponsive to conservative therapy
- In volume overload conditions
- Modality of choice in unstable hemodynamic status
- Anticoagulants in hypercoagulable conditions
- Sequential extracorporeal therapy
- ↑ 1.0 1.1 1.2 Malha, Line; Mueller, Franco B.; Pecker, Mark S.; Mann, Samuel J.; August, Phyllis; Feig, Peter U. (2020). "COVID-19 and the Renin-Angiotensin System". Kidney International Reports. 5 (5): 563–565. doi:10.1016/j.ekir.2020.03.024. ISSN 2468-0249.
- ↑ Skorecki K, Green J, Brenner BM (2005). "Chronic renal failure". In Kasper DL, Braunwald E, Fauci AS, et al. Harrison's Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 1653–63. ISBN 978-0-07-139140-5.
- ↑ Ronco C, Reis T, Husain-Syed F (2020). "Management of acute kidney injury in patients with COVID-19". Lancet Respir Med. doi:10.1016/S2213-2600(20)30229-0. PMC 7255232 Check
|pmc=value (help). PMID 32416769 Check|pmid=value (help).