Multiple endocrine neoplasia type 2 surgery: Difference between revisions
Irfan Dotani (talk | contribs) No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Surgery is the mainstay of treatment for multiple endocrine neoplasia type 2. | Surgery is the mainstay of treatment for multiple endocrine neoplasia type 2. Management of multiple endocrine neoplasia type 2 patients includes [[thyroidectomy]] including cervical, central, and bilateral [[lymph node]]s dissection for [[medullary thyroid carcinoma]], unilateral [[adrenalectomy]] for unilateral [[pheochromocytoma]] or bilateral [[adrenalectomy]] when both [[gland]]s are involved, and selective resection of pathologic [[parathyroid gland]]s for [[primary hyperparathyroidism]]. | ||
==Surgery== | ==Surgery== | ||
Management of multiple endocrine neoplasia type 2 patients includes [[thyroidectomy]] including cervical central and bilateral [[lymph node]]s dissection for [[medullary thyroid carcinoma]], unilateral [[adrenalectomy]] for unilateral [[pheochromocytoma]] or bilateral [[adrenalectomy]] when both [[gland]]s are involved, and selective resection of pathologic [[parathyroid gland]]s for [[primary hyperparathyroidism]]. | Management of multiple endocrine neoplasia type 2 patients includes [[thyroidectomy]] including cervical, central, and bilateral [[lymph node]]s dissection for [[medullary thyroid carcinoma]], unilateral [[adrenalectomy]] for unilateral [[pheochromocytoma]] or bilateral [[adrenalectomy]] when both [[gland]]s are involved, and selective resection of pathologic [[parathyroid gland]]s for [[primary hyperparathyroidism]]. | ||
===Medullary Thyroid Cancer=== | ===Medullary Thyroid Cancer=== | ||
====Conventional Therapy==== | ====Conventional Therapy==== | ||
* The treatment of choice for primary [[medullary thyroid carcinoma]], both sporadic or hereditary, is total [[thyroidectomy]] with systematic dissection of all [[lymph node]]s of the central compartment. Total [[thyroidectomy]] is necessary as [[medullary thyroid carcinoma]] is multicentric in 65–90% of patients in multiple endocrine neoplasia type 2 and extensive central [[lymph node]] dissection has been reported to improve survival and recurrence rates compared to less aggressive procedures.<ref name="pmid17665245">{{cite journal| author=Machens A, Hauptmann S, Dralle H| title=Increased risk of lymph node metastasis in multifocal hereditary and sporadic medullary thyroid cancer. | journal=World J Surg | year= 2007 | volume= 31 | issue= 10 | pages= 1960-5 | pmid=17665245 | doi=10.1007/s00268-007-9185-1 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17665245 }}</ref><ref name="pmid6128962">{{cite journal| author=Russell CF, Van Heerden JA, Sizemore GW, Edis AJ, Taylor WF, ReMine WH et al.| title=The surgical management of medullary thyroid carcinoma. | journal=Ann Surg | year= 1983 | volume= 197 | issue= 1 | pages= 42-8 | pmid=6128962 | doi= | pmc=PMC1352852 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6128962 }} </ref> [[Lymph node]] dissection of laterocervical compartments is not performed on principle but only when the neck [[ultrasound]] suggests the presence of metastatic nodes. | * The treatment of choice for primary [[medullary thyroid carcinoma]], both sporadic or hereditary, is total [[thyroidectomy]] with systematic dissection of all [[lymph node]]s of the central compartment. Total [[thyroidectomy]] is necessary as [[medullary thyroid carcinoma]] is multicentric in 65–90% of patients in multiple endocrine neoplasia type 2 and extensive central [[lymph node]] dissection has been reported to improve survival and recurrence rates compared to less aggressive procedures.<ref name="pmid17665245">{{cite journal| author=Machens A, Hauptmann S, Dralle H| title=Increased risk of lymph node metastasis in multifocal hereditary and sporadic medullary thyroid cancer. | journal=World J Surg | year= 2007 | volume= 31 | issue= 10 | pages= 1960-5 | pmid=17665245 | doi=10.1007/s00268-007-9185-1 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17665245 }}</ref><ref name="pmid6128962">{{cite journal| author=Russell CF, Van Heerden JA, Sizemore GW, Edis AJ, Taylor WF, ReMine WH et al.| title=The surgical management of medullary thyroid carcinoma. | journal=Ann Surg | year= 1983 | volume= 197 | issue= 1 | pages= 42-8 | pmid=6128962 | doi= | pmc=PMC1352852 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6128962 }} </ref> [[Lymph node]] dissection of laterocervical compartments is not performed on principle but only when the neck [[ultrasound]] suggests the presence of [[Metastatic Cancer of Unknown Primary Site|metastatic]] nodes. | ||
* Endoscopic adrenal-sparing [[surgery]] has become the method of choice for the surgical therapy of [[pheochromocytoma]].<ref name="pmid18784938">{{cite journal| author=Walz MK, Alesina PF| title=Single access retroperitoneoscopic adrenalectomy (SARA)--one step beyond in endocrine surgery. | journal=Langenbecks Arch Surg | year= 2009 | volume= 394 | issue= 3 | pages= 447-50 | pmid=18784938 | doi=10.1007/s00423-008-0418-z | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18784938 }} </ref> In cases with an asynchronous development of [[pheochromocytoma]], the adrenal gland without [[pheochromocytoma]] can be preserved, but the patient must be aware that the probability to repeat the surgical treatment in the near future is very high. The advantage of a | * [[Endoscopic]] adrenal-sparing [[surgery]] has become the method of choice for the surgical therapy of [[pheochromocytoma]].<ref name="pmid18784938">{{cite journal| author=Walz MK, Alesina PF| title=Single access retroperitoneoscopic adrenalectomy (SARA)--one step beyond in endocrine surgery. | journal=Langenbecks Arch Surg | year= 2009 | volume= 394 | issue= 3 | pages= 447-50 | pmid=18784938 | doi=10.1007/s00423-008-0418-z | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18784938 }} </ref> In cases with an asynchronous development of [[pheochromocytoma]], the [[adrenal gland]] without [[pheochromocytoma]] can be preserved, but the patient must be aware that the probability to repeat the surgical treatment in the near future is very high. The advantage of a unilateral [[adrenal]] [[surgery]] is the possibility to avoid substitute therapy until the second [[surgery]] is performed. | ||
* The [[parathyroid gland]]s are frequently found to be enlarged at the time of the [[thyroidectomy]] for [[medullary thyroid carcinoma]] and should, therefore, be carefully evaluated. The goal in multiple endocrine neoplasia type 2 patients with | * The [[parathyroid gland]]s are frequently found to be enlarged at the time of the [[thyroidectomy]] for [[medullary thyroid carcinoma]] and should, therefore, be carefully evaluated. The goal in multiple endocrine neoplasia type 2 patients with [[primary hyperparathyroidism]] (PHPT) is to excise the enlarged [[gland]]s and to leave at least one apparently normal [[parathyroid]] [[gland]] intact. If all [[gland]]s are enlarged, a subtotal [[parathyroidectomy]] or total [[parathyroidectomy]] with [[autotransplantation]] should be performed. | ||
====Prophylactic or Precocious Thyroidectomy in RET Gene Carrier==== | ====Prophylactic or Precocious Thyroidectomy in RET Gene Carrier==== | ||
* Prophylactic [[thyroidectomy]] is advised in [[gene]] carriers to guarantee a definitive cure in these subjects. | * Prophylactic [[thyroidectomy]] is advised in [[gene]] carriers to guarantee a definitive cure in these subjects. | ||
* | * In 1999, during the Seventh International Multiple Endocrine Neoplasia Meeting in Gubbio, the risk of [[MTC]] has been stratified in three categories according to the mutations of c-''[[RET gene|RET]]'' as following: | ||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | ||
|+'''''Prophylactic Thyroidectomy''''' | |+'''''Prophylactic Thyroidectomy''''' | ||
! style="background: #4479BA; width: 120px;" | {{fontcolor|#FFF|Gene}} | ! style="background: #4479BA; width: 120px;" | {{fontcolor|#FFF|Gene}} | ||
| Line 40: | Line 40: | ||
! style="background: #F5F5F5;" | Operated at a later stage | ! style="background: #F5F5F5;" | Operated at a later stage | ||
|} | |} | ||
* Recently, some evidences in big series of ''RET'' gene carriers demonstrated that [[gene]] carriers with undetectable levels of basal [[calcitonin]] have an almost null risk to have already developed the [[medullary thyroid carcinoma]].<ref name="pmid19801688">{{cite journal| author=Lau GS, Lang BH, Lo CY, Tso A, Garcia-Barcelo MM, Tam PK et al.| title=Prophylactic thyroidectomy in ethnic Chinese patients with multiple endocrine neoplasia type 2A syndrome after the introduction of genetic testing. | journal=Hong Kong Med J | year= 2009 | volume= 15 | issue= 5 | pages= 326-31 | pmid=19801688 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19801688 }} </ref><ref> Prognostic Factors of Disease-Free Survival after Thyroidectomy in 170 Young Patients with a RET Germline Mutation: A Multicenter Study of the Groupe Français d'Etude des Tumeurs Endocrines. Endocrine Society (30.09,2015)http://press.endocrine.org/doi/abs/10.1210/jc.2010-1234 accessed on October, 2015</ref> Moreover, a serum Ct <30–40 pg/mL is always associated to an intrathyroidal micro-medullary thyroid carcinoma without any evidence of [[lymph node]] [[metastases]]. Moreover, a serum Ct <30–40 pg/mL is always associated to an intrathyroidal micro-medullary thyroid carcinoma without any evidence of [[lymph node]] [[metastases]] | * Recently, some evidences in big series of [[RET gene|''RET'' gene]] carriers demonstrated that [[gene]] carriers with undetectable levels of basal [[calcitonin]] (Ct) have an almost null risk to have already developed the [[medullary thyroid carcinoma]].<ref name="pmid19801688">{{cite journal| author=Lau GS, Lang BH, Lo CY, Tso A, Garcia-Barcelo MM, Tam PK et al.| title=Prophylactic thyroidectomy in ethnic Chinese patients with multiple endocrine neoplasia type 2A syndrome after the introduction of genetic testing. | journal=Hong Kong Med J | year= 2009 | volume= 15 | issue= 5 | pages= 326-31 | pmid=19801688 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19801688 }} </ref><ref>Prognostic Factors of Disease-Free Survival after Thyroidectomy in 170 Young Patients with a RET Germline Mutation: A Multicenter Study of the Groupe Français d'Etude des Tumeurs Endocrines. Endocrine Society (30.09,2015)http://press.endocrine.org/doi/abs/10.1210/jc.2010-1234 accessed on October, 2015</ref> Moreover, a serum Ct <30–40 pg/mL is always associated to an intrathyroidal micro-[[medullary thyroid carcinoma]] without any evidence of [[lymph node]] [[metastases]]. Moreover, a serum Ct <30–40 pg/mL is always associated to an intrathyroidal micro-medullary thyroid carcinoma without any evidence of [[lymph node]] [[metastases]]. | ||
* The following flowchart depicts the surgical management of medullary thyroid cancer | * The following flowchart depicts the surgical management of medullary thyroid cancer: | ||
[[File:Medullary thyroid cancer.png|thumb|center|500px|ESMO clinical practice guidelines for treatment of medullary cell carcinoma]] | [[File:Medullary thyroid cancer.png|thumb|center|500px|ESMO clinical practice guidelines for treatment of medullary cell carcinoma]] | ||
=====Post Surgery===== | =====Post Surgery===== | ||
* [[Thyroxine]] should be supplemented for patients undergoing total [[thyroidectomy]].<ref name="pmid22997443">{{cite journal| author=Pacini F, Castagna MG, Brilli L, Pentheroudakis G, ESMO Guidelines Working Group| title=Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. | journal=Ann Oncol | year= 2012 | volume= 23 Suppl 7 | issue= | pages= vii110-9 | pmid=22997443 | doi=10.1093/annonc/mds230 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22997443 }} </ref> | * [[Thyroxine]] should be supplemented for patients undergoing total [[thyroidectomy]].<ref name="pmid22997443">{{cite journal| author=Pacini F, Castagna MG, Brilli L, Pentheroudakis G, ESMO Guidelines Working Group| title=Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. | journal=Ann Oncol | year= 2012 | volume= 23 Suppl 7 | issue= | pages= vii110-9 | pmid=22997443 | doi=10.1093/annonc/mds230 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22997443 }} </ref> | ||
* Serum [[calcitonin]] and carcinoembryonic antigen doubling time (CEA DT) are measured during post surgical follow-up. | * Serum [[calcitonin]] and [[carcinoembryonic antigen]] doubling time (CEA DT) are measured during post surgical follow-up. | ||
* Provacative [[pentagastrin]] or [[calcium]] test is administered and serum [[calcitonin]] level is measured. | * Provacative [[pentagastrin]] or [[calcium]] test is administered and serum [[calcitonin]] level is measured. | ||
* If there is no significant elevation in serum [[calcitonin]] level, serum [[calcitonin]] is measured every 6 months for 2-3 years and then yearly. | * If there is no significant elevation in serum [[calcitonin]] level, serum [[calcitonin]] is measured every 6 months for 2-3 years and then yearly. | ||
* If the [[calcitonin]] is below 150 pg/ml, ultrasound [[neck]] is recommended. | * If the [[calcitonin]] is below 150 pg/ml, [[Ultrasound-enhanced systemic thrombolysis|ultrasound]] [[neck]] is recommended. | ||
* If the basal serum [[calcitonin]] is above 150 pg/ml, screening for distant [[metastasis]] is recommended. | * If the basal serum [[calcitonin]] is above 150 pg/ml, screening for distant [[metastasis]] is recommended. | ||
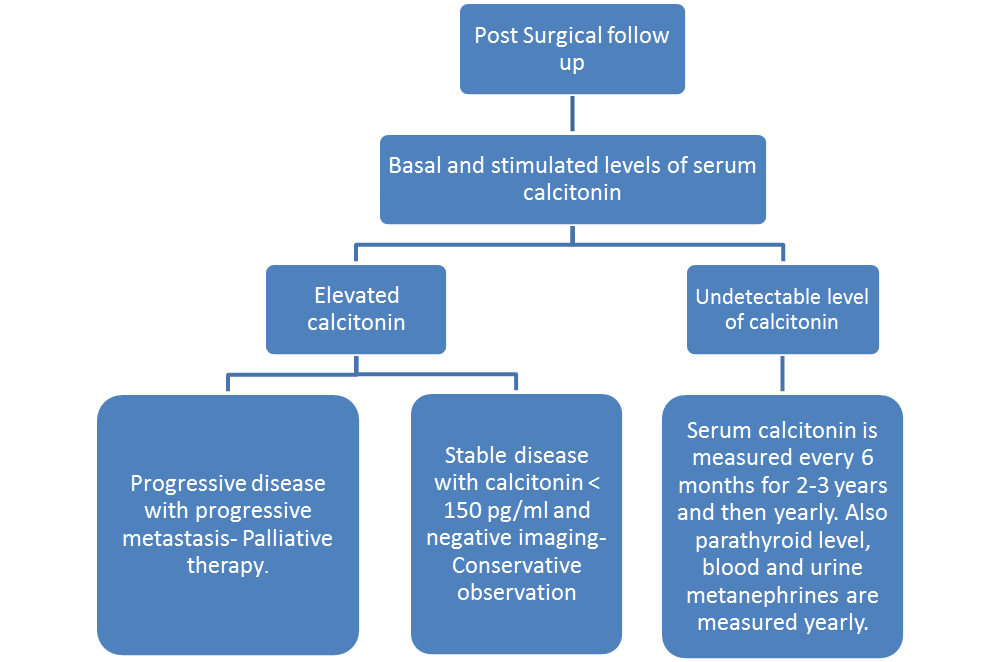
* The following flowchart depicts the post surgical management of medullary thyroid cancer | * The following flowchart depicts the post surgical management of medullary thyroid cancer: | ||
[[File:Post surgical follow up MEN 2.png|thumb|center|500px|ESMO clinical practice guidelines for treatment of medullary cell carcinoma]] | [[File:Post surgical follow up MEN 2.png|thumb|center|500px|ESMO clinical practice guidelines for treatment of medullary cell carcinoma]] | ||
Revision as of 16:31, 25 October 2017
|
Multiple endocrine neoplasia type 2 Microchapters |
|
Differentiating Multiple endocrine neoplasia type 2 from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Multiple endocrine neoplasia type 2 surgery On the Web |
|
American Roentgen Ray Society Images of Multiple endocrine neoplasia type 2 surgery |
|
Directions to Hospitals Treating Multiple endocrine neoplasia type 2 |
|
Risk calculators and risk factors for Multiple endocrine neoplasia type 2 surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Overview
Surgery is the mainstay of treatment for multiple endocrine neoplasia type 2. Management of multiple endocrine neoplasia type 2 patients includes thyroidectomy including cervical, central, and bilateral lymph nodes dissection for medullary thyroid carcinoma, unilateral adrenalectomy for unilateral pheochromocytoma or bilateral adrenalectomy when both glands are involved, and selective resection of pathologic parathyroid glands for primary hyperparathyroidism.
Surgery
Management of multiple endocrine neoplasia type 2 patients includes thyroidectomy including cervical, central, and bilateral lymph nodes dissection for medullary thyroid carcinoma, unilateral adrenalectomy for unilateral pheochromocytoma or bilateral adrenalectomy when both glands are involved, and selective resection of pathologic parathyroid glands for primary hyperparathyroidism.
Medullary Thyroid Cancer
Conventional Therapy
- The treatment of choice for primary medullary thyroid carcinoma, both sporadic or hereditary, is total thyroidectomy with systematic dissection of all lymph nodes of the central compartment. Total thyroidectomy is necessary as medullary thyroid carcinoma is multicentric in 65–90% of patients in multiple endocrine neoplasia type 2 and extensive central lymph node dissection has been reported to improve survival and recurrence rates compared to less aggressive procedures.[1][2] Lymph node dissection of laterocervical compartments is not performed on principle but only when the neck ultrasound suggests the presence of metastatic nodes.
- Endoscopic adrenal-sparing surgery has become the method of choice for the surgical therapy of pheochromocytoma.[3] In cases with an asynchronous development of pheochromocytoma, the adrenal gland without pheochromocytoma can be preserved, but the patient must be aware that the probability to repeat the surgical treatment in the near future is very high. The advantage of a unilateral adrenal surgery is the possibility to avoid substitute therapy until the second surgery is performed.
- The parathyroid glands are frequently found to be enlarged at the time of the thyroidectomy for medullary thyroid carcinoma and should, therefore, be carefully evaluated. The goal in multiple endocrine neoplasia type 2 patients with primary hyperparathyroidism (PHPT) is to excise the enlarged glands and to leave at least one apparently normal parathyroid gland intact. If all glands are enlarged, a subtotal parathyroidectomy or total parathyroidectomy with autotransplantation should be performed.
Prophylactic or Precocious Thyroidectomy in RET Gene Carrier
- Prophylactic thyroidectomy is advised in gene carriers to guarantee a definitive cure in these subjects.
- In 1999, during the Seventh International Multiple Endocrine Neoplasia Meeting in Gubbio, the risk of MTC has been stratified in three categories according to the mutations of c-RET as following:
| Gene | Risk | Treatment |
|---|---|---|
| Children with MEN2B and/or c-RET codon 883, 918,
922 |
Highest risk of aggressive medullary thyroid carcinoma | Total thyroidectomy with
central node dissection, within the first six months. |
| Children with any c-RET codon 611, 618, 620 or 634
mutations |
High risk of medullary thyroid carcinoma | Total thyroidectomy should be performed before age of
five years, with or without central node dissection. |
| Children with c-RET codon 609, 768, 790, 791, 804
and 891 mutations |
Less aggressive and slowly growing medullary thyroid carcinoma | Operated at a later stage |
- Recently, some evidences in big series of RET gene carriers demonstrated that gene carriers with undetectable levels of basal calcitonin (Ct) have an almost null risk to have already developed the medullary thyroid carcinoma.[4][5] Moreover, a serum Ct <30–40 pg/mL is always associated to an intrathyroidal micro-medullary thyroid carcinoma without any evidence of lymph node metastases. Moreover, a serum Ct <30–40 pg/mL is always associated to an intrathyroidal micro-medullary thyroid carcinoma without any evidence of lymph node metastases.
- The following flowchart depicts the surgical management of medullary thyroid cancer:

Post Surgery
- Thyroxine should be supplemented for patients undergoing total thyroidectomy.[6]
- Serum calcitonin and carcinoembryonic antigen doubling time (CEA DT) are measured during post surgical follow-up.
- Provacative pentagastrin or calcium test is administered and serum calcitonin level is measured.
- If there is no significant elevation in serum calcitonin level, serum calcitonin is measured every 6 months for 2-3 years and then yearly.
- If the calcitonin is below 150 pg/ml, ultrasound neck is recommended.
- If the basal serum calcitonin is above 150 pg/ml, screening for distant metastasis is recommended.
- The following flowchart depicts the post surgical management of medullary thyroid cancer:
References
- ↑ Machens A, Hauptmann S, Dralle H (2007). "Increased risk of lymph node metastasis in multifocal hereditary and sporadic medullary thyroid cancer". World J Surg. 31 (10): 1960–5. doi:10.1007/s00268-007-9185-1. PMID 17665245.
- ↑ Russell CF, Van Heerden JA, Sizemore GW, Edis AJ, Taylor WF, ReMine WH; et al. (1983). "The surgical management of medullary thyroid carcinoma". Ann Surg. 197 (1): 42–8. PMC 1352852. PMID 6128962.
- ↑ Walz MK, Alesina PF (2009). "Single access retroperitoneoscopic adrenalectomy (SARA)--one step beyond in endocrine surgery". Langenbecks Arch Surg. 394 (3): 447–50. doi:10.1007/s00423-008-0418-z. PMID 18784938.
- ↑ Lau GS, Lang BH, Lo CY, Tso A, Garcia-Barcelo MM, Tam PK; et al. (2009). "Prophylactic thyroidectomy in ethnic Chinese patients with multiple endocrine neoplasia type 2A syndrome after the introduction of genetic testing". Hong Kong Med J. 15 (5): 326–31. PMID 19801688.
- ↑ Prognostic Factors of Disease-Free Survival after Thyroidectomy in 170 Young Patients with a RET Germline Mutation: A Multicenter Study of the Groupe Français d'Etude des Tumeurs Endocrines. Endocrine Society (30.09,2015)http://press.endocrine.org/doi/abs/10.1210/jc.2010-1234 accessed on October, 2015
- ↑ Pacini F, Castagna MG, Brilli L, Pentheroudakis G, ESMO Guidelines Working Group (2012). "Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up". Ann Oncol. 23 Suppl 7: vii110–9. doi:10.1093/annonc/mds230. PMID 22997443.