Paroxysmal AV block interventions: Difference between revisions
Homa Najafi (talk | contribs) No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
{{CMG}}; {{AE}}{{Akash}} | {{CMG}}; {{AE}}{{Akash}} | ||
==Overview== | ==Overview== | ||
Several studies have demonstrated the efficacy of [[cardiac pacing]] in [[paroxysmal AV block]]. Temporary pacing should be used for the minimum duration necessary to prevent [[hemodynamic]] compromise and [[asystole]]. The presence or absence of [[Symptom|symptoms]] and the correlation of those symptoms with a [[Conduction System|conduction]] defect is an important determinant of [[cardiac pacing]]. An improvement in conduction suggests that the level of the block is at the level of the [[AV node]]. Counterpressure maneuvers may be helpful in preventing [[Vagal|vagally]] mediated [[syncope]]. | |||
==European Society of Cardiology : Indications for Cardiac Pacing== | |||
[ | [[Image: Cardiac Pacing Indications.JPG|thumb|center|500px|Indications-{{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}}]] | ||
*The major factors predicting the efficacy of pacing in preventing [[syncope]] recurrence are an '''established relationship between [[symptoms]] and [[bradycardia]] and the absence of associated [[Hypotension|hypotensive]] susceptibility '''. | |||
**When this relationship is less established, or some [[hypotensive]] mechanism is present, [[syncope]] can recur in a minority of patients. | |||
**[[Pacing]] is '''not indicated in unexplained [[syncope]] without evidence of any [[Conduction System|conduction]] disturbance'''. | |||
**'''Less than half of the patients with bifascicular [[Bundle branch block|BBB]] and [[syncope]] have a final diagnosis of [[cardiac]] [[syncope]]''', albeit the probability is different among the types of [[Bundle branch block|BBB]]. | |||
**Elderly patients with bifascicular [[BBB]] and unexplained [[syncope]] after a reasonable workup might benefit from empirical [[pacemaker]] implantation,especially if [[syncope]] is unpredictable (with no or short prodromes) or '''has occurred in the [[supine]] position or during effort'''. {{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}} | |||
*'''Milena et al''' conducted a 4 year study to study the '''efficacy of cardiac [[pacing]]''' in patients with documented [[paroxysmal AV block]]. | |||
**The endpoints of the study focused on '''[[syncope]] recurrence and time taken till first recurrence of [[presyncope]]'''. | |||
**Recurrence was only seen in patients without structural heart disease and the mechanism was related to [[hypotension]], onset of [[atrial fibrillation]] or [[reflex]] mediated. | |||
**Significantly lower recurrence rates were seen in patients with documented [[paroxysmal AV block]] and it was also concluded that '''cardiac pacing could be offered more confidently to patients with structural heart disease'''.{{cite web |url=https://www.semanticscholar.org/paper/Syncope-in-patients-paced-for-atrioventricular-Aste-Oddone/14a61cc90f61fb38600f6d625dfb14b1d878c983 |title=Syncope in patients paced for atrioventricular block. | Semantic Scholar |format= |work= |accessdate=}} | |||
*'''The Syncope Unit Project -2 (SUP-2 )''' studied carried about by '''Brignole et al''' included patients with a history of recurrent [[syncope]] and positive findings on [[carotid sinus massage]]/ [[tilt table testing]]/ [[implantable loop recorders]]. | |||
**Such patients were fitted with '''dual chamber [[Pacemakers and implantable defibrillators (patient information)|pacemakers]] and recurrence rates were followed up'''. | |||
**Using a standardized algorithm in their approach, they came to the conclusion that [[pacing]] can be can be offered to patients with positive findings on [[carotid sinus massage]]/ [[tilt table testing]]/ [[implantable loop recorders]]. | |||
**An '''efficacy of 3 years was maintained'''. | |||
**Furthermore, similar results were also found in those with '''[[intrinsic paroxysmal AV block]] patients and in [[Tilt table test|tilt table]] positive [[Asystole|asystolic]] [[reflex]] [[syncope]] patients'''.<ref name="pmid26612880">{{cite journal| author=Brignole M, Arabia F, Ammirati F, Tomaino M, Quartieri F, Rafanelli M | display-authors=etal| title=Standardized algorithm for cardiac pacing in older patients affected by severe unpredictable reflex syncope: 3-year insights from the Syncope Unit Project 2 (SUP 2) study. | journal=Europace | year= 2016 | volume= 18 | issue= 9 | pages= 1427-33 | pmid=26612880 | doi=10.1093/europace/euv343 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26612880 }} </ref> | |||
**'''The ISSUE 3 study''' also produced similar results where '''TT- negative [[Asystole|asystolic]] [[reflex]] syncope patients were concerned'''. | |||
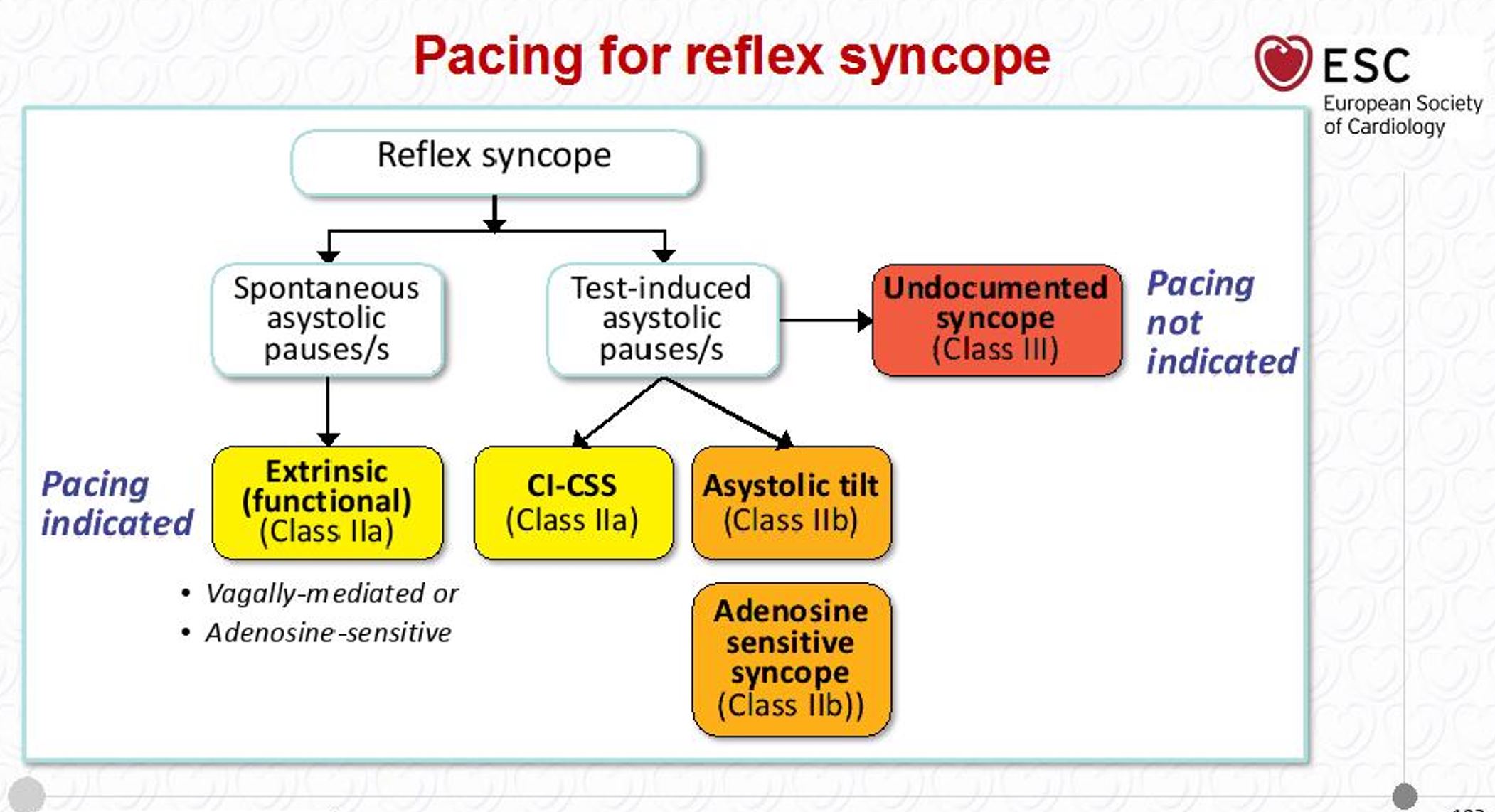
[[Image:Pacing in Reflex Syncope.JPG|thumb|center|500px|Pacing in Reflex Syncope-{{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}}]] | |||
==2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay== | |||
'''Temporary Pacing''' | |||
== | {|class="wikitable" | ||
|- | |||
| colspan="1" style="text-align:center; background: LemonChiffon"|[[2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay| Recommendations for Temporary Pacing for Bradycardia Attributable to Atrioventricular Block]] | |||
|- | |||
| bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''1.''' For patients with second-degree or third-degree atrioventricular block associated with symptoms or hemodynamic compromise that | |||
is refractory to medical therapy, temporary transvenous pacing is reasonable to increase heart rate and improve symptoms. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B-NR]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
The | '''2.'''For patients who require prolonged temporary transvenous pacing, it is reasonable to choose an externalized permanent active fixation lead over a standard passive fixation temporary pacing lead.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B-NR]])]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | ||
'''3.''' For patients with second-degree or third-degree atrioventricular block and hemodynamic compromise refractory to antibradycardic medical therapy, temporary transcutaneous | |||
pacing may be considered until a temporary transvenous or PPM is placed or the bradyarrhythmia resolves.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B-R]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' <nowiki>"</nowiki> | |||
|} | |||
*Temporary [[pacing]] is a process that requires careful consideration where timing and necessity is concerned. | |||
*It should be used for the minimum duration necessary to prevent [[hemodynamic]] compromise and [[asystole]]. | |||
*Increased safety has been noted when prolonged temporary [[pacing]] is done with an externalized active fixation [[Pacing|permanent pacing]]. <ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref> | |||
'''Chronic Therapy/Management of Bradycardia Attributable to Atrioventricular Block''' | |||
[[Image:Guidelines for Chronic Therapy.JPG|thumb|center|500px|Chronic Therapy/Management of Bradycardia Attributable to Atrioventricular Block <ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>]] | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background: LemonChiffon"|[[2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay| Recommendations for General Principles of Chronic Therapy/Management of Bradycardia Attributable to Atrioventricular Block]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' In patients with first-degree atrioventricular block or second-degree Mobitz type I (Wenckebach) or 2:1 atrioventricular block which is believed to be at the level of the atrioventricular node, with symptoms that do not temporally correspond to the atrioventricular block, permanent pacing should not be performed. ''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]]<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
'''2.'''In asymptomatic patients with first-degree atrioventricular block or second-degree Mobitz type I (Wenckebach) or 2:1 atrioventricular block which is believed to be at the level of the atrioventricular node, permanent pacing should not be performed.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
|} | |||
*The presence or absence of [[Symptom|symptoms]] is a major determinant on whether permanent pacing will be required in the setting of [[bradycardia]] associated with [[atrioventricular block]]. | |||
*Improvement in [[atrioventricular]] [[Conduction System|conduction]] suggests that the site of block is at the [[atrioventricular node]], whereas worsening atrioventricular conduction suggests infranodal block. If the symptoms do not clearly correspond to the episodes of atrioventricular block, the risks associated with the [[pacemaker]] in the absence of clear benefit make the overall risk-benefit ratio unfavorable. | |||
*If the level of the block is at the [[atrioventricular node]], then sudden progression to a higher degree of atrioventricular block is unlikely. | |||
*Given the procedural and long-term risks of PPMs, in the absence of mitigating circumstances, for patients with first-degree or second-degree Mobitz type I (Wenckebach) atrioventricular block that does not clearly correspond to [[Symptom|symptoms]], further monitoring and follow up should be implemented. | |||
'''Permanent Pacing''' | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background: Pink"|[[2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay| Recommendations for Permanent Pacing for Chronic Therapy/Management of Bradycardia Attributable to Atrioventricular Block ]] | |||
|- | |||
| bgcolor="Pink"|<nowiki>"</nowiki>' '''1.''' In patients with acquired second-degree Mobitz type II atrioventricular block, highgrade atrioventricular block, or third-degree | |||
atrioventricular block not attributable to reversible or physiologic causes, permanent pacing is recommended regardless of symptoms.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B-NR]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
'''2.''' In patients with neuromuscular diseases associated with conduction disorders, including muscular dystrophy (eg,myotonic dystrophy type 1) or Kearns-Sayre syndrome, who have evidence of seconddegree atrioventricular block, third-degree atrioventricular block, or an HV interval of 70 ms or greater, regardless of symptoms, permanent pacing, with additional defibrillator capability if needed and meaningful survival of greater than 1 year is expected, is recommended''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B-NR]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
'''3.''' In patients with permanent AF and symptomatic bradycardia, permanent pacing is recommended.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
'''4.'''In patients who develop symptomatic atrioventricular block as a consequence of guideline-directed management and therapy for which there is no alternative treatment and continued treatment is clinically necessary, permanent pacing is recommended to increase heart rate and improve symptoms''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
'''5.'''In patients with an infiltrative cardiomyopathy, such as cardiac sarcoidosis or amyloidosis, and seconddegree Mobitz type II atrioventricular block,high-grade atrioventricular block, or thirddegree atrioventricular block, permanent pacing, with additional defibrillator capability if needed and meaningful survival of greater than 1 year is expected,is reasonable''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B-NR]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
'''6.'''In patients with lamin A/C gene mutations,including limb-girdle and Emery-Dreifuss muscular dystrophies, with a PR interval greater than 240 ms and LBBB, permanent pacing, with additional defibrillator capability if needed and meaningful survival of greater than 1 year is expected, is reasonable''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: B-NR]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
'''7.'''In patients with marked first-degree or second-degree Mobitz type I (Wenckebach) atrioventricular block with symptoms that are clearly attributable to the | |||
atrioventricular block, permanent pacing is reasonable''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
'''8.'''In patients with neuromuscular diseases, such as myotonic dystrophy type 1, with a PR interval greater than 240 ms, a QRS duration greater than 120 ms, or fascicular block,permanent pacing, with additional defibrillator capability if needed and meaningful survival of greater than 1 year is expected, may be considered''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' | |||
|} | |||
==Treatment for Reflex Syncope== | |||
*Once a diagnosis of '''[[Extrinsic vagal paroxysmal AV block]]''' has been made, the following guidelines may be helpful ; | |||
[[Image:Treatment of Reflex Syncope.JPG|thumb|center|500px| Treatment of Reflex Syncope-{{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}}]] | |||
[[Image:Counter Pressure Maneuvers.JPG|thumb|center|500px| Counter Pressure Maneuvers-{{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}}]] | |||
==References== | ==References== | ||
Latest revision as of 06:58, 11 July 2020
|
Paroxysmal AV block Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Paroxysmal AV block interventions On the Web |
|
American Roentgen Ray Society Images of Paroxysmal AV block interventions |
|
Risk calculators and risk factors for Paroxysmal AV block interventions |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akash Daswaney, M.B.B.S[2]
Overview
Several studies have demonstrated the efficacy of cardiac pacing in paroxysmal AV block. Temporary pacing should be used for the minimum duration necessary to prevent hemodynamic compromise and asystole. The presence or absence of symptoms and the correlation of those symptoms with a conduction defect is an important determinant of cardiac pacing. An improvement in conduction suggests that the level of the block is at the level of the AV node. Counterpressure maneuvers may be helpful in preventing vagally mediated syncope.
European Society of Cardiology : Indications for Cardiac Pacing

- The major factors predicting the efficacy of pacing in preventing syncope recurrence are an established relationship between symptoms and bradycardia and the absence of associated hypotensive susceptibility .
- When this relationship is less established, or some hypotensive mechanism is present, syncope can recur in a minority of patients.
- Pacing is not indicated in unexplained syncope without evidence of any conduction disturbance.
- Less than half of the patients with bifascicular BBB and syncope have a final diagnosis of cardiac syncope, albeit the probability is different among the types of BBB.
- Elderly patients with bifascicular BBB and unexplained syncope after a reasonable workup might benefit from empirical pacemaker implantation,especially if syncope is unpredictable (with no or short prodromes) or has occurred in the supine position or during effort. "ESC Guidelines on Syncope (Diagnosis and Management of)".
- Milena et al conducted a 4 year study to study the efficacy of cardiac pacing in patients with documented paroxysmal AV block.
- The endpoints of the study focused on syncope recurrence and time taken till first recurrence of presyncope.
- Recurrence was only seen in patients without structural heart disease and the mechanism was related to hypotension, onset of atrial fibrillation or reflex mediated.
- Significantly lower recurrence rates were seen in patients with documented paroxysmal AV block and it was also concluded that cardiac pacing could be offered more confidently to patients with structural heart disease."Syncope in patients paced for atrioventricular block. | Semantic Scholar".
- The Syncope Unit Project -2 (SUP-2 ) studied carried about by Brignole et al included patients with a history of recurrent syncope and positive findings on carotid sinus massage/ tilt table testing/ implantable loop recorders.
- Such patients were fitted with dual chamber pacemakers and recurrence rates were followed up.
- Using a standardized algorithm in their approach, they came to the conclusion that pacing can be can be offered to patients with positive findings on carotid sinus massage/ tilt table testing/ implantable loop recorders.
- An efficacy of 3 years was maintained.
- Furthermore, similar results were also found in those with intrinsic paroxysmal AV block patients and in tilt table positive asystolic reflex syncope patients.[1]
- The ISSUE 3 study also produced similar results where TT- negative asystolic reflex syncope patients were concerned.
2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay
Temporary Pacing
| Recommendations for Temporary Pacing for Bradycardia Attributable to Atrioventricular Block |
| "1. For patients with second-degree or third-degree atrioventricular block associated with symptoms or hemodynamic compromise that
is refractory to medical therapy, temporary transvenous pacing is reasonable to increase heart rate and improve symptoms. (Level of Evidence: B-NR)[2] 2.For patients who require prolonged temporary transvenous pacing, it is reasonable to choose an externalized permanent active fixation lead over a standard passive fixation temporary pacing lead.(Level of Evidence: B-NR)]])[2] 3. For patients with second-degree or third-degree atrioventricular block and hemodynamic compromise refractory to antibradycardic medical therapy, temporary transcutaneous pacing may be considered until a temporary transvenous or PPM is placed or the bradyarrhythmia resolves.(Level of Evidence: B-R)[2] " |
- Temporary pacing is a process that requires careful consideration where timing and necessity is concerned.
- It should be used for the minimum duration necessary to prevent hemodynamic compromise and asystole.
- Increased safety has been noted when prolonged temporary pacing is done with an externalized active fixation permanent pacing. [2]
Chronic Therapy/Management of Bradycardia Attributable to Atrioventricular Block

| Recommendations for General Principles of Chronic Therapy/Management of Bradycardia Attributable to Atrioventricular Block |
| "1. In patients with first-degree atrioventricular block or second-degree Mobitz type I (Wenckebach) or 2:1 atrioventricular block which is believed to be at the level of the atrioventricular node, with symptoms that do not temporally correspond to the atrioventricular block, permanent pacing should not be performed. (Level of Evidence: C-LD[2]
2.In asymptomatic patients with first-degree atrioventricular block or second-degree Mobitz type I (Wenckebach) or 2:1 atrioventricular block which is believed to be at the level of the atrioventricular node, permanent pacing should not be performed.(Level of Evidence: C-LD)[2] |
- The presence or absence of symptoms is a major determinant on whether permanent pacing will be required in the setting of bradycardia associated with atrioventricular block.
- Improvement in atrioventricular conduction suggests that the site of block is at the atrioventricular node, whereas worsening atrioventricular conduction suggests infranodal block. If the symptoms do not clearly correspond to the episodes of atrioventricular block, the risks associated with the pacemaker in the absence of clear benefit make the overall risk-benefit ratio unfavorable.
- If the level of the block is at the atrioventricular node, then sudden progression to a higher degree of atrioventricular block is unlikely.
- Given the procedural and long-term risks of PPMs, in the absence of mitigating circumstances, for patients with first-degree or second-degree Mobitz type I (Wenckebach) atrioventricular block that does not clearly correspond to symptoms, further monitoring and follow up should be implemented.
Permanent Pacing
| Recommendations for Permanent Pacing for Chronic Therapy/Management of Bradycardia Attributable to Atrioventricular Block |
| "' 1. In patients with acquired second-degree Mobitz type II atrioventricular block, highgrade atrioventricular block, or third-degree
atrioventricular block not attributable to reversible or physiologic causes, permanent pacing is recommended regardless of symptoms.(Level of Evidence: B-NR)[2] 2. In patients with neuromuscular diseases associated with conduction disorders, including muscular dystrophy (eg,myotonic dystrophy type 1) or Kearns-Sayre syndrome, who have evidence of seconddegree atrioventricular block, third-degree atrioventricular block, or an HV interval of 70 ms or greater, regardless of symptoms, permanent pacing, with additional defibrillator capability if needed and meaningful survival of greater than 1 year is expected, is recommended(Level of Evidence: B-NR)[2] 3. In patients with permanent AF and symptomatic bradycardia, permanent pacing is recommended.(Level of Evidence: C-LD)[2] 4.In patients who develop symptomatic atrioventricular block as a consequence of guideline-directed management and therapy for which there is no alternative treatment and continued treatment is clinically necessary, permanent pacing is recommended to increase heart rate and improve symptoms(Level of Evidence: C-LD)[2] 5.In patients with an infiltrative cardiomyopathy, such as cardiac sarcoidosis or amyloidosis, and seconddegree Mobitz type II atrioventricular block,high-grade atrioventricular block, or thirddegree atrioventricular block, permanent pacing, with additional defibrillator capability if needed and meaningful survival of greater than 1 year is expected,is reasonable(Level of Evidence: B-NR)[2] 6.In patients with lamin A/C gene mutations,including limb-girdle and Emery-Dreifuss muscular dystrophies, with a PR interval greater than 240 ms and LBBB, permanent pacing, with additional defibrillator capability if needed and meaningful survival of greater than 1 year is expected, is reasonable(Level of Evidence: B-NR)[2] 7.In patients with marked first-degree or second-degree Mobitz type I (Wenckebach) atrioventricular block with symptoms that are clearly attributable to the atrioventricular block, permanent pacing is reasonable(Level of Evidence: C-LD)[2] 8.In patients with neuromuscular diseases, such as myotonic dystrophy type 1, with a PR interval greater than 240 ms, a QRS duration greater than 120 ms, or fascicular block,permanent pacing, with additional defibrillator capability if needed and meaningful survival of greater than 1 year is expected, may be considered(Level of Evidence: C-LD)[2] |
Treatment for Reflex Syncope
- Once a diagnosis of Extrinsic vagal paroxysmal AV block has been made, the following guidelines may be helpful ;


References
- ↑ Brignole M, Arabia F, Ammirati F, Tomaino M, Quartieri F, Rafanelli M; et al. (2016). "Standardized algorithm for cardiac pacing in older patients affected by severe unpredictable reflex syncope: 3-year insights from the Syncope Unit Project 2 (SUP 2) study". Europace. 18 (9): 1427–33. doi:10.1093/europace/euv343. PMID 26612880.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR; et al. (2019). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society". J Am Coll Cardiol. 74 (7): 932–987. doi:10.1016/j.jacc.2018.10.043. PMID 30412710.