Hepatoblastoma overview: Difference between revisions
Nima Nasiri (talk | contribs) |
Aditya Ganti (talk | contribs) |
||
| (24 intermediate revisions by 2 users not shown) | |||
| Line 7: | Line 7: | ||
==Historical Perspective== | ==Historical Perspective== | ||
In 1898, the first case of hepatoblastoma was published in English literature, the [[tumor]] was diagnosed in a 6-week old boy in Prague, by a physician named Misick, who found a large tumor on the [[autopsy]] of his [[liver]]. Decades later on 1962 Willis used the term, hepatoblastoma for this type of [[liver]] [[tumor]] because of it's [[Embryo|embryonal]] origin | |||
==Classification== | ==Classification== | ||
Hepatoblastoma can be divided into major and minor categories based on histology. Major categories constitutes epithelial, small cell undifferentiated and rhabdoid while minor constitutes cholangioblastic (ductal), keratinising squamous epithelium, intestinal glandular epithelium, teratoid (neuroid-melanocytic), rhabdomyoblastic, chondroid, and osteoid. | |||
* | |||
* | |||
==Pathophysiology== | ==Pathophysiology== | ||
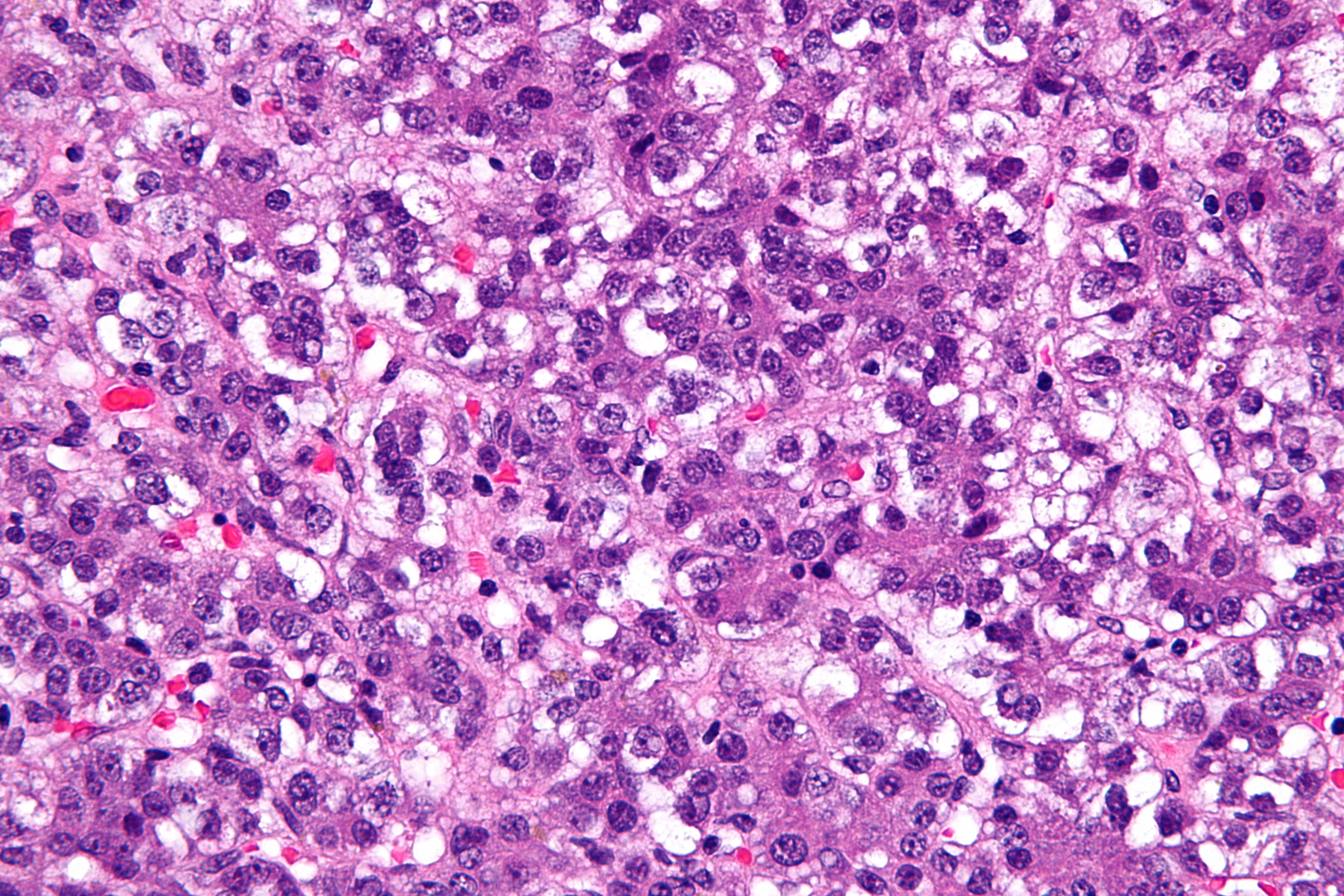
Development of hepatoblastoma is the result of multiple genetic mutations. Genes involved in the pathogenesis of hepatoblastoma include ''[[Beta-catenin|CTNNB1]]'', ''CAPRIN2'', ''[[SPOP]]'', ''[[OR5I1]]'', and ''CDC20B''. On gross pathology, hepatoblastoma is characterized by a solitary, large, well circumscribed mass with heterogeneous cut surface. On microscopic histopathological analysis, hepatoblastoma is characterized by small round cell tumor, fetal hepatocytes ~ 1:3 nuclear-cytoplasmic ratio, eosinophilic cytoplasm (mesenchymal component), and immature fibrous tissue osteoid or cartilage. Hepatoblastoma is demonstrated by positivity to [[alpha-fetoprotein]], hepatocyte specific antigen (especially in fetal component), and beta-catenin (cytoplasmic and nuclear).[[File:Hepatoblastoma.jpg|300x300px|thumb|Hepatoblastoma H&E[https://commons.wikimedia.org/wiki source:wikipedia]|center]]<br style="clear:left" /> | |||
[[File:Hepatoblastoma.jpg| | |||
==Causes== | ==Causes== | ||
There are no specific causes of hepatoblastoma and most tumors are sporadic but there are some [[Hepatoblastoma risk factors|risk factors]] and conditions that have a strong association with this [[tumor]] such as [[Beckwith-Weidemann Syndrome|beckwith-Weidemann syndrome]], [[familial adenomatous polyposis]] (FAP), [[down syndrome]], [[Edward's syndrome|edward syndrome]] ([[trisomy 18]]). | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
Hepatoblastoma is a common tumor that tends to affect children aged less than five years. Males are more commonly affected with hepatoblastoma than females. The annual [[incidence]] of hepatoblastoma in the United States appears to have doubled from 8 (1975-1983) to 16 (2002-2009) per 100,000 children aged 19 years and younger. | |||
==Risk factors== | ==Risk factors== | ||
Common risk factors in the development of hepatoblastoma include [[Low birth weight]] infants, [[Preeclampsia]], [[Fetal distress]], [[Premature labor]], [[Chromosomal anomalies]] such as [[Down syndrome]], [[Edwards syndrome]]. parental [[tobacco]] [[smoking]] before and during [[pregnancy]], [[Oxygen therapy]], certain medication ([[furosemide]]), [[Total parenteral nutrition]] ([[TPN]]). | |||
==Screening== | ==Screening== | ||
According to the American Association for the Study of Liver Diseases and United States Preventive Services Task Force, there is insufficient evidence to recommend routine screening for hepatoblastoma | According to the American Association for the Study of Liver Diseases and United States Preventive Services Task Force, there is insufficient evidence to recommend routine screening for hepatoblastoma. However, [[ultrasound]] is the recommended for suspected [[hepatic]] lesions in children. | ||
==Differentiating Hepatoblastoma from other diseases== | ==Differentiating Hepatoblastoma from other diseases== | ||
Hepatoblastoma must be differentiated from other diseases such as [[Hamartoma|hepatic mesenchymal hamartoma]], [[hepatocellular carcinoma]], [[Hepatocellular carcinoma|hepatic metastases]], [[infantile hemangioendothelioma]], and [[Rhabdomyosarcoma|rhabdomyosarcoma of biliary tract]]. | Hepatoblastoma must be differentiated from other diseases such as [[Hamartoma|hepatic mesenchymal hamartoma]], [[hepatocellular carcinoma]], [[Hepatocellular carcinoma|hepatic metastases]], [[infantile hemangioendothelioma]], and [[Rhabdomyosarcoma|rhabdomyosarcoma of biliary tract]]. | ||
==Natural History, Complications and Prognosis== | ==Natural History, Complications and Prognosis== | ||
If left untreated, patients with hepatoblastoma may progress to develop [[failure to thrive]], [[weight loss]], spontaneous rupture, hemorrhage | |||
If left untreated, patients with hepatoblastoma may progress to develop [[failure to thrive]], [[weight loss]], [[Abdominal mass|rapidly enlarging abdominal mass]], spontaneous rupture, [[hemorrhage]]. Common complications of hepatoblastoma include paraneoplastic features, [[erythrocytosis]], [[thrombocytosis]], [[hypocalcemia]], [[Precocious puberty|isosexual precocious puberty]], and [[hypoglycemia]]. The 5-year survival rate of children with hepatoblastoma is approximately 70%. | |||
==Diagnosis== | ==Diagnosis== | ||
=== | ===Diagnostic study of choice=== | ||
The | The diagnosis of hepatoblastoma is made when [[abdominal mass]] is detected on [[ultrasound]] or [[spiral CT scan]], but a definitive diagnosis requires the histological evaluation of [[biopsy]] specimen after surgery. | ||
=== Screening === | |||
The staging of hepatoblastoma is based on the Intergroup staging system. | |||
===History and Symptoms=== | ===History and Symptoms=== | ||
The majority of patients with hepatoblastoma have an [[abdominal mass]] or [[abdominal distension]]. Other symptoms include [[abdominal pain]], [[weight loss]], [[loss of appetite]], early [[puberty]] in boys, [[jaundice]], [[nausea]], [[vomiting]], [[back pain]], [[failure to thrive]], and [[Abdominal mass|rapidly enlarging abdominal mass]]. | |||
===Physical examination=== | ===Physical examination=== | ||
Common physical examination findings of hepatoblastoma include [[hepatomegaly]], [[abdominal distension]], [[Abdominal mass|asymptomatic palpable abdominal mass]], [[hemihypertrophy]], [[jaundice]], [[pyrexia]], and [[anemia]]. | Common physical examination findings of hepatoblastoma include [[hepatomegaly]], [[abdominal distension]], [[Abdominal mass|asymptomatic palpable abdominal mass]], [[hemihypertrophy]], [[jaundice]], [[pyrexia]], and [[anemia]]. | ||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
Laboratory tests for liver function are usually normal. An elevated concentration of [[alpha-fetoprotein]] is present in patients with hepatoblastoma. | Laboratory tests for liver function are usually normal among patients. An elevated concentration of [[alpha-fetoprotein]] is present in patients with hepatoblastoma. | ||
===Xray=== | ===Xray=== | ||
Findings on abdominal xray are nonspecific for hepatoblastoma and include [[Abdominal mass|right upper quadrant abdominal mass]] and/or calcifications in 10% of cases. | Findings on abdominal xray are nonspecific for hepatoblastoma and include [[Abdominal mass|right upper quadrant abdominal mass]] and/or calcifications in 10% of cases. [[Chest-X-Ray|Chest]] [[Chest X-ray|x-rays]] can be useful especially since this [[tumor]] has the affinity to [[metastasize]] to [[lungs]]. | ||
===CT=== | ===CT=== | ||
Abdominal | Abdominal CT scan may be helpful in the diagnosis of hepatoblastoma. Findings on CT scan suggestive of hepatoblastoma include well defined heterogeneous mass, frequent areas of necrosis and hemorrhage, and chunky dense calcifications. | ||
===MRI=== | ===MRI=== | ||
[[MRI]] has the advantage of multiplanar [[soft-tissue]] characterization, lack of harmful [[ionizing radiation]] and when [[diffusion-weighted imaging]] techniques are used, [[MRI]] is exquisitely sensitive for detecting tiny [[liver]] lesions. | |||
===Ultrasound=== | ===Ultrasound=== | ||
[[ | Imaging studies play an important role in the diagnosis, [[Staging (pathology)|staging]], and treatment of disease, most tumors can be resected surgically and [[ultrasound]] is often used in order to detect [[tumor]] size, also the initial diagnosis is made by [[abdominal]] [[ultrasound]]. Findings on ultrasound suggestive of hepatoblastoma include echogenic soft tissue mass, well defined lesion, and areas of shadowing due to intralesional calcifications. | ||
===Biopsy=== | ===Biopsy=== | ||
Biopsy is the gold standard for the diagnosis of hepatoblastoma. | Biopsy is the gold standard for the diagnosis of hepatoblastoma. | ||
===Other Imaging Findings=== | |||
Other imaging studies such as [[PET scan]] or even [[bone scan]] when there is evidence of [[metastasis]] to [[bone]] may be helpful in the diagnosis of hepatoblastoma. PET scan can be helpful in localizing recurrent hepatoblastoma. | |||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
The | The mainstay of therapy for hepatoblastoma is [[Surgery|surger]]<nowiki/>y. However, the vast majority of the tumors cannot be completely resected because of their large size or [[metastasis]]. [[Chemotherapy]] is an important [[adjuvant therapy]], and [[cisplatin]] is the most commonly used [[chemotherapeutic agent]], it can reduce the volume of [[tumors]] that are too big for surgical removal. | ||
===Surgery=== | ===Surgery=== | ||
Surgery is the mainstay of treatment for hepatoblastoma. | [[Surgery]] is the mainstay of treatment for hepatoblastoma. Liver [[transplantation]] can be considered for [[tumors]] that cannot be removed by surgery. The feasibility of [[surgery]] depends on the resectability of [[tumor]] at diagnosis. | ||
===Primary Prevention=== | ===Primary Prevention=== | ||
There are no primary preventive measures available for hepatoblastoma. | There are no primary preventive measures available for hepatoblastoma. | ||
===Secondary Prevention=== | ===Secondary Prevention=== | ||
Effective measures for the secondary prevention of hepatoblastoma include use of abdominal ultrasound and alpha-fetoprotein levels in patients with [[Beckwith-Wiedemann syndrome]] or isolated hemihyperplasia. | Effective measures for the secondary prevention of hepatoblastoma include use of abdominal [[ultrasound]] and [[alpha-fetoprotein]] levels in patients with [[Beckwith-Wiedemann syndrome]] or isolated hemihyperplasia. | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Gastroenterology]] | |||
[[Category:Surgery]] | |||
[[Category:Hepatology]] | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
Latest revision as of 21:32, 13 March 2019
|
Hepatoblastoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hepatoblastoma overview On the Web |
|
American Roentgen Ray Society Images of Hepatoblastoma overview |
|
Risk calculators and risk factors for Hepatoblastoma overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Nawal Muazam M.D.[2]
Overview
Hepatoblastoma is the most common primary liver tumor occurs in infant and children, usually less than 3 years old, more frequently in male, and accounting for over 1% of pediatric cancers. The etiology is unknown and not well understood, but it has been associated with Beckwith-Weidemann syndrome, familial adenomatous polyposis, and other factors such as low birth weight, preeclampsia, hemihypertrophy. The primary treatment is surgical resection, however, chemotherapy plays an important role by increasing the number of tumors that are respectable, chemotherapeutic agents helps in shrinkage of the tumor and make it easier to be resected by surgery. Prognosis of the tumor depends on various criteria such as resectability of the tumor, distant metastasis, tumor size, PRETEXT staging, and recurrence of the tumor. The mainstay of treatment is surgery, but the adjuvant chemotherapeutic agents and liver transplantation also are helpful.
Historical Perspective
In 1898, the first case of hepatoblastoma was published in English literature, the tumor was diagnosed in a 6-week old boy in Prague, by a physician named Misick, who found a large tumor on the autopsy of his liver. Decades later on 1962 Willis used the term, hepatoblastoma for this type of liver tumor because of it's embryonal origin
Classification
Hepatoblastoma can be divided into major and minor categories based on histology. Major categories constitutes epithelial, small cell undifferentiated and rhabdoid while minor constitutes cholangioblastic (ductal), keratinising squamous epithelium, intestinal glandular epithelium, teratoid (neuroid-melanocytic), rhabdomyoblastic, chondroid, and osteoid.
Pathophysiology
Development of hepatoblastoma is the result of multiple genetic mutations. Genes involved in the pathogenesis of hepatoblastoma include CTNNB1, CAPRIN2, SPOP, OR5I1, and CDC20B. On gross pathology, hepatoblastoma is characterized by a solitary, large, well circumscribed mass with heterogeneous cut surface. On microscopic histopathological analysis, hepatoblastoma is characterized by small round cell tumor, fetal hepatocytes ~ 1:3 nuclear-cytoplasmic ratio, eosinophilic cytoplasm (mesenchymal component), and immature fibrous tissue osteoid or cartilage. Hepatoblastoma is demonstrated by positivity to alpha-fetoprotein, hepatocyte specific antigen (especially in fetal component), and beta-catenin (cytoplasmic and nuclear).
Causes
There are no specific causes of hepatoblastoma and most tumors are sporadic but there are some risk factors and conditions that have a strong association with this tumor such as beckwith-Weidemann syndrome, familial adenomatous polyposis (FAP), down syndrome, edward syndrome (trisomy 18).
Epidemiology and Demographics
Hepatoblastoma is a common tumor that tends to affect children aged less than five years. Males are more commonly affected with hepatoblastoma than females. The annual incidence of hepatoblastoma in the United States appears to have doubled from 8 (1975-1983) to 16 (2002-2009) per 100,000 children aged 19 years and younger.
Risk factors
Common risk factors in the development of hepatoblastoma include Low birth weight infants, Preeclampsia, Fetal distress, Premature labor, Chromosomal anomalies such as Down syndrome, Edwards syndrome. parental tobacco smoking before and during pregnancy, Oxygen therapy, certain medication (furosemide), Total parenteral nutrition (TPN).
Screening
According to the American Association for the Study of Liver Diseases and United States Preventive Services Task Force, there is insufficient evidence to recommend routine screening for hepatoblastoma. However, ultrasound is the recommended for suspected hepatic lesions in children.
Differentiating Hepatoblastoma from other diseases
Hepatoblastoma must be differentiated from other diseases such as hepatic mesenchymal hamartoma, hepatocellular carcinoma, hepatic metastases, infantile hemangioendothelioma, and rhabdomyosarcoma of biliary tract.
Natural History, Complications and Prognosis
If left untreated, patients with hepatoblastoma may progress to develop failure to thrive, weight loss, rapidly enlarging abdominal mass, spontaneous rupture, hemorrhage. Common complications of hepatoblastoma include paraneoplastic features, erythrocytosis, thrombocytosis, hypocalcemia, isosexual precocious puberty, and hypoglycemia. The 5-year survival rate of children with hepatoblastoma is approximately 70%.
Diagnosis
Diagnostic study of choice
The diagnosis of hepatoblastoma is made when abdominal mass is detected on ultrasound or spiral CT scan, but a definitive diagnosis requires the histological evaluation of biopsy specimen after surgery.
Screening
The staging of hepatoblastoma is based on the Intergroup staging system.
History and Symptoms
The majority of patients with hepatoblastoma have an abdominal mass or abdominal distension. Other symptoms include abdominal pain, weight loss, loss of appetite, early puberty in boys, jaundice, nausea, vomiting, back pain, failure to thrive, and rapidly enlarging abdominal mass.
Physical examination
Common physical examination findings of hepatoblastoma include hepatomegaly, abdominal distension, asymptomatic palpable abdominal mass, hemihypertrophy, jaundice, pyrexia, and anemia.
Laboratory Findings
Laboratory tests for liver function are usually normal among patients. An elevated concentration of alpha-fetoprotein is present in patients with hepatoblastoma.
Xray
Findings on abdominal xray are nonspecific for hepatoblastoma and include right upper quadrant abdominal mass and/or calcifications in 10% of cases. Chest x-rays can be useful especially since this tumor has the affinity to metastasize to lungs.
CT
Abdominal CT scan may be helpful in the diagnosis of hepatoblastoma. Findings on CT scan suggestive of hepatoblastoma include well defined heterogeneous mass, frequent areas of necrosis and hemorrhage, and chunky dense calcifications.
MRI
MRI has the advantage of multiplanar soft-tissue characterization, lack of harmful ionizing radiation and when diffusion-weighted imaging techniques are used, MRI is exquisitely sensitive for detecting tiny liver lesions.
Ultrasound
Imaging studies play an important role in the diagnosis, staging, and treatment of disease, most tumors can be resected surgically and ultrasound is often used in order to detect tumor size, also the initial diagnosis is made by abdominal ultrasound. Findings on ultrasound suggestive of hepatoblastoma include echogenic soft tissue mass, well defined lesion, and areas of shadowing due to intralesional calcifications.
Biopsy
Biopsy is the gold standard for the diagnosis of hepatoblastoma.
Other Imaging Findings
Other imaging studies such as PET scan or even bone scan when there is evidence of metastasis to bone may be helpful in the diagnosis of hepatoblastoma. PET scan can be helpful in localizing recurrent hepatoblastoma.
Treatment
Medical Therapy
The mainstay of therapy for hepatoblastoma is surgery. However, the vast majority of the tumors cannot be completely resected because of their large size or metastasis. Chemotherapy is an important adjuvant therapy, and cisplatin is the most commonly used chemotherapeutic agent, it can reduce the volume of tumors that are too big for surgical removal.
Surgery
Surgery is the mainstay of treatment for hepatoblastoma. Liver transplantation can be considered for tumors that cannot be removed by surgery. The feasibility of surgery depends on the resectability of tumor at diagnosis.
Primary Prevention
There are no primary preventive measures available for hepatoblastoma.
Secondary Prevention
Effective measures for the secondary prevention of hepatoblastoma include use of abdominal ultrasound and alpha-fetoprotein levels in patients with Beckwith-Wiedemann syndrome or isolated hemihyperplasia.