Testosterone (nasal)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Turky Alkathery, M.D. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Testosterone (nasal) is a steroid hormone from the androgen group that is FDA approved for the treatment of deficiency or absence of endogenous testosterone. Common adverse reactions include PSA increased, headache, rhinorrhea, epistaxis, nasal discomfort, nasopharyngitis, bronchitis, upper respiratory tract infection, sinusitis, and nasal scab.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- Testosterone is indicated for replacement therapy in adult males for conditions associated with a deficiency or absence of endogenous testosterone.
- Primary hypogonadism (congenital or acquired): testicular failure due to conditions such as cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchiectomy, Klinefelter’s syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. These men usually have low serum testosterone concentrations and gonadotropins (follicle-stimulating hormone [FSH], luteinizing hormone [LH]) above the normal range.
- Hypogonadotropic hypogonadism (congenital or acquired): idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. These men have low testosterone serum concentrations but have gonadotropins in the normal or low range.
- Limitations of use:
- Safety and efficacy of testosterone in males less than 18 years old have not been established.
Dosage
Dosing
- The recommended dose of testosterone is 11 mg of testosterone (2 pump actuations; 1 actuation per nostril) administered intranasally three times daily for a total daily dose of 33 mg.
- Serum total testosterone concentrations should be checked periodically, starting as soon as one month after initiating treatment with testosterone. When the total testosterone concentration consistently exceeds 1050 ng/dL, therapy with testosterone should be discontinued. If the total testosterone concentration is consistently below 300 ng/dL, an alternative treatment should be considered.
Administration Instructions
- Testosterone is administered intranasally three times daily once in the morning, once in the afternoon and once in the evening (6 to 8 hours apart), preferably at the same time each day. Patients should be instructed to completely depress the pump 1 time in each nostril to receive the total dose. Do not administer testosterone to other parts of the body.

Use with Nasally Administered Drugs Other Than Sympathomimetic Decongestants
- The drug interaction potential between testosterone and nasally administered drugs other than sympathomimetic decongestants is unknown. Therefore, testosterone is not recommended for use with nasally administered drugs other than sympathomimetic decongestants (e.g., oxymetazoline).
Temporary Discontinuation of Use for Severe Rhinitis
- If the patient experiences an episode of severe rhinitis, temporarily discontinue testosterone therapy pending resolution of the severe rhinitis symptoms. If the severe rhinitis symptoms persist, an alternative testosterone replacement therapy is recommended.
Dosage Forms and Strengths
- Testosterone is a slightly yellow gel for intranasal use and is available in a dispenser with a metered dose pump. One pump actuation delivers 5.5 mg of testosterone.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Testosterone (nasal) in adult patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Testosterone (nasal) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- Safety and efficacy of testosterone has not been established in pediatric patients less than 18 years of age. Improper use may result in acceleration of bone age and premature closure of epiphyses.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Testosterone (nasal) in pediatric patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Testosterone (nasal) in pediatric patients.
Contraindications
- Testosterone is contraindicated in men with carcinoma of the breast or known or suspected carcinoma of the prostate.
- Testosterone is contraindicated in women who are or who may become pregnant, or who are breast- feeding. Testosterone may cause fetal harm when administered to a pregnant woman. Testosterone may cause serious adverse reactions in nursing infants. Exposure of a fetus or nursing infant to androgens may result in varying degrees of virilization. If a pregnant woman is exposed to testosterone, she should be apprised of the potential hazard to the fetus.
Warnings
Nasal Adverse Reactions and Limited Long-Term Information on Nasal Safety
- Nasal adverse reactions, including nasopharyngitis, rhinorrhea, epistaxis, nasal discomfort and nasal scabbing, were reported in the clinical trial experience with testosterone. All nasal adverse reactions except one (a single case of upper respiratory infection) were reported as mild or moderate in severity; however, long-term clinical trial data on nasal safety is available in a limited number of subjects. Patients should be instructed to report any nasal symptoms or signs to their health care professional. In that circumstance, health care professionals should determine whether further evaluation (e.g., otorhinolaryngology consultation) or discontinuation of testosterone is appropriate.
Use in Patients with Chronic Nasal Conditions and Alterations in Nasal Anatomy
- Due to lack of clinical data on the safety or efficacy, testosterone is not recommended for use in the following patients:
- History of nasal disorders;
- History of nasal or sinus surgery;
- History of nasal fracture within the previous 6 months or nasal fracture that caused a deviated anterior nasal septum;
- Mucosal inflammatory disorders (e.g, Sjogren’s syndrome); and
- Sinus disease.
Worsening of Benign Prostatic Hyperplasia and Potential Risk of Prostate Cancer
- Patients with BPH treated with androgens are at an increased risk for worsening of signs and symptoms of BPH. Monitor patients with BPH for worsening signs and symptoms.
- Patients treated with androgens may be at increased risk for prostate cancer. Evaluate patients for prostate cancer prior to initiating treatment. It would be appropriate to re-evaluate patients 3 to 6 months after initiation of treatment and then in accordance with prostate cancer screening practices.
Polycythemia
- Increases in hematocrit, reflective of increases in red blood cell mass, may require discontinuation of testosterone . Check hematocrit prior to initiating testosterone treatment. It would be appropriate to re-evaluate the hematocrit 3 to 6 months after starting testosterone treatment, and then annually. If hematocrit becomes elevated, stop therapy until hematocrit decreases to an acceptable level. An increase in red blood cell mass may increase the risk of thromboembolic events.
Venous Thromboembolism
- There have been postmarketing reports of venous thromboembolic events , including deep vein thrombosis (DVT) and pulmonary embolism (PE), in patients using testosterone products such as testosterone. Evaluate patients who report symptoms of pain, edema, warmth and erythema in the lower extremity for (DVT) and those who present with acute shortness of breath for PE. If a venous thromboembolic event is suspected, discontinue treatment with testosterone and initiate appropriate workup and management.
Use in Women
- Due to lack of controlled studies in women and potential virilizing effects, testosterone is not indicated for use in women.
Potential for Adverse Effects on Spermatogenesis
- With large doses of exogenous androgens, including testosterone, spermatogenesis may be suppressed through feedback inhibition of pituitary follicle-stimulating hormone (FSH), which could possibly lead to adverse effects on semen parameters, including sperm count.
Hepatic Adverse Effects
- Prolonged use of high doses of orally active 17-alpha-alkyl androgens (methyltestosterone) has been associated with serious hepatic adverse effects (peliosis hepatitis, hepatic neoplasms, cholestatic hepatitis, and jaundice). Peliosis hepatitis can be a life-threatening or fatal complication. Long-term therapy with intramuscular testosterone enanthate has produced multiple hepatic adenomas. Testosterone is not known to cause these adverse effects. Nonetheless, patients should be instructed to report any signs or symptoms of hepatic dysfunction (e.g., jaundice). If these occur, promptly discontinue testosterone while the cause is evaluated.
Edema
- Androgens, including testosterone, may promote retention of sodium and water. Edema, with or without congestive heart failure, may be a serious complication in patients with pre-existing cardiac, renal, or hepatic disease. In addition to discontinuation of the drug, diuretic therapy may be required.
Gynecomastia
- Gynecomastia may develop and may persist in patients being treated with androgens, including testosterone, for hypogonadism.
Sleep Apnea
- The treatment of hypogonadal men with testosterone may potentiate sleep apnea in some patients, especially those with risk factors such as obesity and chronic lung disease.
Lipids
- Changes in the serum lipid profile may occur. Monitor the lipid profile periodically, particularly after starting testosterone therapy. Changes in serum lipid profile may require discontinuation of testosterone therapy.
Hypercalcemia
- Androgens, including testosterone, should be used with caution in cancer patients at risk of hypercalcemia (and associated hypercalciuria). Regular monitoring of serum calcium concentrations is recommended in these patients.
Decreased Thyroxine-binding Globulin
- Androgens, including testosterone, may decrease concentrations of thyroxine-binding globulins, resulting in decreased total T4 serum concentrations and increased resin uptake of T3 and T4. Free thyroid hormone concentrations remain unchanged; however, and there is no clinical evidence of thyroid dysfunction.
Drug Abuse and Dependence
Controlled Substance
- Testosterone contains testosterone, a Schedule III controlled substance in the Controlled Substances Act.
Abuse
- Anabolic steroids, such as testosterone, are abused. Abuse is often associated with adverse physical and psychological effects.
Dependence
- Although drug dependence is not documented in individuals using therapeutic doses of anabolic steroids for approved indications, dependence is observed in some individuals abusing high doses of anabolic steroids. In general, anabolic steroid dependence is characterized by any three of the following:
- Taking more drug than intended
- Continued drug use despite medical and social problems
- Significant time spent in obtaining adequate amounts of drug
- Desire for anabolic steroids when supplies of the drug are interrupted
- Difficulty in discontinuing use of the drug despite desires and attempts to do so
- Experience of withdrawal syndrome upon discontinuation of anabolic steroid use
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- Testosterone was evaluated in a multicenter, open-label, 90-day clinical study. Patients could continue treatment with testosterone in two, open-label extension periods for an additional 90 and 180 days, respectively. A total of 306 hypogonadal men with morning testosterone concentrations ≤ 300 ng/dL received testosterone. Of these, 78 received testosterone at a dose of 11 mg three times daily.
90-Day Clinical Study
- Among the 78 patients who received testosterone three times daily in the 90-day clinical study, the most common adverse reactions were: prostate specific antigen (PSA) increased, headache, rhinorrhea, epistaxis, nasal discomfort, nasopharyngitis, upper respiratory tract infection (URI), sinusitis, bronchitis and nasal scab. PSA increased was considered an adverse reaction by meeting one of two pre-specified criteria: (1) increase from baseline serum PSA greater than 1.4 ug/L, or (2) serum PSA greater than 4.0 ug/L.
- Table 1 shows adverse reactions reported by ≥3% of patients treated with 11 mg three times daily in the 90-day clinical study.

- Adverse reactions reported by >2% but <3% of patients in the 90-day clinical study include:
- blood pressure increased, dysgeusia, nasal dryness, nasal congestion, and cough.
Extension Periods
- Among the 78 patients who received testosterone three times daily in the 90-day clinical study, a total of 69 patients received testosterone three times daily in the first 90-day extension period. Among these 69 patients, the most common adverse reactions were: nasopharyngitis, PSA increased, parosmia, nasal discomfort, rhinorrhea and nasal scab.
- Table 2 shows adverse reactions reported by ≥3% of patients who received testosterone three times daily in both the 90-day clinical study and in the 90-day extension period.

- A total of 18 patients received testosterone three times daily in all three treatment periods, including the 90-day clinical study, the first 90-day extension period, and the second 180-day extension period. Among these 18 patients, the following adverse reactions were reported in more than one patient each: nasopharyngitis, parosmia, PSA increased, nasal discomfort, nasal scab and hypertension. The following adverse reactions were reported in one patient each: nausea, nasal excoriation, thyroid stimulating hormone increased, decreased appetite, myalgia, anosmia, testicular atrophy, epistaxis, nasal septum disorder, nasal discomfort, and rhinorrhea.
- In patients who received testosterone three times daily, mean serum PSA concentrations increased by 0.2 ng/mL, 0.1 ng/mL, and 0.2 ng/mL after 90, 180 and 360 days, respectively.
Discontinuations due to Adverse Reactions
- Among all subjects (n=306) who received testosterone at any dose in the 90-day clinical study and its 90- and 180-day extension periods, a total of 6 subjects withdrew from treatment for the following adverse reactions, reported by 1 subject each: nasal discomfort, headache dysgeusia, PSA increased, allergic reaction (hives, swollen lips and tongue), and 1 patient with myalgia, arthralgia, fever, chills and petechiae.
Increased Hematocrit
- Among all subjects (n=306) who received testosterone at any dose in the 90-day clinical study and its 90- and 180-day extension periods, a total of 4 subjects had a hematocrit level > 55%. These 4 patients had baseline hematocrits of 48% and 51%. In no case did hematocrit exceed 58%.
Nasal Adverse Reactions
- Among all subjects (n=306) who received testosterone at any dose in the 90-day clinical study and its 90- and 180-day extension periods, the following nasal adverse reactions were reported: nasopharyngitis (8.2%), rhinorrhea (7.8%), epistaxis (6.5%), nasal discomfort (5.9%), parosmia (5.2%), nasal scab (5.2%), upper respiratory infection (4.2%), nasal dryness (4.2%), and nasal congestion (3.9%).
Postmarketing Experience
- The following adverse reactions have been identified during post-approval use of testosterone. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Vascular Disorders: Venous thromboembolism.
Drug Interactions
Insulin
- Changes in insulin sensitivity or glycemic control may occur in patients treated with androgens. In diabetic patients, the metabolic effects of androgens may decrease blood glucose and, therefore, may necessitate a decrease in the dose of anti-diabetic medication.
Oral Anticoagulants
- Changes in anticoagulant activity may be seen with androgens, therefore more frequent monitoring of international normalized ration (INR) and prothrombin time is recommended in patients taking warfarin, especially at the initiation and termination of androgen therapy.
Corticosteroids
- The concurrent use of testosterone with corticosteroids may result in increased fluid retention and requires monitoring particularly in patients with cardiac, renal, or hepatic disease.
Oxymetazoline
- A 2.6% decrease in mean AUC(0-24) and 3.6% decrease in mean Cmax of total testosterone was observed in males with symptomatic seasonal rhinitis when treated with oxymetazoline 30 minutes prior to testosterone compared to when left untreated. Oxymetazoline does not impact the absorption of testosterone when concomitantly administered with testosterone. Drug interaction potential with other nasally administered drugs other than oxymetazoline has not been studied.
Use in Specific Populations
Pregnancy
- Testosterone is contraindicated during pregnancy or in women who may become pregnant. Testosterone is teratogenic and may cause fetal harm. Exposure of a fetus to androgens may result in varying degrees of virilization. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Testosterone (nasal) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Testosterone (nasal) during labor and delivery.
Nursing Mothers
- Although it is not known how much testosterone transfers into human milk, testosterone is contraindicated in nursing women because of the potential for serious adverse reactions in nursing infants.
Pediatric Use
- Safety and efficacy of testosterone has not been established in pediatric patients less than 18 years of age. Improper use may result in acceleration of bone age and premature closure of epiphyses.
Geriatic Use
- There have not been sufficient numbers of geriatric patients involved in controlled clinical studies utilizing testosterone to determine whether efficacy in those over 65 years of age differs from younger subjects.
- Of the 306 patients enrolled in the Phase 3 clinical trial utilizing testosterone, 60 were 65 years of age or older, and 9 were 75 years of age or older. There are insufficient long-term safety data in geriatric patients to assess the potential for increased risks of cardiovascular disease and prostate cancer.
- Geriatric patients treated with androgens may also be at risk for worsening of signs and symptoms of BPH.
Gender
There is no FDA guidance on the use of Testosterone (nasal) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Testosterone (nasal) with respect to specific racial populations.
Renal Impairment
- No studies were conducted in patients with renal impairment.
Hepatic Impairment
- No studies were conducted in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Testosterone (nasal) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Testosterone (nasal) in patients who are immunocompromised.
Allergic Rhinitis
Serum total testosterone concentrations were decreased by 21 to 24% in males with symptomatic allergic rhinitis, whether treated with nasal decongestants such as oxymetazoline, or left untreated
Administration and Monitoring
Administration
- Nasal.
Monitoring
- Monitor patients with benign prostatic hyperplasia (BPH) for worsening of signs and symptoms of BPH.
- Monitor prostate-specific antigen (PSA), hematocrit and lipid concentrations periodically.
- More frequent monitoring of International Normalized Ratio (INR) and prothrombin time is recommended in patients taking warfarin.
- Regular monitoring of serum calcium concentrations is recommended in cancer patients.
IV Compatibility
- There is limited information regarding IV Compatibility.
Overdosage
- No cases of overdose with testosterone have been reported in clinical trials. There is 1 report of acute overdosage by injection of testosterone enanthate: testosterone concentrations of up to 11,400 ng/dL were implicated in a cerebrovascular accident.
- Treatment of overdosage would consist of discontinuation of testosterone together with appropriate symptomatic and supportive care.
Pharmacology
Mechanism of Action
- Endogenous androgens, including testosterone and dihydrotestosterone (DHT), are responsible for the normal growth and development of the male sex organs and for maintenance of secondary sex characteristics. These effects include the growth and maturation of the prostate, seminal vesicles, penis, and scrotum; the development of male hair distribution, such as facial, pubic, chest, and axillary hair; laryngeal enlargement, vocal cord thickening, alterations in body musculature, and fat distribution. Testosterone and DHT are necessary for the normal development of secondary sex characteristics.
- Male hypogonadism, a clinical syndrome resulting from insufficient secretion of testosterone, has two main etiologies. Primary hypogonadism is caused by defects of the gonads, such as Klinefelter’s syndrome or Leydig cell aplasia, whereas secondary hypogonadism is the failure of the hypothalamus (or pituitary) to produce sufficient gonadotropins (FSH, LH).
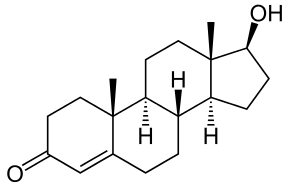
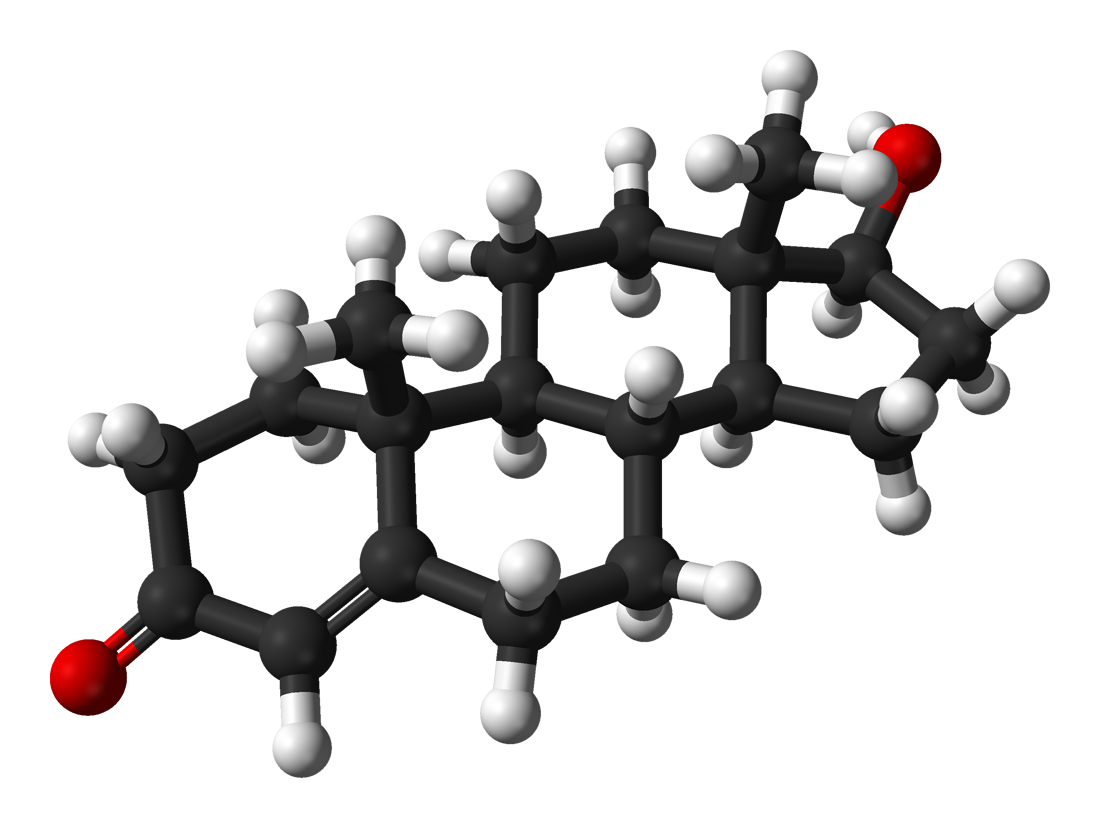
Structure
- Testosterone nasal gel is a slightly yellow gel containing 5.5 mg of testosterone in 122.5 mg of Natesto gel for nasal administration. The active pharmacologic ingredient in Natesto is testosterone, an androgen. Testosterone is a white to practically white crystalline powder chemically described as 17β-Hydroxyandrost-4-en-3-one. The structural formula is:

- The inactive ingredients are castor oil, oleoyl polyoxylglycerides, and colloidal silicon dioxide.
Pharmacodynamics
- No specific pharmacodynamic studies were conducted using testosterone.
Pharmacokinetics
- Absorption
- testosterone nasal delivers physiologic amounts of testosterone, producing circulating concentrations that approximate normal testosterone concentrations (i.e., 300 to 1,050 ng/dL) seen in healthy men. The maximum concentration for testosterone is achieved within approximately 40 minutes of administration and has a half-life ranging from 10 to 100 minutes.
- Figure 1 summarizes the pharmacokinetic profiles of total testosterone in patients completing 90 days of testosterone (nasal) treatment administered as 33 mg of testosterone daily (11 mg three times daily).
Figure 1: Mean Serum Total Testosterone Concentrations on Day 90 Following Natesto Administered As 11 mg of Testosterone Three Times Daily (N=69)

- The average daily testosterone concentration produced by testosterone (nasal) administered as 11 mg of testosterone three times daily on Day 90 was 421 (± 116) ng/dL.
- Distribution
- Circulating testosterone is primarily bound in the serum to sex hormone-binding globulin (SHBG) and albumin. Approximately 40% of testosterone in plasma is bound to SHBG, 2% remains unbound (free), and the rest is loosely bound to albumin and other proteins.
- Metabolism
- Testosterone is metabolized to various 17-keto steroids through 2 different pathways. The major active metabolites of testosterone are estradiol and dihydrotestosterone (DHT).
- DHT concentrations increased in parallel with testosterone concentrations during testosterone (nasal) treatment. After 90 days of treatment, the mean DHT/testosterone ratio was 0.09 which was within the normal range.
- Excretion
- About 90% of a dose of testosterone given intramuscularly is excreted in the urine as glucuronic and sulfuric acid conjugates of testosterone and its metabolites; about 6% of a dose is excreted in the feces, mostly in the unconjugated form. Inactivation of testosterone occurs primarily in the liver.
- Drug Interactions
- Use in patients with allergic rhinitis and oxymetazoline: The effects of allergic rhinitis and the use of oxymetazoline on the absorption of testosterone were investigated in a 3-way cross-over clinical study. Eighteen males with seasonal allergic rhinitis received 3 doses of 11 mg of testosterone intranasally (testosterone dose of 33 mg/day) while they were in the asymptomatic, symptomatic, and symptomatic but treated (with oxymetazoline) states using an environmental challenge chamber model.
- Serum total testosterone concentrations were decreased by 21 to 24% in males with symptomatic allergic rhinitis. A 2.6% decrease in mean AUC(0-24) and 3.6% decrease in mean Cmax of total testosterone was observed in males with symptomatic seasonal rhinitis when treated with oxymetazoline 30 minutes prior to testosterone (nasal) compared to when left untreated. Oxymetazoline does not impact the absorption of testosterone when concomitantly administered with testosterone (nasal). Drug interaction potential with nasally administered drugs other than oxymetazoline has not been studied.
Nonclinical Toxicology
Carcinogenesis and Mutagenesis and Impairment of Fertility
- Carcinogenicity
- Testosterone has been tested by subcutaneous injection and implantation in mice and rats. In mice, the implant induced cervical-uterine tumors, which metastasized in some cases. There is suggestive evidence that injection of testosterone into some strains of female mice increases their susceptibility to hepatoma. Testosterone is also known to increase the number of tumors and decrease the degree of differentiation of chemically induced carcinomas of the liver in rats.
- Mutagenesis
- Testosterone was negative in the in vitro Ames and in the in vivo mouse micronucleus assays.
- Impairment of Fertility
- The administration of exogenous testosterone has been reported to suppress spermatogenesis in the rat, dog and non-human primates, which was reversible on cessation of the treatment.
Clinical Studies
Testosterone Replacement Therapy
- Testosterone (nasal) was evaluated for efficacy in a 90-day, open-label, multicenter study of 306 hypogonadal men. Eligible patients were 18 years of age and older (mean age 54 years) and had morning serum total testosterone concentrations less than 300 ng/dL. Patients were Caucasian (89%), African-American (6%), Asian (5%), or of other ethnicities (less than 1%).
- Patients were instructed to self-administer testosterone (nasal) (11 mg of testosterone) intranasally either two or three times daily.
- The primary endpoint was the percentage of patients with an average serum total testosterone concentration (Cavg) within the normal range (300 to 1050 ng/dL) on Day 90.
- The secondary endpoint was the percentage of patients with a maximum total testosterone concentration (Cmax) above three predetermined limits: greater than 1500 ng/dL, between 1800 and 2500 ng/dL, and greater than 2500 ng/dL.
- A total of 78 hypogonadal men received testosterone (nasal) (11 mg of testosterone) three times daily (33 mg of testosterone daily). Of these, a total of 73 hypogonadal men were included in the statistical evaluation of efficacy (total testosterone pharmacokinetics) on Day 90 based on the intent-to-treat (ITT) population with last observation carried forward (LOCF). Ninety percent (90%) of these 73 patients had a Cavg within the normal range (300 to 1050 ng/dL) on Day 90. The percentages of patients with Cavg below the normal range (less than 300 ng/dL) and above the normal range (greater than 1050 ng/dL) on Day 90 were 10% and 0%, respectively.
- Table 3 summarizes the mean (SD) serum total testosterone concentrations on Day 90 in 69 patients who had a full pharmacokinetic sampling profile and were treated with testosterone (nasal) (11 mg of testosterone) three times daily for 90 days.

How Supplied
- Natesto (testosterone) nasal gel is available as a metered dose pump containing 11 grams of gel dispensed as 60 metered pump actuations. One pump actuation delivers 5.5 mg of testosterone in 0.122 grams of gel.
- NDC 63481-239-01
Storage
- Keep Natesto out of reach of children.
- Store at 20°C to 25°C (68°F to 77°F). Excursions are permitted to 15°C to 30°C (59°F to 86°F). See USP Controlled Room Temperature.
Handling and Disposal
- Used Natesto dispensers should be discarded in household trash in a manner that prevents accidental exposure of children or pets.
Images
Drug Images
{{#ask: Page Name::Testosterone (nasal) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel



{{#ask: Label Page::Testosterone (nasal) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling (Patient Information).
Use in Men With Known or Suspected Prostate or Breast Cancer
- Men with known or suspected prostate or breast cancer should not use Natesto.
Nasal Adverse Reactions
- Nasal adverse reactions, including nasopharyngitis, rhinorrhea, epistaxis, nasal discomfort and nasal scabbing, were reported in clinical trials of Natesto. Advise patients to report any nasal symptoms or signs to their health care professional.
Potential Adverse Reactions With Androgens
- Patients should be informed that treatment with androgens may lead to adverse reactions which include:
- Changes in urinary habits such as increased urination at night, trouble starting your urine stream, passing urine many times during the day, having an urge that you have to go to the bathroom right away, having urine accident, being unable to pass urine, and having a weak urine flow.
- Breathing disturbances, including those associated with sleep, or excessive daytime sleepiness.
- Too frequent or persistent erections of the penis.
- Nausea, vomiting, changes in skin color, or ankle swelling.
Patients Should be Advised of the Following Instructions For Use
- Read the Patient Information accompanying each Natesto metered dose pump.
- Prime the pump by depressing it 10 times prior to its first use. No priming is needed with subsequent uses of that pump.
- Administer Natesto intranasally and NOT to other parts of the body. Administer Natesto intranasally three times daily, once in the morning, once in the afternoon and once in the evening (6 to 8 hours apart), preferably at the same time each day.
- Keep Natesto out of the reach of children.
- Report any changes in their state of health, such as changes in urinary habits, breathing, sleep, mood, nasal irritation or rhinitis.
- Never share Natesto with anyone.


Precautions with Alcohol
- Alcohol-Testosterone (nasal) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- NATESTO®[1]
Look-Alike Drug Names
- Testoderm - Testoderm TTS[2]
- Testoderm - Testoderm with Adhesive[2]
- Testoderm with Adhesive - Testoderm TTS[2]
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "NATESTO- testosterone gel".
- ↑ 2.0 2.1 2.2 "https://www.ismp.org". External link in
|title=(help)