Statin therapy for ASCVD prevention
Template:Hypercholesterolemia Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Major Recommendations for Statin Therapy for ASCVD Prevention
2016 USPSTF Recommendations
Clinical practice guidelines [1] and systematic review [2] by the United States Preventive Services Task Force in 2016 stated:
- Grade B: The USPSTF recommends low-moderate intensity statin for adults without a history of cardiovascular disease (CVD) for the prevention of CVD events and mortality when all criteria are met:
- Age 40 to 75 years
- 1 or more cardiovascular disease risk factors (i.e., dyslipidemia, diabetes, hypertension, or smoking)
- Calculated 10-year cardiovascular risk of 10% or greater.
- Grade C: The USPSTF gives clinicians the option to offer a low- to moderate-dose statin to certain adults aged 40 to 75 years with no history of CVD, 1 or more CVD risk factors, and a calculated 10-year CVD event risk of 7.5% to 10%.
- Grade I: The USPSTF does not recommend statin therapy for primary prevention of CVD events and mortality in adults 76 years old due to insufficient evidence to assess benefits vs. risks.
The projected benefits of statin therapy include decreased incidences of the following[2]:
- All-cause mortality (NNT 250)
- Cardiovascular mortality (NNT 233)
- Composite cardiovascular outcomes (NNT 72)
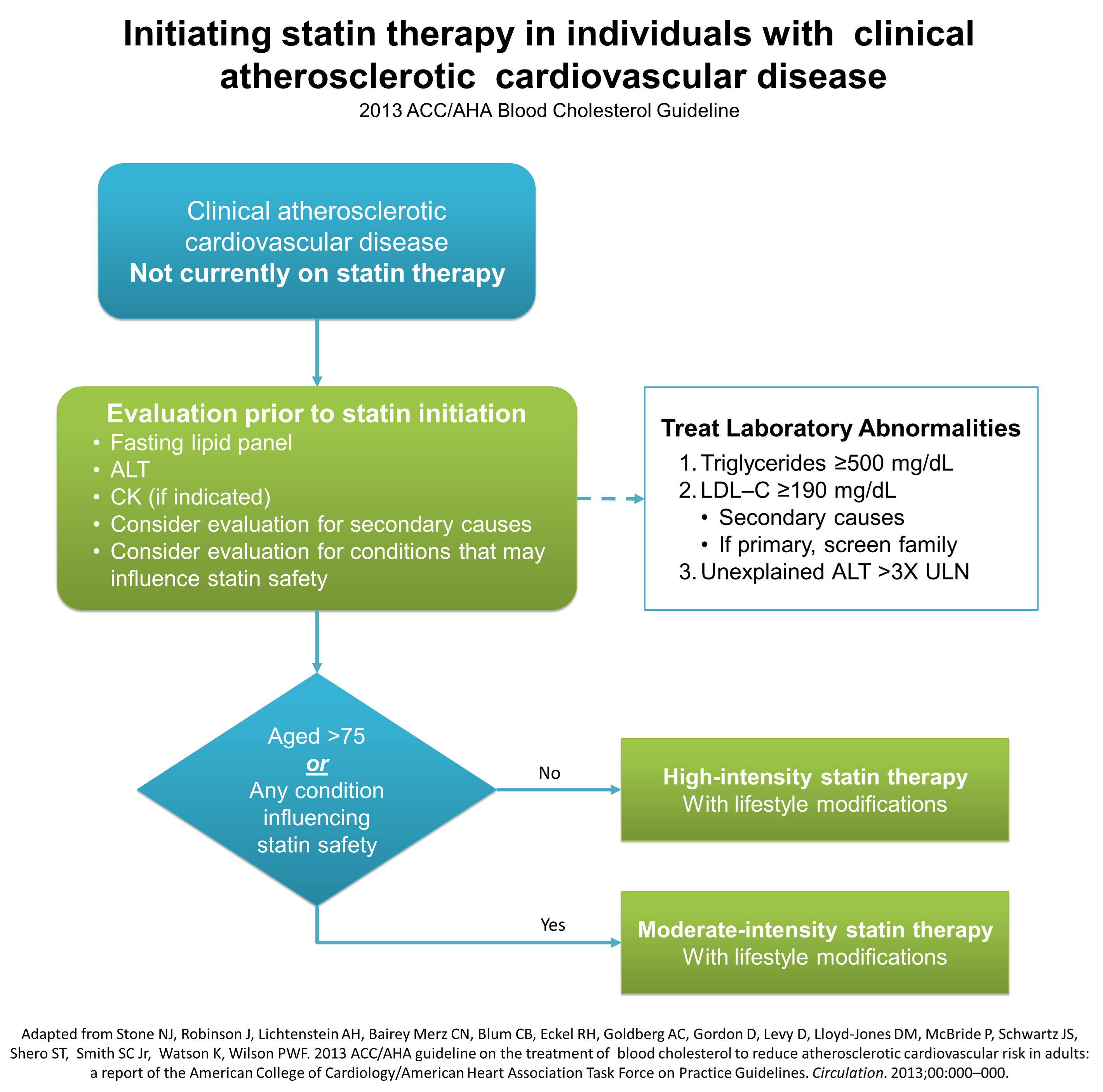
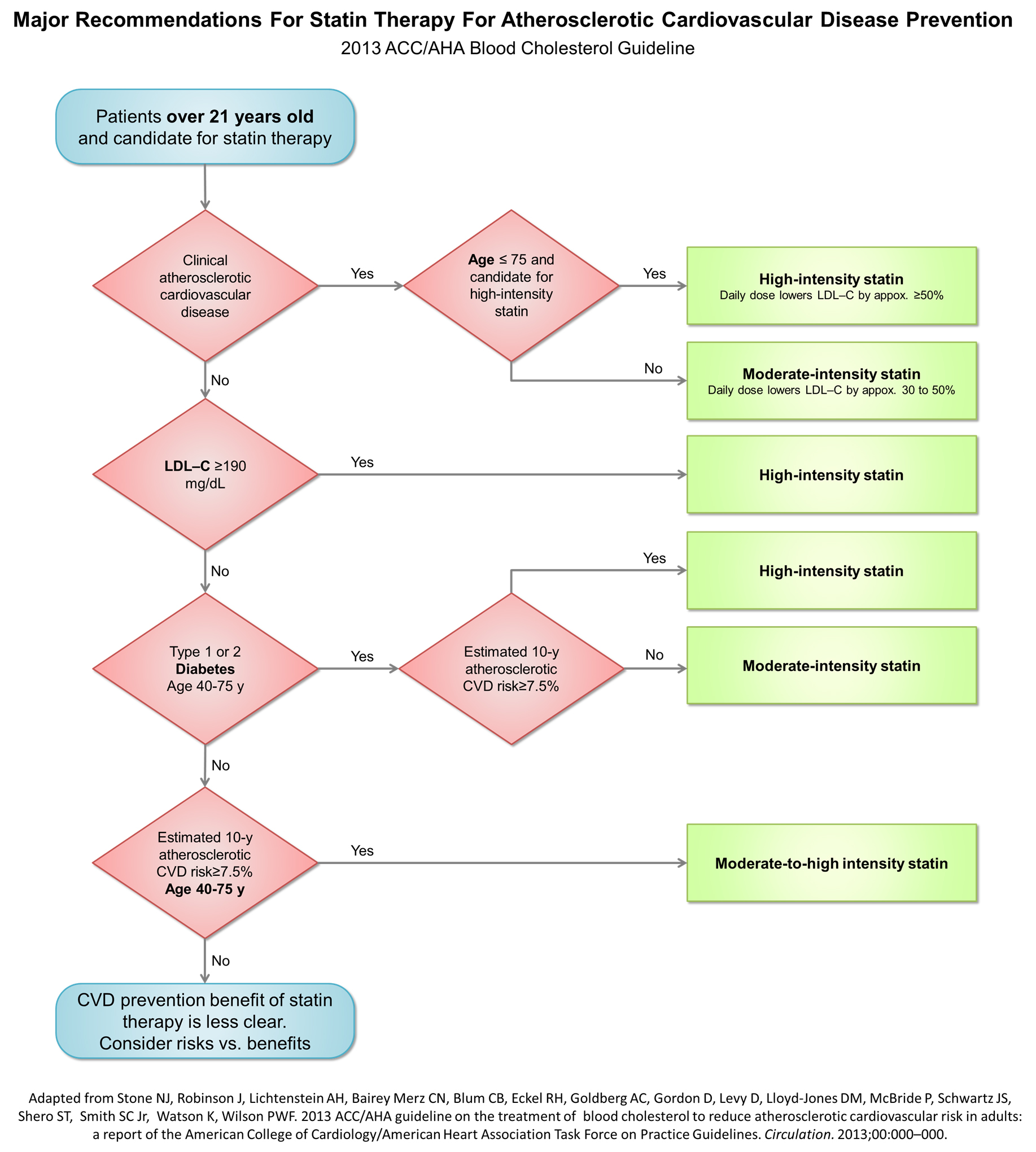
2013 AHA/ACC Guidelines
The following is a treatment algorithm proposed by the AHA/ACC guidelines committee:[3][4]
Initial evaluation prior to statin initiation
Initial evaluation prior to statin initiation include:
- Fasting lipid panel
- Fasting lipid panel preferred. In a nonfasting individual, a non–HDL-C level ≥220 mg/dL could indicate genetic hypercholesterolemia that requires further evaluation or a secondary etiology. If nonfasting triglycerides are ≥500 mg/dL, a fasting lipid panel is required.
- ALT
- CK
- Consider evaluation for other secondary causes
| Secondary Cause | Elevated LDL-C | Elevated Triglycerides |
|---|---|---|
| Diet | Saturated or trans fats
Weight gain Anorexia nervosa |
Weight gain
Very-low-fat diets High intake of refined carbohydrates Excessive alcohol intake |
| Drugs | Diuretics
Cyclosporine Glucocorticoids Amiodarone |
Oral estrogens
Glucocorticoids Bile acid sequestrants Protease inhibitors Retinoic acid Anabolic steroids Sirolimus Raloxifene Tamoxifen Beta blockers |
| Diseases | Biliary obstruction
Nephrotic syndrome |
Nephrotic syndrome
Chronic renal failure Lipodystrophies |
| Disorders and altered states of metabolism | Hypothyroidism
Obesity Pregnancy |
Diabetes (poorly controlled)
Hypothyroidism Obesity Pregnancy |
- ↑ US Preventive Services Task Force. Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW; et al. (2016). "Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement". JAMA. 316 (19): 1997–2007. doi:10.1001/jama.2016.15450. PMID 27838723. Review in: Ann Intern Med. 2017 Mar 21;166(6):JC26
- ↑ 2.0 2.1 Chou R, Dana T, Blazina I, Daeges M, Bougatsos C, Grusing S; et al. (2016). "Statin Use for the Prevention of Cardiovascular Disease in Adults: A Systematic Review for the U.S. Preventive Services Task Force". U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. 139. PMID 27905702.
- ↑ 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. http://ac.els-cdn.com/S0735109713060282/1-s2.0-S0735109713060282-main.pdf?_tid=06f509a0-9c67-11e6-b670-00000aab0f01&acdnat=1477587879_04fcb2e98e9d9b3a556253eefd0247d2 Accessed on October 27, 2016
- ↑ Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH; et al. (2014). "2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. 129 (25 Suppl 2): S1–S45. doi:10.1161/01.cir.0000437738.63853.7a. PMID 24222016.