Obstructive lung disease
|
Obstructive lung disease Microchapters |
|
Differentiating Obstructive Lung Disease from other Diseases |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [2], Feham Tariq, MD [3], Dildar Hussain, MBBS [4]
Overview
An obstructive lung disease is a group of diseases characterized by various deformities that result in the collapse of airways. Patients suffering from obstructive lung disease usually present with shortness of breath due to damage to the airways within the lungs. This results in an inability to exhale air completely and an abnormally high amount of air may still present in the lungs after the end of full expiration. One of the main etiology of the obstructive lung disease is long-term exposure to substances that irritate and damage the lung epithelium and lung parenchyma. This includes cigarette smoke, air pollution, chemical fumes, or dust etc. Patients are usually asymptotic during the initial phase of the disease. However, symptoms usually become more evident as the disease process gets worse. The symptoms usually include a productive cough, difficulty in breathing, wheezing, and tightness in the chest. These diseases include asthma, COPD, bronchiolitis, bronchiectasis, heart failure, tuberculosis, cystic fibrosis, and lymphangioleiomyomatosis. Obstructive lung diseases present with an obstructive pattern that is an increase in total lung capacity (TLC), increase in respiratory volume (RV), a decrease in forced vital capacity (FVC), a decreased forced expiratory volume (FEV1), and a decreased FEV1/FVC, on pulmonary function tests.
Classification
Various diseases that present with an obstructive pattern on pulmonary function tests include:
- Asthma
- COPD
- Bronchiolitis
- Bronchiectasis
- Heart failure
- Tuberculosis
- Lymphangioleiomyomatosis
- Cystic fibrosis
Spirometry Findings in Various Lung Conditions
Spirometry can help distinguish obstructive lung disease from restrictive lung disease. On spirometry the findings include:[1][2]
| Pulmonary Function Test | Obstructive Lung Disease | Restrictive Lung Disease | 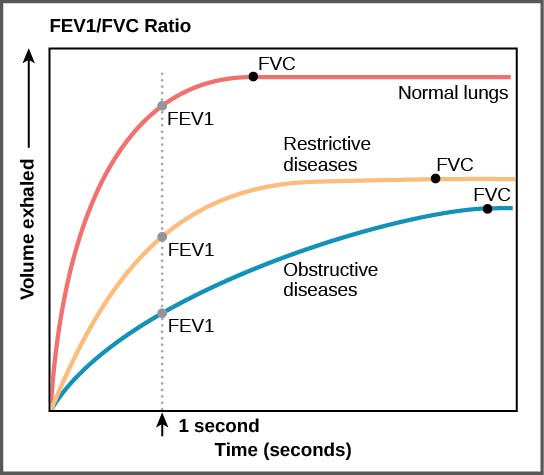 |
|---|---|---|---|
| Total lung capacity (TLC) | ↑ | ↓ | |
| Residual volume (RV) | ↑ | ↓ | |
| Forced vital capacity (FVC) | ↓ | ↓ | |
| Forced expiratory volume
in 1st second (FEV1) |
↓↓ | ↓ | |
| FEV1/FVC ratio | ↓ | N to ↑ | |
| Maximum voluntary ventilation | ↓ | ↓ | |
| RV/TLC | ↑ | Normal |
Approach to Lung Disorders
| Spirometry | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Low FEV1/FVC ratio | Normal to high FEV1/FVC ratio | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Obstructive Lung Disease | Restrictive Lung Disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Bronchodilator therapy | DLCO | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Increased FEV1 | No change in FEV1 | Normal DLCO | Decreased DLCO | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Asthma | COPD | Chest wall disorders | Interstitial Lung Disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Differentiating Obstructive Lung Disease from other Diseases
Various diseases presenting with obstructive pattern on pulmonary function tests can be differentiated from each other as follows:
| Diseases | Clinical manifestations | Diagnosis | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Signs | Lab findings | PFT | Imaging | Gold standard | Other features | ||||||||||||||
| Cough | Dyspnea | Hemoptysis | Fever | Weight loss | Cyanosis | Clubbing | JVD | Peripheral edema | Auscultation | ABGs | FEV1/FVC | TLC | DLCO | |||||||
| CXR | CT scan | Other tests | ||||||||||||||||||
| Asthma[3] | + | + | ± | ± | − | − | − | − | − |
|
|
|
FEV1:FVC =<0.7 |
|
|
|
|
|
|
Associated with:
|
| Chronic bronchitis[5] | + | + | ± | + | − | − | − | − | − |
|
|
|
|
|
|
|
|
Microbiological testing is done in cases of:
|
|
|
| Bronchiolitis[7] | + | + | − | + | − | − | − | − | – |
|
|
|
|
|
|
|
|
|
Can be associated with:
| |
| Emphysema | + | + | – | + | + | + | + | – | – |
|
|
|
|
|
– |
|
|
|
|
|
| Bronchiectasis [9] | + | + | + | + | – | + | + | – | – |
|
|
|
|
|
|
|
|
| ||
| Heart failure | + | + | – | – | – | + | – | + | + |
|
|
|
|
|
|
|
||||
| Tuberculosis | + | + | + | + | + | – | – | – | – |
|
|
|
|
|||||||
| Lymphangioleiomyomatosis | + | + | +(<5%) | - | - | - | +(rare) | - | + |
|
|
|
|
|
|
|
|
|
|
|
| Status Asthmaticus | + | + | - | ± | - | - | - | + | - |
|
|
|
|
|
|
|
- |
|
|
|
| Cystic fibrosis | + | + | + | + | - | + | + | - | - |
|
|
|
|
|
|
|||||
References
- ↑ Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CP, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J (November 2005). "Interpretative strategies for lung function tests". Eur. Respir. J. 26 (5): 948–68. doi:10.1183/09031936.05.00035205. PMID 16264058.
- ↑ Mehrparvar AH, Sakhvidi MJ, Mostaghaci M, Davari MH, Hashemi SH, Zare Z (2014). "Spirometry values for detecting a restrictive pattern in occupational health settings". Tanaffos. 13 (2): 27–34. PMC 4260070. PMID 25506373.
- ↑ Elbehairy AF, Raghavan N, Cheng S, Yang L, Webb KA, Neder JA; et al. (2015). "Physiologic characterization of the chronic bronchitis phenotype in GOLD grade IB COPD". Chest. 147 (5): 1235–1245. doi:10.1378/chest.14-1491. PMID 25393126.
- ↑ Gaeta M, Minutoli F, Girbino G, Murabito A, Benedetto C, Contiguglia R, Ruggeri P, Privitera S (2013). "Expiratory CT scan in patients with normal inspiratory CT scan: a finding of obliterative bronchiolitis and other causes of bronchiolar obstruction". Multidiscip Respir Med. 8 (1): 44. doi:10.1186/2049-6958-8-44. PMC 3710098. PMID 23835554.
- ↑ Mejza F, Gnatiuc L, Buist AS, Vollmer WM, Lamprecht B, Obaseki DO; et al. (2017). "Prevalence and burden of chronic bronchitis symptoms: results from the BOLD study". Eur Respir J. 50 (5). doi:10.1183/13993003.00621-2017. PMC 5699921. PMID 29167298.
- ↑ Park JE, Kim Y, Lee SW, Shim SS, Lee JK, Lee JH (2016). "The usefulness of low-dose CT scan in elderly patients with suspected acute lower respiratory infection in the emergency room". Br J Radiol. 89 (1060): 20150654. doi:10.1259/bjr.20150654. PMC 4846199. PMID 26861744.
- ↑ Allinson JP, Hardy R, Donaldson GC, Shaheen SO, Kuh D, Wedzicha JA (2016). "The Presence of Chronic Mucus Hypersecretion across Adult Life in Relation to Chronic Obstructive Pulmonary Disease Development". Am J Respir Crit Care Med. 193 (6): 662–72. doi:10.1164/rccm.201511-2210OC. PMC 4824943. PMID 26695373.
- ↑ Kesimer M, Ford AA, Ceppe A, Radicioni G, Cao R, Davis CW; et al. (2017). "Airway Mucin Concentration as a Marker of Chronic Bronchitis". N Engl J Med. 377 (10): 911–922. doi:10.1056/NEJMoa1701632. PMC 5706541. PMID 28877023.
- ↑ Dijkstra AE, de Jong K, Boezen HM, Kromhout H, Vermeulen R, Groen HJ; et al. (2014). "Risk factors for chronic mucus hypersecretion in individuals with and without COPD: influence of smoking and job exposure on CMH". Occup Environ Med. 71 (5): 346–52. doi:10.1136/oemed-2013-101654. PMID 24642640.
- ↑ Espiritu JD, Ruppel G, Shrestha Y, Kleinhenz ME (June 2003). "The diffusing capacity in adult cystic fibrosis". Respir Med. 97 (6): 606–11. PMID 12814143.