Hyaluronidase
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alberto Plate [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Hyaluronidase is a dermatological agent, enzyme and tissue permeability modifier that is FDA approved for the treatment of subcutaneous fluid administration, dispersion and absorption of injected drugs, subcutaneous urography. Common adverse reactions include injection site reaction.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Subcutaneous Fluid Administration (Hypodermoclysis)
- Insert needle with aseptic precautions. With tip lying free and movable between skin and muscle, begin clysis; fluid should start in readily without pain or lump. Then inject Hyaluronidase (hyaluronidase injection) into rubber tubing close to needle. An alternate method is to inject Hyaluronidase under skin prior to clysis. 150 U will facilitate absorption of 1,000 mL or more of solution. As with all parenteral fluid therapy, observe effect closely, with same precautions for restoring fluid andelectrolyte balance as in intravenous injections. The dose, the rate of injection, and the type of solution (saline, glucose, Ringer’s, etc.) must be adjusted carefully to the individual patient. When solutions devoid of inorganic electrolytes are given by hypodermoclysis, hypovolemia may occur. This may be prevented by using solutions containing adequate amounts of inorganic electrolytes and/or controlling the volume and speed of administration.
- Hyaluronidase may be added to small volumes of solution (up to 200 mL), such as small clysis for infants or solutions of drugs for subcutaneous injection. For infants and children less than 3 years old, the volume of a single clysis should be limited to 200 mL; and in premature infants or during the neonatal period, the daily dosage should not exceed 25 mL/kg of body weight; the rate of administration should not be greater than 2 mL per minute. For older patients, the rate and volume of administration should not exceed those employed for intravenous infusion.
Absorption and Dispersion of Injected Drugs
- Absorption and dispersion of other injected drugs may be enhanced by adding 50-300 Units, most typically 150 U hyaluronidase, to the injection solution.
Subcutaneous Urography
- The subcutaneous route of administration of urographic contrast media is indicated when intravenous administration cannot be successfully accomplished, particularly in infants and small children. With the patient prone, 75 U of Hyaluronidase (hyaluronidase injection) is injected subcutaneously over each scapula, followed by injection of the contrast medium at the same sites.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Hyaluronidase in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Hyaluronidase in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Hyaluronidase FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Hyaluronidase in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Hyaluronidase in pediatric patients.
Contraindications
- Hypersensitivity to hyaluronidase or any other ingredient in the formulation is a contraindication to the use of this product. A preliminary skin test for hypersensitivity to Hyaluronidase can be performed. The skin test is made by an intradermal injection of approximately 0.02 mL (3 Units) of a 150 Unit/mL solution. A positive reaction consists of a wheal with pseudopods appearing within 5 minutes and persisting for 20 to 30 minutes and accompanied by localized itching. Transient vasodilation at the site of the test, i.e., erythema, is not a positive reaction. Discontinue Hyaluronidase if sensitization occurs.
Warnings
Spread of Localized Infection
- Hyaluronidase should not be injected into or around an infected or acutely inflamed area because of the danger of spreading a localized infection. Hyaluronidase should not be used to reduce the swelling of bites or stings.
Ocular Damage
- Hyaluronidase should not be applied directly to the cornea.
Enzyme Inactivation with Intravenous Administration
- Hyaluronidase should not be used for intravenous injections because the enzyme is rapidly inactivated.
Adverse Reactions
Clinical Trials Experience
- The following adverse reactions have been identified during post-approval use of hyaluronidase products. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The most frequently reported adverse reactions have been local injection site reactions.
- Hyaluronidase has been reported to enhance the adverse reactions associated with co-administered drug products. Edema has been reported most frequently in association with hypodermoclysis.
Allergic reactions (urticaria, angioedema) have been reported in less than 0.1% of patients receiving hyaluronidase. Anaphylactic-like reactions following retrobulbar block or intravenous injections have occurred, rarely.
Postmarketing Experience
There is limited information regarding Hyaluronidase Postmarketing Experience in the drug label.
Drug Interactions
It is recommended that appropriate references be consulted regarding physical or chemical incompatibilities before adding Hyaluronidase to a solution containing another drug.
Incompatibilities
- Furosemide, the benzodiazepines and phenytoin have been found to be incompatible with hyaluronidase.
Drug-Specific Precautions
- Hyaluronidase should not be used to enhance the dispersion and absorption of dopamine and/or alpha agonist drugs. When considering the administration of any other drug with hyaluronidase, it is recommended that appropriate references first be consulted to determine the usual precautions for the use of the other drug; e.g., when epinephrine is injected along with hyaluronidase, the precautions for the use of epinephrine in cardiovascular disease, thyroid disease, diabetes, digital nerve block, ischemia of the fingers and toes etc., should be observed.
Local Anesthetics
- When hyaluronidase is added to a local anesthetic agent, it hastens the onset of analgesia and tends to reduce the swelling caused by local infiltration, but the wider spread of the local anesthetic solution increases its absorption; this shortens its duration of action and tends to increase the incidence of systemic reaction.
Salicylates, Cortisone, ACTH, Estrogens and Antihistamines
- Patients receiving large doses of salicylates, cortisone, ACTH, estrogens or antihistamines may require larger amounts of hyaluronidase for equivalent dispersing effect, since these drugs apparently render tissues partly resistant to the action of hyaluronidase.
Use in Specific Populations
Pregnancy
- No adequate and well controlled studies have been conducted with Hyaluronidase in pregnant women. No adequate and well controlled animal studies have been conducted with Hyaluronidase to determine reproductive effects. Hyaluronidase should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Hyaluronidase in women who are pregnant.
Labor and Delivery
- Administration of hyaluronidase during labor was reported to cause no complications: no increase in blood loss or differences in cervical trauma were observed.
Nursing Mothers
- It is not known whether hyaluronidase is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when hyaluronidase is administered to a nursing woman.
Pediatric Use
- The safety and effectiveness of Hyaluronidase have been established in pediatric patients. Use of Hyaluronidase in these patients is supported by evidence from adequate and well-controlled studies. Clinical hydration requirements for children can be achieved through administration of subcutaneous fluids facilitated with Hyaluronidase The dosage of subcutaneous fluids administered is dependent upon the age, weight, and clinical condition of the patient as well as laboratory determinations. The potential for chemical or physical incompatibilities should be kept in mind
- The rate and volume of subcutaneous fluid administration should not exceed those employed for intravenous infusion. For premature infants or during the neonatal period, the daily dosage should not exceed 25 mL/kg of body weight, and the rate of administration should not be greater than 2 mL per minute. During subcutaneous fluid administration, special care must be taken in pediatric patients to avoid over hydration by controlling the rate and total volume of the infusion
Geriatic Use
- No overall differences in safety or effectiveness have been observed between elderly and younger adult patients.
Gender
There is no FDA guidance on the use of Hyaluronidase with respect to specific gender populations.
Race
There is no FDA guidance on the use of Hyaluronidase with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Hyaluronidase in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Hyaluronidase in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Hyaluronidase in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Hyaluronidase in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Hyaluronidase Administration in the drug label.
Monitoring
There is limited information regarding Hyaluronidase Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Hyaluronidase and IV administrations.
Overdosage
There is limited information regarding Hyaluronidase overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Mechanism of Action
- Hyaluronidase is a dispersion agent, which modifies the permeability of connective tissue through the hydrolysis of hyaluronic acid, a polysaccharide found in the intercellular ground substance of connective tissue, and of certain specialized tissues, such as the umbilical cord and vitreous humor. Hyaluronic acid is also present in the capsules of type A and C hemolytic streptococci. Hyaluronidase hydrolyzes hyaluronic acid by splitting the glucosaminidic bond between Cl of an N-acetylglucosamine moiety and C4 of a glucuronic acid moiety. This temporarily decreases the viscosity of the cellular cement and promotes dispersion of injected fluids or of localized transudates or exudates, thus facilitating their absorption.
- Hyaluronidase cleaves glycosidic bonds of hyaluronic acid and, to a variable degree, some other acid mucopolysaccharides of the connective tissue. The activity is measured in vitro by monitoring the decrease in the amount of an insoluble serum albumin-hyaluronic acid complex as the enzyme cleaves the hyaluronic acid component.
Structure
Pharmacodynamics
- In the absence of hyaluronidase, material injected subcutaneously disperses very slowly. Hyaluronidase facilitates dispersion, provided local interstitial pressure is adequate to furnish the necessary mechanical impulse. Such an impulse is normally initiated by injected solutions. The rate and extent of dispersion and absorption is proportionate to the amount of hyaluronidase and the volume of solution.
- Results from an experimental study, in humans, on the influence of hyaluronidase in bone repair support the conclusion that this enzyme alone, in the usual clinical dosage, does not deter bone healing.
Pharmacokinetics
- Knowledge of the mechanisms involved in the disappearance of injected hyaluronidase is limited. It is known, however, that the blood of a number of mammalian species brings about the inactivation of hyaluronidase.
Studies have demonstrated that hyaluronidase is antigenic: repeated injections of relatively large amounts of this enzyme may result in the formation of neutralizing antibodies.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Long-term animal studies have not been performed to assess the carcinogenic or mutagenic potential of hyaluronidase. Hyaluronidase is found in most tissues of the body. Long-term animal studies have not been performed to assess whether hyaluronidase impaired fertility; however, it has been reported that testicular degeneration may occur with the production of organ-specific antibodies against this enzyme following repeated injections. Human studies on the effect of intravaginal hyaluronidase in sterility due to oligospermia indicated that hyaluronidase may have aided conception. Thus, it appears that hyaluronidase may not adversely affect fertility in females.
Clinical Studies
There is limited information regarding Hyaluronidase Clinical Studies in the drug label.
How Supplied
- Sterile as 150 USP units of hyaluronidase per mL in a 2 mL single-use glass vial with a gray rubber stopper and aluminum flip-off seal.
Storage
- Store unopened in a refrigerator at 2° to 8°C (36° to 46° F).
Images
Drug Images
{{#ask: Page Name::Hyaluronidase |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
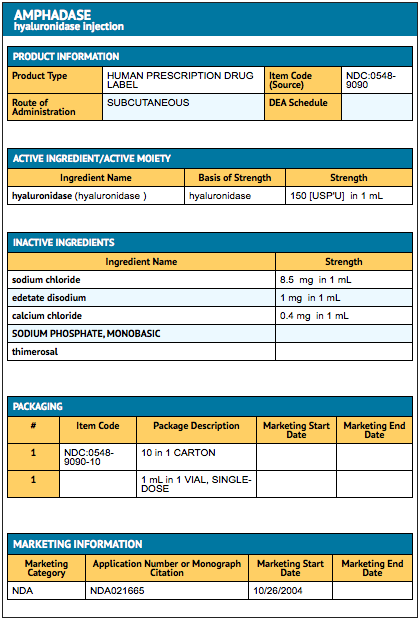
{{#ask: Label Page::Hyaluronidase |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Hyaluronidase Patient Counseling Information in the drug label.
Precautions with Alcohol
- Alcohol-Hyaluronidase interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Hyaluronidase Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Hyaluronidase |Label Name=Hyaluronidasepackage2.png
}}
{{#subobject:
|Label Page=Hyaluronidase |Label Name=Hyaluronidase package.png
}}