Glaucoma physical examination
|
Glaucoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Glaucoma physical examination On the Web |
|
American Roentgen Ray Society Images of Glaucoma physical examination |
|
Risk calculators and risk factors for Glaucoma physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Rohan Bir Singh, M.B.B.S.[2]
Overview
Ocular Examination
- External adnexae
- Useful in determining the presence of a variety of conditions associated with secondary glaucomas as well as external ocular manifestations of glaucoma therapy.
- Pupils
- Pupillary responses are one measure of compliance in patients who are on miotic therapy. Corectopia, ectropion uveae and pupillary abnormalities may be observed in some forms of glaucoma. Testing for a RAPD may detect asymmetric optic nerve damage in glaucoma.
- Conjunctiva
- conjunctival injection can lead to acutely elevated IOP during chronic use of sympathomimetic drops
- massive episcleral venous dilation can cause chronically elevated IOP
- black adrenochrome deposits due to chronic use of epinephrine derivative drops
- use of topical antiglaucoma medication may lead to decreased tear production, allergic reactions, foreshortening of the conjunctival fornices, scarring.
- to measure size, height, degree of vascularization, integrity of a filtering bleb if present
- Episclera and sclera
- dilation of the episcleral vessels can cause elevated episcleral venous pressure.
- sentinel vessels in case of an intraocular tumor
- thinning or staphylomatous areas
- Cornea
- enlargement of the cornea, breaks in Descemet’s membrane (Haab’s striae) can lead to developmental glaucoma
- punctate epithelial defects (especially in the inferonasal interpalpebral region) secondary to medication toxicity
- microcystic epithelial edema → acute elevated IOP
- endothelial abnormalities → underlying associated secondary glaucoma
- Krukenberg spindle in pigmentary glaucoma
- deposition of exfoliation material in exfoliation syndrome
- keratic precipitates in uveitic glaucoma
- guttae in Fuchs endothelial dystrophy
- irregular and vesicular lesions in posterior polymorphous dystrophy
- ‘beaten bronze’ appearance in the iridocorneal endothelial syndrome
- anteriorly displaced Schwalbe’s line → Axenfeld-Rieger syndrome
- traumatic or surgical corneal scars, corneal thickness
- Anterior chamber
- width of the chamber angle → van Herick method (A narrow slit beam is directed at an angle of 60˚ onto the cornea just anterior to the limbus. If the distance from the anterior iris surface to the posterior surface of the cornea is less than one fourth the thickness of the cornea, the angle may be narrow)
- uniformity of depth of the anterior chamber (iris bombe, iris masses)
- inflammatory cells, red cells, ghost cells, fibrin, vitreous
- Iris
- heterochromia, iris atrophy, transillumination defects, ectropion uveae, corectopia, nevi, nodules, exfoliative material
- early stages of neovascularization of the anterior segment → fine tufts around the pupillary margin, fine network of vessels on the surface of the iris.
- evidence of trauma (sphincter tear, iridodonesis), iris pigmentation \
- Lens
- exfoliative material, phacodonesis, subluxation, dislocation
- lens size, shape and clarity
- posterior subcapsular cataract → chronic corticosteroid use
- presence, type and position of an IOL
- Fundus
- careful assessment of the optic disc
- hemorrhage, effusion, masses, inflammatory lesion, retinovascular occlusion, diabetic retinopathy, retinal detachment
Gonioscopy
- Under normal conditions the anterior chamber angle cannot be vieweddirectly through the cornea, because light coming from the angle undergoes total internal reflection at the tear film-air interface.
- Because the index of refraction of glass or plastic is similar to that of thecornea and tears, gonioscopy eliminates this interface and replaces it with anew lens-air interface set at a different angle to the emerging rays.
- Types of goniolenses
- Indirect goniolens: Goldmann-type, Zeiss-type
- Direct goniolens: Koeppe, Barkan, Wurst, Richardson.
- Angle landmarks: Schwalbe’s line and scleral spur → inferior portion
- The width of the angle is determined by :
- the site of insertion of the iris on the ciliary face
- the convexity of the iris
- the prominence of the peripheral iris roll
- The best method for describing the angle is a description or drawing of theiris contour, the location of the iris insertion, and the angle between the iris and the trabecular meshwork.
- Gonioscopic grading systems
- Shaffer system→ describes the angle between the iris and the surface of the trabecular meshwork
- Grade IV 45°
- Grade III 20-45°
- Grade II 20° Angle closure possible
- Grade I 10° Angle closure probable in time
- Slit <10° Angle closure very likely
- O (the iris is against the trabecular meshwork; angle closure is present)
- Spaeth system → describes the peripheral iris contour, the insertion of their is root, and the effects of indentation gonioscopy on the angle configuration.
- Ordinarily, Schlemm’s canal is invisible by gonioscopy. Occasionally during gonioscopy in normal eyes, blood refluxes into Schlemm’s canal where it is seen as a faint red line in the posterior portion of the trabecular meshwork. Blood enters Schlemm’s canal when episcleral venous pressure exceeds IOP, most commonly because of compression of the episcleral veins by the lip of the goniolens. Pathological causes include hypotony and elevated episcleral venous pressure (e.g. carotid-cavernous fistula, Sturge-Weber syndrome).
- Normal blood vessels in the angle include:
- radial iris vessels, portions of the arterial circle of the ciliary body
- vertical branches of the anterior ciliary arteries → oriented either radially along the iris or circumferentially (in a serpentine
manner) in the ciliary body face Fuchs heterochromic iridocyclitis → fine, branching, unsheathed, meandering Neovascular glaucoma → trunklike vessels crossing the ciliary body and scleral spur and arborizing over the trabecular meshwork. • Gonioscopic examination Posterior cornea pigmentation, guttata Schwalbe’s line thickening, anterior displacement Trabecular meshwork pigmentation, PAS, inflammatory or neovascular membranes, keratic precipitates Scleral spur iris processes Ciliary body band width, regularity, cyclodialysis cleft Iris contour, rubeosis, atrophy, cysts, iridodonesis Pupil, lens exfoliation syndrome, posterior synechiae, position and regularity, sphincter rupture, ectropion uveae Zonular fibers pigmentation, rupture • Iris processes → follow the normal curve of the angle; the angle structures are visible in the open spaces between the processes
-
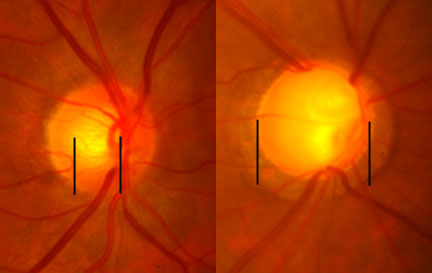
0.5 to 0.9 cup-to-disc ratio. Increase seen with open angle glaucoma.
-
Glaucoma
-
A normal range of vision. Courtesy NIH National Eye Institute
-
The same view with advanced vision loss from glaucoma.