Genital warts differential diagnosis
|
Genital warts Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Genital warts differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Genital warts differential diagnosis |
|
Risk calculators and risk factors for Genital warts differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Differentiating Genital Warts from other Diseases
It is a common misconception among men that hirsuties papillaris genitalis are genital warts. Hirsuties papillaris genitalis is not contagious and no treatment for it is necessary. Some may deem it unsightly and there are various methods of ridding the penis of the condition such as carbon dioxide laser treatment.
Genital warts (condylomata) should not be confused with Molluscum contagiosum (MC), which is often transmitted sexually, but does not occur internally as do condylomata. MC looks like small warts, which are much smaller than condylomata genital warts. It does not increase the risk of cervical cancer for women. Genital warts should not be confused with Fordyce's spots, which are considered benign.
Genital warts should be differentiated from syphilis, which commonly presents with generalized systemic symptoms such as malaise, fatigue, headache and fever. Skin eruptions may be subtle and asymptomatic. It is classically described as 1) non-pruritic bilateral symmetrical mucocutaneous rash; 2) non-tender regional lymphadenopathy; 3) condylomata lata; and 4) patchy alopecia.[1]
Anogenital wars must be differentiated from other diseases that cause anal discomfort and pain with defecation such as hemorrhoids, anal fissure and perianal abscess.
| Disease | History | Physical exam findings | Sample image |
|---|---|---|---|
| Hemorrhoids |
External hemorrhoids
Internal hemorrhoids
|
Skin examination
Digital rectal examination
|
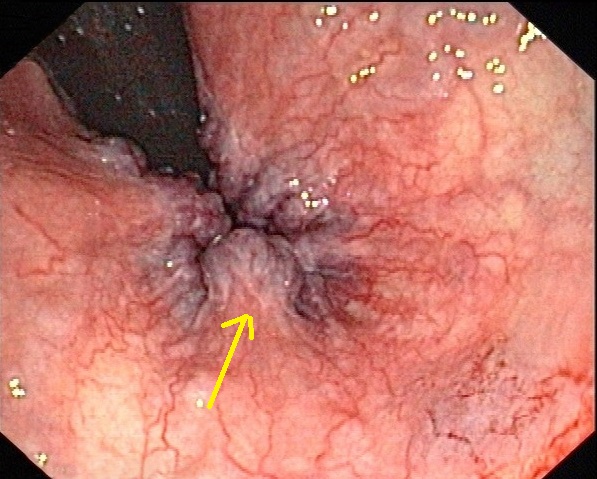 |
| Anal fissure |
|
|
 |
| Rectal prolapse |
|
|
 |
| Perianal abscess |
|
|
|
| Anal cancer |
|
 | |
| Condylomata acuminata |
|
|
References
- ↑ Moore, Zack S; Seward, Jane F; Lane, J Michael (2006). "Smallpox". The Lancet. 367 (9508): 425–435. doi:10.1016/S0140-6736(06)68143-9. ISSN 0140-6736.
- ↑ Schlichtemeier S, Engel A (2016). "Anal fissure". Aust Prescr. 39 (1): 14–7. doi:10.18773/austprescr.2016.007. PMC 4816871. PMID 27041801.
- ↑ Beaty JS, Shashidharan M (2016). "Anal Fissure". Clin Colon Rectal Surg. 29 (1): 30–7. doi:10.1055/s-0035-1570390. PMC 4755763. PMID 26929749.
- ↑ Cannon JA (2017). "Evaluation, Diagnosis, and Medical Management of Rectal Prolapse". Clin Colon Rectal Surg. 30 (1): 16–21. doi:10.1055/s-0036-1593431. PMID 28144208.
- ↑ Blaker K, Anandam JL (2017). "Functional Disorders: Rectoanal Intussusception". Clin Colon Rectal Surg. 30 (1): 5–11. doi:10.1055/s-0036-1593433. PMID 28144206.
- ↑ Sahnan K, Adegbola SO, Tozer PJ, Watfah J, Phillips RK (2017). "Perianal abscess". BMJ. 356: j475. PMID 28223268.
- ↑ Moureau-Zabotto L, Vendrely V, Abramowitz L, Borg C, Francois E, Goere D, Huguet F, Peiffert D, Siproudhis L, Ducreux M, Bouché O (2017). "Anal cancer: French Intergroup Clinical Practice Guidelines for diagnosis, treatment and follow-up". Dig Liver Dis. doi:10.1016/j.dld.2017.05.011. PMID 28610905.
- ↑ Prigge ES, von Knebel Doeberitz M, Reuschenbach M (2017). "Clinical relevance and implications of HPV-induced neoplasia in different anatomical locations". Mutat. Res. 772: 51–66. doi:10.1016/j.mrrev.2016.06.005. PMID 28528690.
- ↑ Wieland U, Kreuter A (2017). "[Genital warts in HIV-infected individuals]". Hautarzt (in German). 68 (3): 192–198. doi:10.1007/s00105-017-3938-z. PMID 28160045.
- ↑ Köhn FM, Schultheiss D, Krämer-Schultheiss K (2016). "[Dermatological diseases of the external male genitalia : Part 2: Infectious and malignant dermatological]". Urologe A (in German). 55 (7): 981–96. doi:10.1007/s00120-016-0163-9. PMID 27364818.
Template:STD/STI Template:Viral diseases Template:WH Template:WS