Gamma globulin
|
WikiDoc Resources for Gamma globulin |
|
Articles |
|---|
|
Most recent articles on Gamma globulin Most cited articles on Gamma globulin |
|
Media |
|
Powerpoint slides on Gamma globulin |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Gamma globulin at Clinical Trials.gov Trial results on Gamma globulin Clinical Trials on Gamma globulin at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Gamma globulin NICE Guidance on Gamma globulin
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Gamma globulin Discussion groups on Gamma globulin Patient Handouts on Gamma globulin Directions to Hospitals Treating Gamma globulin Risk calculators and risk factors for Gamma globulin
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Gamma globulin |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Overview
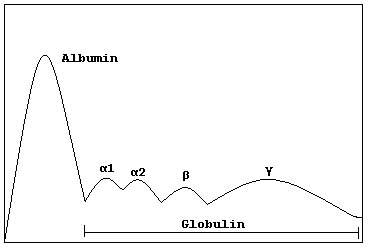
Gamma globulins, or Ig's, are a class of proteins in the blood, identified by their position after serum protein electrophoresis. The most significant gamma globulins are immunoglobulins.
Injections
Gamma globulin injections are usually given in an attempt to temporarily boost a patient's immunity against disease. Injections are most commonly used on patients who have been exposed to hepatitis A or measles, or to make a donor and a kidney recipient compatible regardless of blood type of tissue match. Injections are also used to boost immunity in patients who lack the ability to produce gamma globulins because of an immune deficiency, such as X-linked agammaglobulinemia and hyper IgM syndrome. Such injections are less common in modern medical practice than they were previously, and injections of gamma globulin previously recommended for travelers have largely been replaced by the use of hepatitis A vaccine.
Gamma globulin infusions are also used to treat immunological diseases, such as idiopathic thrombocytopenia purpura (ITP), a disease in which the platelets are being attacked by antibodies, leading to seriously low platelet counts. Gamma globulin apparently causes the spleen to ignore the antibody-tagged platelets, thus allowing them to survive and function.
Gamma globulin injections also provide substantial benefit to many suffering from Chronic Fatigue Syndrome, also known as Chronic Fatigue and Immune Disfunction Syndrome; Mylagic Encyphalitis; Chronic Epsteinn-Barr; Chronic Mono. In particular, it helps those who are greatly affected by changes in the barometric pressure (i.e., change in weather conditions, especially rain or other storms).
Another theory on how gamma globulin administration works in autoimmune disease is by overloading the mechanisms which degrade gamma globulins. Over loading the degradation mechanism causes the harmful gamma globulins to have a much shorter halflife in sera.
Pathology
An excess is known as hypergammaglobulinemia.
A disease of gamma globulins is called a "gammopathy" (for example, in monoclonal gammopathy of undetermined significance.)
Disease treatments
Kidney Transplant: Intravenous Gamma globulin was FDA approved in 2004 to reduce antibodies in a patient in kidney failure to allow that person to accept a kidney from a donor who has a different blood type, (ABO incompatible) or is an unacceptable tissue match. Dr. Stanley Jordan at Cedars-Sinai Medical Center in Los Angeles pioneered this treatment.
External links
- gamma-Globulins at the US National Library of Medicine Medical Subject Headings (MeSH)
- http://www.sciencedaily.com/releases/2004/12/041208234532.htm