Cholesterol
|
Cholesterol Microchapters |
|
Clinical Correlation |
|---|
|
Treatment |
|
Case Studies |
|
Cholesterol On the Web |
|
American Roentgen Ray Society Images of Cholesterol |
|
WikiDoc Resources for Cholesterol |
|
Articles |
|---|
|
Most recent articles on Cholesterol Most cited articles on Cholesterol |
|
Media |
|
Powerpoint slides on Cholesterol |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Cholesterol at Clinical Trials.gov Clinical Trials on Cholesterol at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Cholesterol
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Cholesterol Discussion groups on Cholesterol Patient Handouts on Cholesterol Directions to Hospitals Treating Cholesterol Risk calculators and risk factors for Cholesterol
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Cholesterol |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information on Hypercholesterolemia click here
For WikiDoc information on Hypercholesterolemia click here
For patient information on Coronary Risk Profile click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Cholesterol is a sterol (a combination steroid and alcohol). Cholesterol is a lipid found in the cell membranes of all tissues, and it is transported in the blood plasma of all animals. Because cholesterol is synthesized by all eukaryotes, trace amounts of cholesterol are also found in membranes of plants and fungi.
Background
The name cholesterol originates from the Greek chole- (bile) and stereos (solid), and the chemical suffix -ol for an alcohol, as researchers first identified cholesterol in solid form in gallstones by François Poulletier de la Salle in 1769. However, it is only in 1815 that chemist Eugène Chevreul named the compound "cholesterine".[1]
Most of the cholesterol is synthesized by the body and some has dietary origin. Cholesterol is more abundant in tissues which either synthesize more or have more abundant densely-packed membranes, for example, the liver, spinal cord and brain. It plays a central role in many biochemical processes, such as the composition of cell membranes and the synthesis of steroid hormones. Cholesterol is insoluble in blood, but is transported in the circulatory system bound to one of the varieties of lipoprotein, spherical particles which have an exterior composed mainly of water-soluble proteins. The main types, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) carry cholesterol from and to the liver.
According to the lipid hypothesis, abnormally high cholesterol levels (hypercholesterolemia) and abnormal proportions of LDL and HDL are associated with cardiovascular disease by promoting atheroma development in arteries (atherosclerosis). This disease process leads to myocardial infarction (heart attack), stroke and peripheral vascular disease. As high LDL contributes to this process, it is termed "bad cholesterol", while high levels of HDL ("good cholesterol") offer a degree of protection. The balance can be redressed with exercise, a healthy diet, and sometimes medication.
Physiology
Function
Cholesterol is required to build and maintain cell membranes; it regulates membrane fluidity over a wide range of temperatures. The hydroxyl group on cholesterol interacts with the phosphate head of the membrane, while the bulky steroid and the hydrocarbon chain is embedded in the membrane. Some research indicates that cholesterol may act as an antioxidant.[2] Cholesterol also aids in the manufacture of bile (which is stored in the gallbladder and helps digest fats), and is also important for the metabolism of fat soluble vitamins, including vitamins A, D, E and K. It is the major precursor for the synthesis of vitamin D and of the various steroid hormones (which include cortisol and aldosterone in the adrenal glands, and the sex hormones progesterone, the various estrogens, testosterone, and derivatives).
Recently, cholesterol has also been implicated in cell signalling processes, where it has been suggested that it forms lipid rafts in the plasma membrane. It also reduces the permeability of the plasma membrane to hydrogen ions (protons) and sodium ions.[3]
Cholesterol is essential for the structure and function of invaginated caveolae and clathrin-coated pits, including the caveolae-dependent endocytosis and clathrin-dependent endocytosis. The role of cholesterol in caveolae-dependent and clathrin-dependent endocytosis can be investigated by using methyl beta cyclodextrin (MβCD) to remove cholesterol from the plasma membrane.
Synthesis and intake

Cholesterol is required in the membrane of mammalian cells for normal cellular function, and is either synthesized in the endoplasmic reticulum, or derived from the diet, in which case it is delivered by the bloodstream in low-density lipoproteins. These are taken into the cell by LDL receptor-mediated endocytosis in clathrin-coated pits, and then hydrolysed in lysosomes.
Cholesterol is primarily synthesized from acetyl CoA through the HMG-CoA reductase pathway in many cells and tissues. About 20 – 25% of total daily production (~1 g/day) occurs in the liver; other sites of higher synthesis rates include the intestines, adrenal glands and reproductive organs. For a person of about 150 pounds (68 kg), typical total body content is about 35 g, typical daily internal production is about 1 g and typical daily dietary intake is 200 to 300 mg in the United States and societies adopting its dietary patterns. Of the cholesterol input to the intestines via bile production, 92-97% is reabsorbed in the intestines and recycled via enterohepatic circulation.
Konrad Bloch and Feodor Lynen shared the Nobel Prize in Physiology or Medicine in 1964 for their discoveries concerning the mechanism and regulation of the cholesterol and fatty acid metabolism.
Regulation
Biosynthesis of cholesterol is directly regulated by the cholesterol levels present, though the homeostatic mechanisms involved are only partly understood. A higher intake from food leads to a net decrease in endogenous production, while lower intake from food has the opposite effect. The main regulatory mechanism is the sensing of intracellular cholesterol in the endoplasmic reticulum by the protein SREBP (Sterol Regulatory Element Binding Protein 1 and 2). In the presence of cholesterol, SREBP is bound to two other proteins: SCAP (SREBP-cleavage activating protein) and Insig1. When cholesterol levels fall, Insig-1 dissociates from the SREBP-SCAP complex, allowing the complex to migrate to the Golgi apparatus, where SREBP is cleaved by S1P and S2P (site 1/2 protease), two enzymes that are activated by SCAP when cholesterol levels are low. The cleaved SREBP then migrates to the nucleus and acts as a transcription factor to bind to the SRE (sterol regulatory element) of a number of genes to stimulate their transcription. Among the genes transcribed are the LDL receptor and HMG-CoA reductase. The former scavenges circulating LDL from the bloodstream, whereas HMG-CoA reductase leads to an increase of endogenous production of cholesterol.[4]
A large part of this mechanism was clarified by Dr Michael S. Brown and Dr Joseph L. Goldstein in the 1970s. They received the Nobel Prize in Physiology or Medicine for their work in 1985.[4]
The average amount of blood cholesterol varies with age, typically rising gradually until one is about 60 years old. There appear to be seasonal variations in cholesterol levels in humans, more, on average, in winter.[5]
Excretion
Cholesterol is excreted from the liver in bile and reabsorbed from the intestines. Under certain circumstances, when more concentrated, as in the gallbladder, it crystallises and is the major constituent of most gallstones, although lecithin and bilirubin gallstones also occur less frequently.
Body fluids
Cholesterol is minimally soluble in water; it cannot dissolve and travel in the water-based bloodstream. Instead, it is transported in the bloodstream by lipoproteins - protein "molecular-suitcases" that are water-soluble and carry cholesterol and triglycerides internally. The apolipoproteins forming the surface of the given lipoprotein particle determine from what cells cholesterol will be removed and to where it will be supplied.
The largest lipoproteins, which primarily transport fats from the intestinal mucosa to the liver, are called chylomicrons. They carry mostly fats in the form of triglycerides and cholesterol. In the liver, chylomicron particles release triglycerides and some cholesterol. The liver converts unburned food metabolites into very low density lipoproteins (VLDL) and secretes them into plasma where they are converted to low-density lipoprotein (LDL) particles and non-esterified fatty acids, which can affect other body cells. In healthy individuals, the relatively few LDL particles are large. In contrast, large numbers of small dense LDL (sdLDL) particles are strongly associated with the presence of atheromatous disease within the arteries. For this reason, LDL is referred to as "bad cholesterol".
The 1987 report of National Cholesterol Education Program, Adult Treatment Panels suggest the total blood cholesterol level should be: <200 mg/dl normal blood cholesterol, 200-239 mg/dl borderline-high, >240 mg/dl high cholesterol.[6]
High-density lipoprotein (HDL) particles transport cholesterol back to the liver for excretion, but vary considerably in their effectiveness for doing this. Having large numbers of large HDL particles correlates with better health outcomes, and hence it is commonly called "good cholesterol". In contrast, having small amounts of large HDL particles is independently associated with atheromatous disease progression within the arteries.
Clinical significance
Hypercholesterolemia
Conditions with elevated concentrations of oxidized LDL particles, especially "small dense LDL" (sdLDL) particles, are associated with atheroma formation in the walls of arteries, a condition known as atherosclerosis, which is the principal cause of coronary heart disease and other forms of cardiovascular disease. In contrast, HDL particles (especially large HDL) have been identified as a mechanism by which cholesterol and inflammatory mediators can be removed from atheroma. Increased concentrations of HDL correlate with lower rates of atheroma progressions and even regression. The relation of cholesterol to CHD, termed the "lipid hypothesis," is still hotly debated.
Elevated levels of the lipoprotein fractions, LDL, IDL and VLDL are regarded as atherogenic (prone to cause atherosclerosis). Levels of these fractions, rather than the total cholesterol level, correlate with the extent and progress of atherosclerosis. Conversely, the total cholesterol can be within normal limits, yet be made up primarily of small LDL and small HDL particles, under which conditions atheroma growth rates would still be high. In contrast, however, if LDL particle number is low (mostly large particles) and a large percentage of the HDL particles are large, then atheroma growth rates are usually low, even negative, for any given total cholesterol concentration.
Multiple human trials utilizing HMG-CoA reductase inhibitors, known as statins, have repeatedly confirmed that changing lipoprotein transport patterns from unhealthy to healthier patterns significantly lowers cardiovascular disease event rates, even for people with cholesterol values currently considered low for adults. As a result, people with a history of cardiovascular disease may derive benefit from statins irrespective of their cholesterol levels,[7] and in men without cardiovascular disease there is benefit from lowering abnormally high cholesterol levels ("primary prevention").[8] Primary prevention in women is practiced only by extension of the findings in studies on men,[9] since in women, none of the large statin trials has shown a reduction in overall mortality or in cardiovascular end points.[10]
The American Heart Association provides a set of guidelines for total (fasting) blood cholesterol levels and risk for heart disease:[11]
| Level mg/dL | Level mmol/L | Interpretation |
| <200 | <5.2 | Desirable level corresponding to lower risk for heart disease |
| 200-239 | 5.2-6.2 | Borderline high risk |
| >240 | >6.2 | High risk |
However, as today's testing methods determine LDL ("bad") and HDL ("good") cholesterol separately, this simplistic view has become somewhat outdated. The desirable LDL level is considered to be less than 100 mg/dL (2.6 mmol/L), although a newer target of <70 mg/dL can be considered in higher risk individuals based on some of the above-mentioned trials. A ratio of total cholesterol to HDL — another useful measure — of far less than 5:1 is thought to be healthier. Of note, typical LDL values for children before fatty streaks begin to develop is 35 mg/dL.
Most testing methods for LDL do not actually measure LDL in their blood, much less particle size. For cost reasons, LDL values have long been estimated using the Friedewald formula: [total cholesterol] − [total HDL] − 20% of the triglyceride value = estimated LDL. The basis of this is that Total cholesterol is defined as the sum of HDL, LDL, and VLDL. Ordinarily just the total, HDL, and triglycerides are actually measured. The VLDL is estimated as one-fifth of the triglycerides. It is important to fast for at least 8-12 hours before the blood test because the triglyceride level varies significantly with food intake.
Given the well-recognized role of cholesterol in cardiovascular disease, it is surprising that some studies have shown an inverse correlation between cholesterol levels and mortality in subjects over 50 years of age — an 11% increase overall and 14% increase in CVD mortality per 1 mg/dL per year drop in cholesterol levels. In the Framingham Heart Study, the researchers attributed this phenomenon to the fact that people with severe chronic diseases or cancer tend to have below-normal cholesterol levels.[12] This explanation is not supported by the Vorarlberg Health Monitoring and Promotion Programme, in which men of all ages and women over 50 lower cholesterol levels with very low cholesterol were increasingly likely to die of cancer, liver diseases, and mental diseases. This result indicates that the low cholesterol effect occurs even among younger respondents, contradicting the previous assessment among cohorts of older people that this is a proxy or marker for frailty occurring with age.[13]
A small group of scientists, united in The International Network of Cholesterol Skeptics, continues to question the link between cholesterol and atherosclerosis.[14] However, the vast majority of doctors and medical scientists accepts the link as fact.[15]
Hypocholesterolemia
Abnormally low levels of cholesterol are termed hypocholesterolemia. Research into the causes of this state is relatively limited, and while some studies suggest a link with depression, cancer and cerebral hemorrhage it is unclear whether the low cholesterol levels are a cause for these conditions or an epiphenomenon.
Food sources
Cholesterol is found in animal fats: all food containing animal fats contains cholesterol; food not containing animal fats either contains no cholesterol or negligible amounts. Major dietary sources of cholesterol include eggs, beef and poultry.[16]
Plants have trace amounts of cholesterol, so even a vegan diet, which includes no animal foods, has traces of cholesterol. However, the amounts are very small. For example, to ingest the amount of cholesterol in one egg, one would need to drink about 9.6 litres (19.57 pounds) of pure peanut oil.[11] [17]
Plant products (e.g. flax seed, peanut), also contain cholesterol-like compounds, phytosterols, which are suggested to help lower serum cholesterol.[18]
Cholesteric liquid crystals
Some cholesterol derivatives, (among other simple cholesteric lipids) are known to generate the liquid crystalline cholesteric phase. The cholesteric phase is in fact a chiral nematic phase, and changes colour when its temperature changes. Therefore, cholesterol derivatives are commonly used as temperature-sensitive dyes, in liquid crystal thermometers and temperature-sensitive paints.
See also
Additional images
-
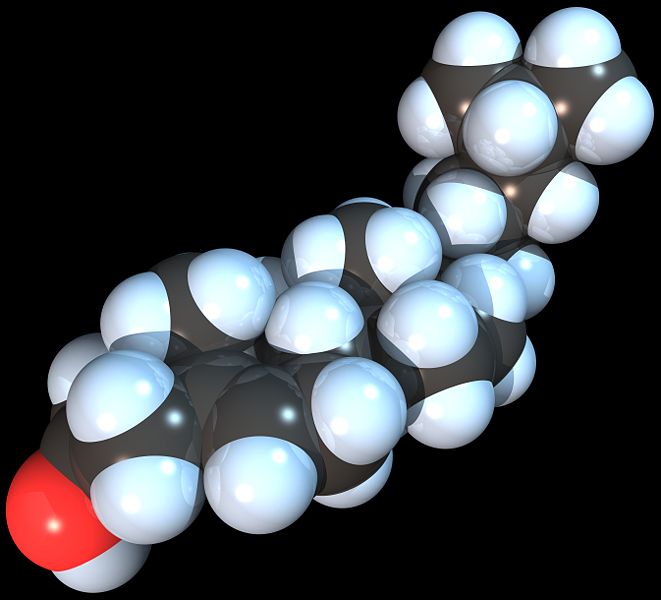
Space-filling model of the Cholesterol molecule
References
- ↑ Olson RE (1998). "Discovery of the lipoproteins, their role in fat transport and their significance as risk factors". J. Nutr. 128 (2 Suppl): 439S–443S. PMID 9478044.
- ↑ Smith LL (1991). "Another cholesterol hypothesis: cholesterol as antioxidant". Free Radic. Biol. Med. 11 (1): 47–61. PMID 1937129.
- ↑ Haines TH (2001). "Do sterols reduce proton and sodium leaks through lipid bilayers?". Prog. Lipid Res. 40 (4): 299–324. PMID 11412894.
- ↑ 4.0 4.1 Anderson RG. (2003). "Joe Goldstein and Mike Brown: from cholesterol homeostasis to new paradigms in membrane biology". Trends Cell Biol. 13: 534 &ndash, 9. PMID 14507481.
- ↑ Ockene IS, Chiriboga DE, Stanek EJ 3rd, Harmatz MG, Nicolosi R, Saperia G, Well AD, Freedson P, Merriam PA, Reed G, Ma Y, Matthews CE, Hebert JR. (2004). "Seasonal variation in serum cholesterol levels: treatment implications and possible mechanisms". Arch Intern Med. 164: 863 &ndash, 70. PMID 15111372.
- ↑ "Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. The Expert Panel". Arch. Intern. Med. 148 (1): 36–69. 1988. PMID 3422148.
- ↑ "MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial". Lancet. 360 (9326): 7–22. 2002. PMID 12114036.
- ↑ Shepherd J, Cobbe SM, Ford I; et al. (1995). "Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group". N. Engl. J. Med. 333 (20): 1301–7. PMID 7566020.
- ↑ Grundy SM (2007). "Should women be offered cholesterol lowering drugs to prevent cardiovascular disease? Yes". BMJ. 334 (7601): 982. doi:10.1136/bmj.39202.399942.AD. PMID 17494017.
- ↑ Kendrick M (2007). "Should women be offered cholesterol lowering drugs to prevent cardiovascular disease? No". BMJ. 334 (7601): 983. doi:10.1136/bmj.39202.397488.AD. PMID 17494018.
- ↑ 11.0 11.1 "About cholesterol" - American Heart Association
- ↑ Anderson KM., Castelli WP, Levy D. (1987). "Cholesterol and mortality. 30 years of follow-up from the Framingham study". JAMA. 257: 2176 &ndash, 80. PMID 3560398.
- ↑ Ulmer H., Kelleher C., Diem G., Concin H. (2004). "Why Eve is not Adam: prospective follow-up in 149650 women and men of cholesterol and other risk factors related to cardiovascular and all-cause mortality". J Womens Health (Larchmt). 13: 41 &ndash, 53. PMID 15006277.
- ↑ Uffe Ravnskov. The Cholesterol Myths : Exposing the Fallacy that Saturated Fat and Cholesterol Cause Heart Disease. New Trends Publishing, Incorporated. ISBN 0-96708-970-0.
- ↑ Daniel Steinberg. The Cholesterol Wars: The Cholesterol Skeptics vs the Preponderance of Evidence. Boston: Academic Press. ISBN 0-12-373979-9.
- ↑ Nutrition and Your Health: Dietary Guidelines for Americans. Table E-18. Dietary Sources of Cholesterol Listed in Decreasing Order.
- ↑ Behrman EJ, Gopalan V. Cholesterol and plants. J Chem Educ 2005;82:1791-1793. PDF
- ↑ Ostlund RE, Racette, SB, and Stenson WF (2003). "Inhibition of cholesterol absorption by phytosterol-replete wheat germ compared with phytosterol-depleted wheat germ". Am J Clin Nutr. 77 (6): 1385–1589. PMID 12791614.
External links
- Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults US National Institutes of Health Adult Treatment Panel III
- Aspects of fat digestion and metabolism - UN/WHO Report 1994
- American Heart Association - "About Cholesterol"
ar:كولسترول az:Xolesterin bg:Холестерол ca:Colesterol cs:Cholesterol da:Kolesterol de:Cholesterin et:Kolesterool el:Χοληστερίνη eo:Kolesterolo fa:کلسترول ko:콜레스테롤 id:Kolesterol it:Colesterolo he:כולסטרול lt:Cholesterolis ml:കൊളസ്ട്രോള് nl:Cholesterol no:Kolesterol oc:Colesteròl simple:Cholesterol sk:Cholesterol sr:Холестерол fi:Kolesteroli sv:Kolesterol th:คอเลสเตอรอล uk:Холестерин zh-yue:膽固醇