Bronchogenic cyst pathophysiology
|
Bronchogenic cyst Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Bronchogenic cyst pathophysiology On the Web |
|
American Roentgen Ray Society Images of Bronchogenic cyst pathophysiology |
|
Risk calculators and risk factors for Bronchogenic cyst pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Joanna Ekabua, M.D. [2] Kalsang Dolma, M.B.B.S.[3]
Overview
It is thought that bronchogenic cyst is the result of abnormal budding of the ventral [1] portion of the primitive foregut[2][3][4]destined to become the tracheobronchial tree[5] between days 26 - 40 of gestation. [5] At such, it is often found in relation to the trachea or esophagus.[6] On rare occasions, they may be found in the cranial, cervical, mediastinal, and abdominal regions. If the cell mass maintains its connection with the tracheobronchial tree, the cyst becomes intrapulmonary or in close association with the lungs. If separated, there is no contiunity with the bronchia lumen. Such cyst increases in size gradually due to secretions produced within the cavity, leading to compressive symptoms.[2][7]
Gross pathology
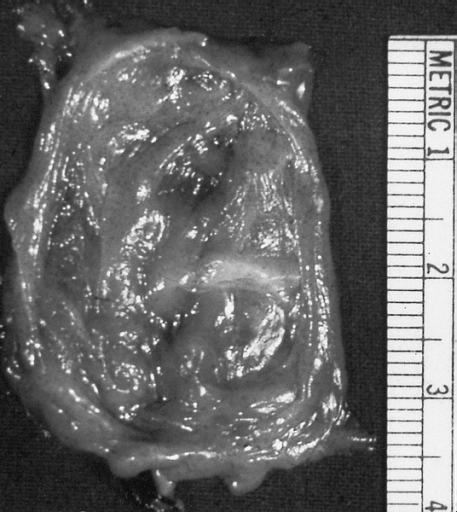
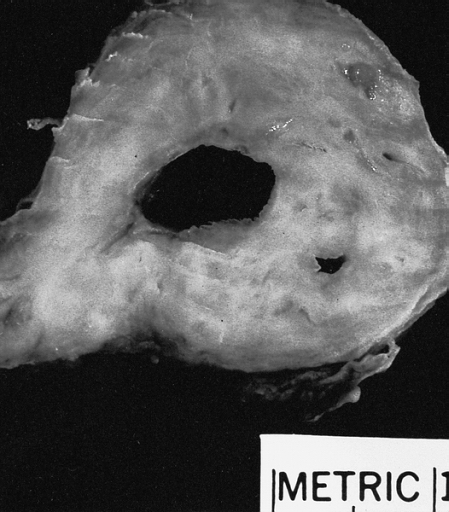
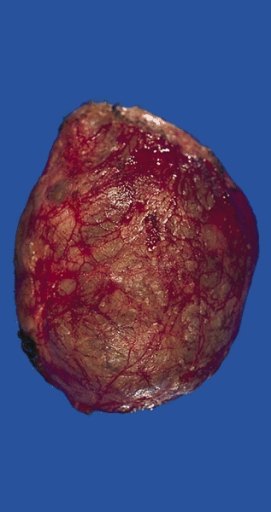
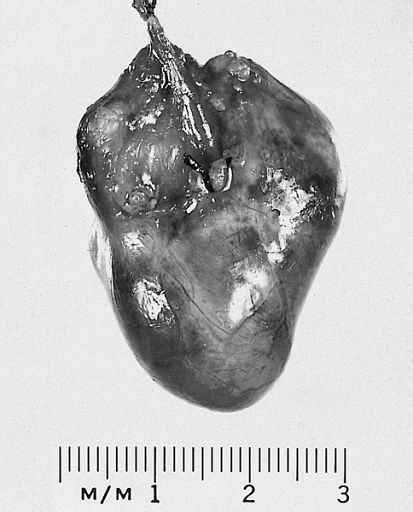
Bronchogenic cyst appear as single or multiple smooth spherical pink masses which may be unlobulated or lobulated. [5][2] The lobules could be of various sizes, communicating or noncommunicating. The wall is relatively thin and frequently trabeculated,[2] even though there may be thicker portions. Cyst often appear to have check valves,[8] leading to their enlargement from secretions by its clilated columnar epithelium. Secretions may be a thick, white mucoid material if uninfected, and a dirty brown mucoid to purulent material if infected.[2] Occassionally, secretions could be hemorrhagic or pneumatic.[3]


Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
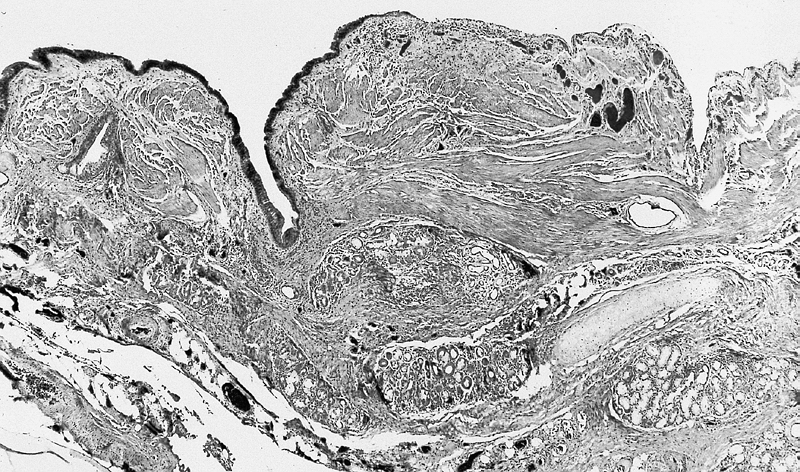
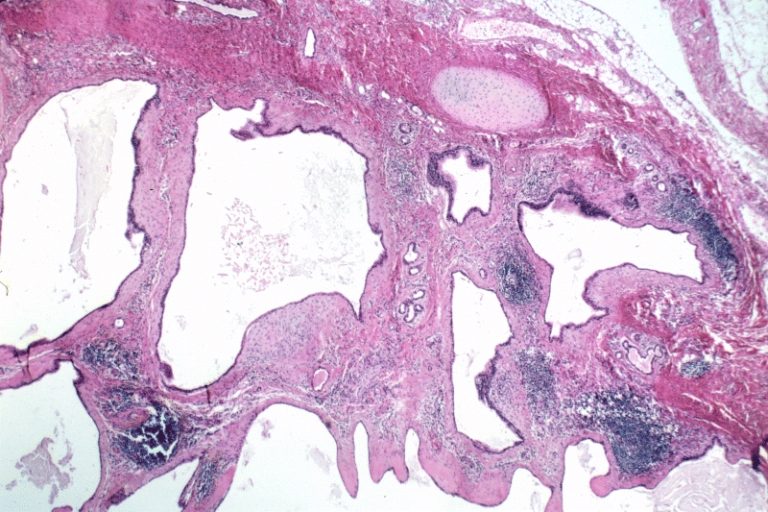
Lower Respiratory Tract: Bronchogenic cysts are grossly nondescript, usually unilocular cavities containing mucus or mucopurulent material with a wall that varies in thickness and may contain cartilage.
-
Lower Respiratory Tract: Bronchogenic cysts are grossly nondescript, usually unilocular cavities containing mucus or mucopurulent material with a wall that varies in thickness and may contain cartilage.
-
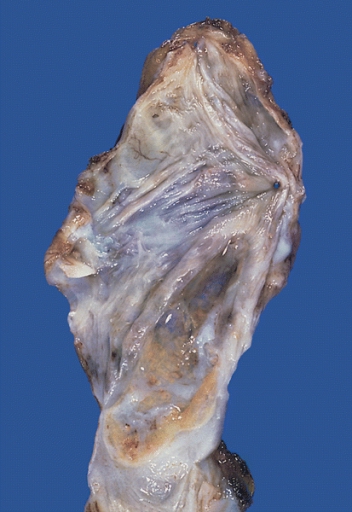
Mediastinum: Bronchogenic cyst; A thin-walled cyst which was present in the posterior mediastinum is distended with slightly cloudy somewhat mucinous fluid.
-
Heart-Great Vessels: Bronchogenic cyst; This example was removed from the epicardial surface of a 13-year-old.
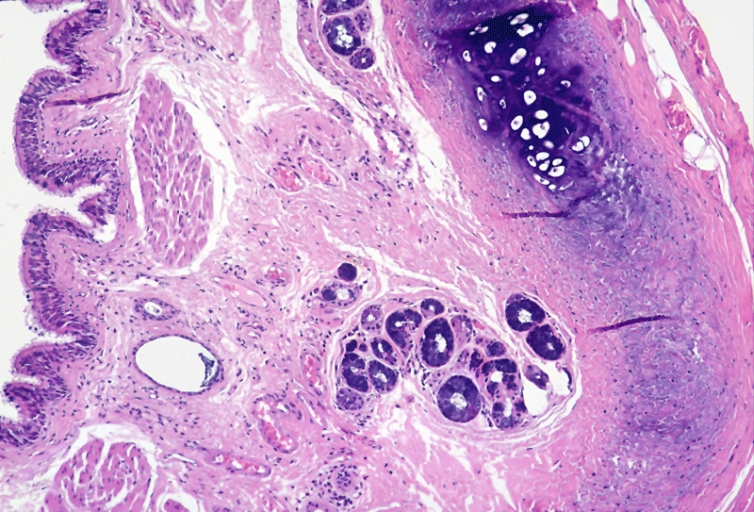
Histopathology
Bronchogenic cysts are usually lined by ciliated columnar epithelium of respiratory type, leading to distention as a result of secretions produced within the cavity. Cyst wall may be composed of cartilage, smooth muscle, fibrous tissue, chronic inflammatory infiltrates, necrotic tissue, focal areas of squamous metaplasia, vascular proliferation, bronchial gland, and mucous glands.[5] [2] [9] [4][10]
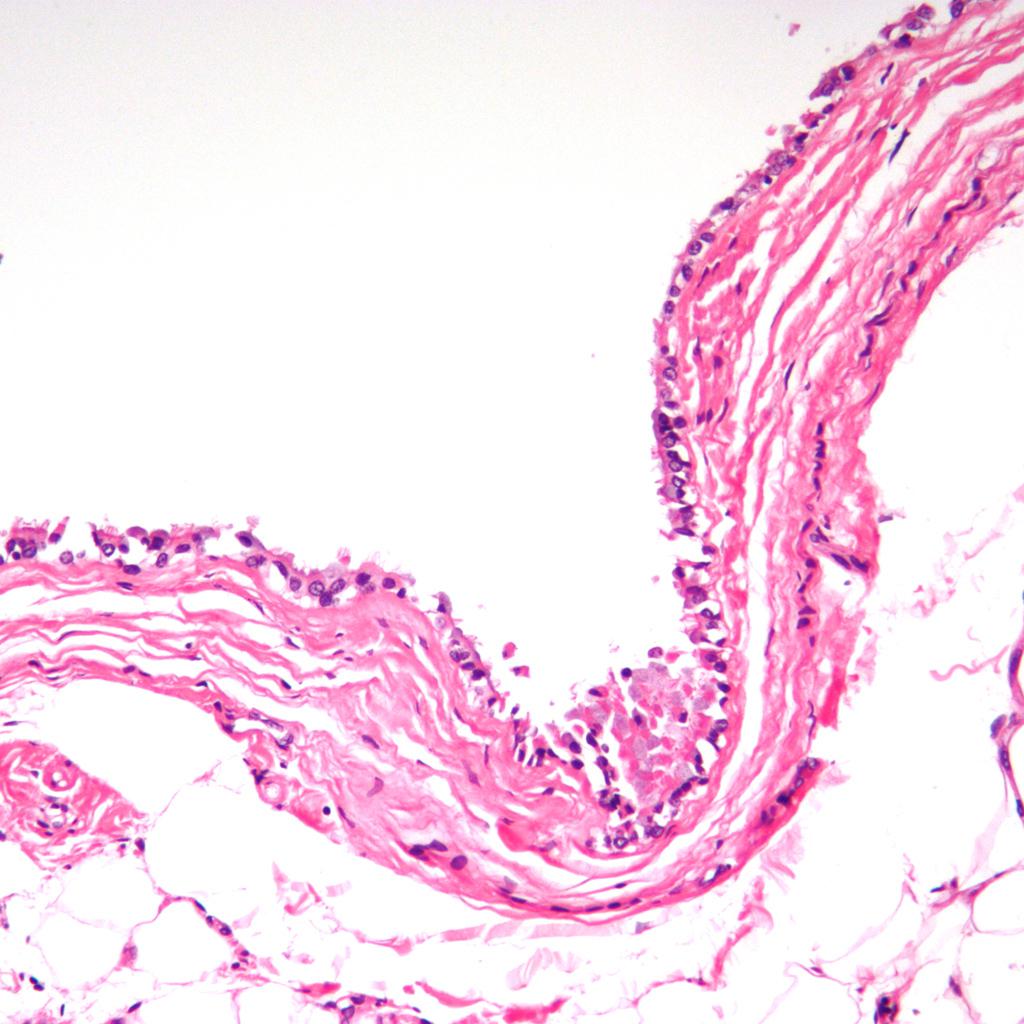

Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
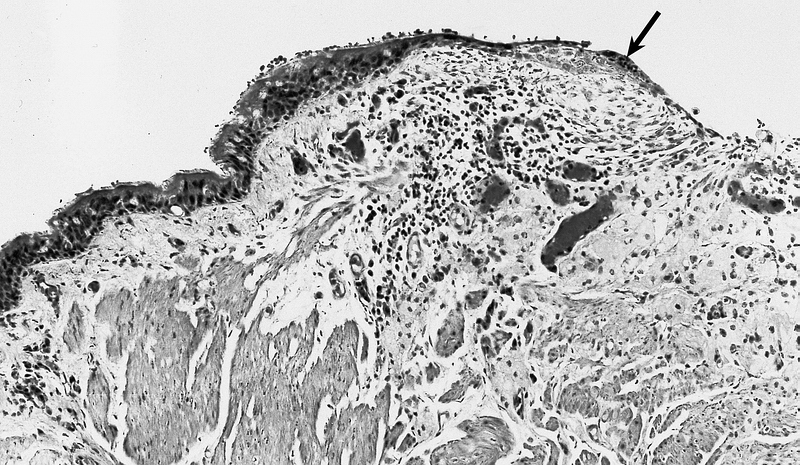
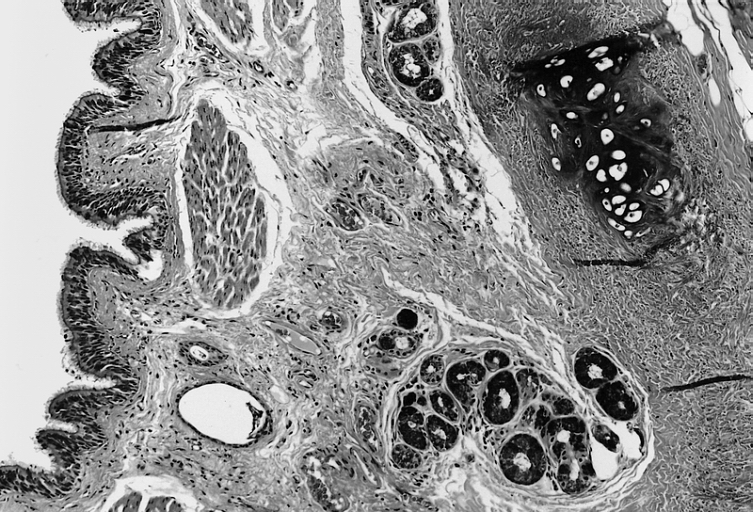
Lower Respiratory Tract: Intrathoracic bronchogenic cyst; Histologically, smooth muscle bundles, minor salivary gland type tissue, and cartilage can be seen in the wall of the cyst.
-
Lower Respiratory Tract: Intrathoracic bronchogenic cyst; The lining is typically pseudostratified ciliated columnar epithelium which may show foci of squamous metaplasia at sites of inflammation (arrow).
-
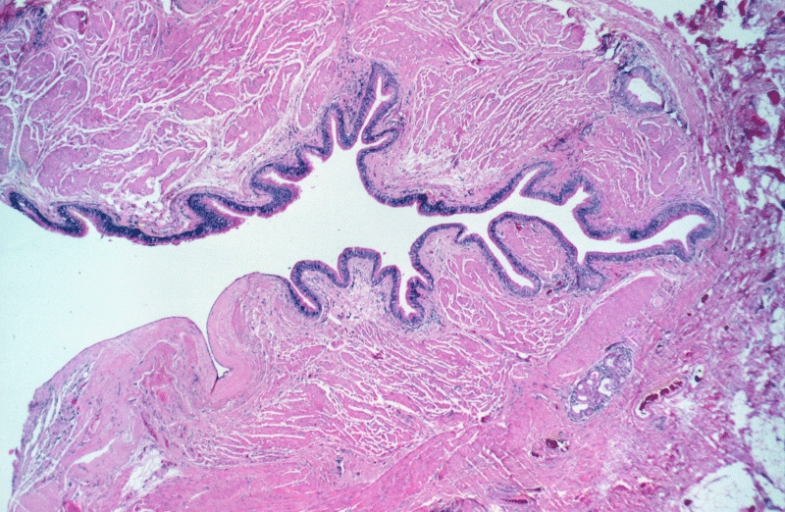
Lower Respiratory Tract: Bronchogenic cyst; There is a cyst lined by bronchiolar epithelium and thick fascicles of smooth muscle in the wall. Islands of cartilage and submucosal salivary glands are lacking and the designation "foregut cyst consistent with bronchogenic cyst" might be more appropriate.
-
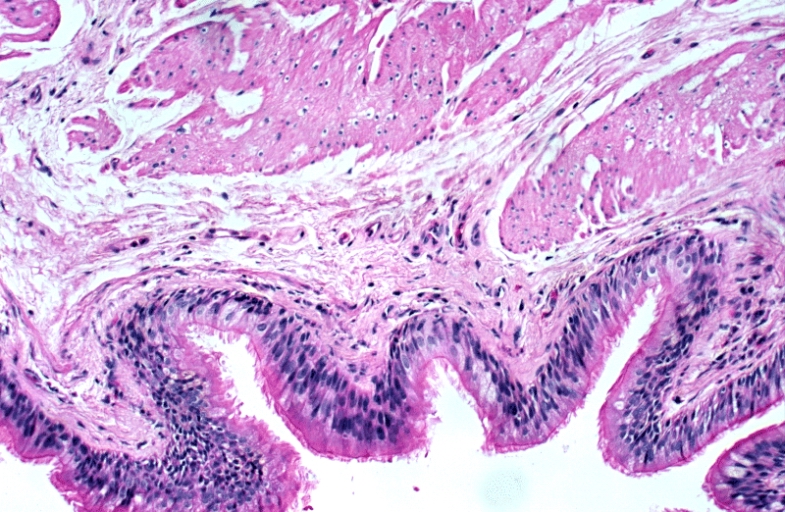
Lower Respiratory Tract: Bronchogenic cyst; There is a cyst lined by bronchiolar epithelium and thick fascicles of smooth muscle in the wall. Islands of cartilage and submucosal salivary glands are lacking and the designation "foregut cyst consistent with bronchogenic cyst" might be more appropriate.
-
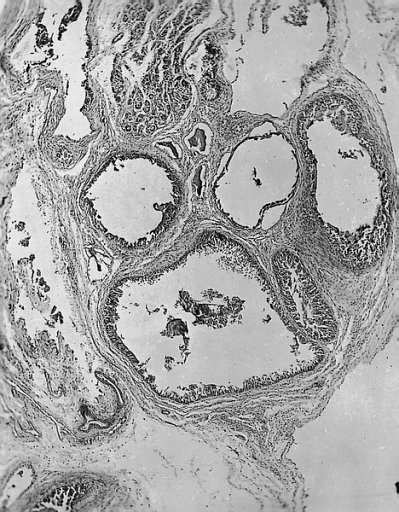
Lower Respiratory Tract: Bronchogenic cyst; There is a multiloculated cyst lined by bronchiolar epithelium. A small island of cartilage is present at the upper right.
-
Heart-Great Vessels: Bronchogenic cyst; The lining cells are cuboidal, and the cysts are surrounded by muscle and may contain underlying seromucous glands.
-
Mediastinum: Bronchogenic cyst; The inner surface is smooth and trabeculated in areas.
-
Mediastinum: Bronchogenic cyst; The cyst is lined by pseudostratified ciliated columnar epithelial cells and the wall contains accessory glands, layers of smooth muscle, and cartilage.
-
Mediastinum: Bronchogenic cyst; The cyst is lined by pseudostratified ciliated columnar epithelial cells and the wall contains accessory glands, layers of smooth muscle, and cartilage.
References
- ↑ Han C, Lin R, Yu J, Zhang Q, Zhang Y, Liu J; et al. (2016). "A Case Report of Esophageal Bronchogenic Cyst and Review of the Literature With an Emphasis on Endoscopic Ultrasonography Appearance". Medicine (Baltimore). 95 (11): e3111. doi:10.1097/MD.0000000000003111. PMC 4839937. PMID 26986156.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Maier HC (1948). "Bronchiogenic Cysts of the Mediastinum". Ann Surg. 127 (3): 476–502. doi:10.1097/00000658-194803000-00010. PMC 1513836. PMID 17859095.
- ↑ 3.0 3.1 Sarper A, Ayten A, Golbasi I, Demircan A, Isin E (2003). "Bronchogenic cyst". Tex Heart Inst J. 30 (2): 105–8. PMC 161894. PMID 12809250.
- ↑ 4.0 4.1 Teissier N, Elmaleh-Bergès M, Ferkdadji L, François M, Van den Abbeele T (2008). "Cervical bronchogenic cysts: usual and unusual clinical presentations". Arch Otolaryngol Head Neck Surg. 134 (11): 1165–9. doi:10.1001/archotol.134.11.1165. PMID 19015445.
- ↑ 5.0 5.1 5.2 5.3 "StatPearls". 2020. PMID 30725658.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID https://doi.org/10.1186/1749-8090-7-94 Check
|pmid=value (help). - ↑ Suda K, Sueyoshi R, Okawada M, Koga H, Lane GJ, Yamataka A; et al. (2015). "Completely intramural bronchogenic cyst of the cervical esophagus in a neonate". Pediatr Surg Int. 31 (7): 683–7. doi:10.1007/s00383-015-3720-1. PMID 26002606.
- ↑ Ribet ME, Copin MC, Gosselin BH (1996). "Bronchogenic cysts of the lung". Ann Thorac Surg. 61 (6): 1636–40. doi:10.1016/0003-4975(96)00172-5. PMID 8651761.
- ↑ Mehta RP, Faquin WC, Cunningham MJ (2004). "Cervical bronchogenic cysts: a consideration in the differential diagnosis of pediatric cervical cystic masses". Int J Pediatr Otorhinolaryngol. 68 (5): 563–8. doi:10.1016/j.ijporl.2003.12.015. PMID 15081229.
- ↑ Aktoğu S, Yuncu G, Halilçolar H, Ermete S, Buduneli T (1996). "Bronchogenic cysts: clinicopathological presentation and treatment". Eur Respir J. 9 (10): 2017–21. doi:10.1183/09031936.96.09102017. PMID 8902460.