Atopic dermatitis physical examination
|
Atopic dermatitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Atopic dermatitis physical examination On the Web |
|
American Roentgen Ray Society Images of Atopic dermatitis physical examination |
|
Risk calculators and risk factors forAtopic dermatitis physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Shalinder Singh, M.B.B.S.[2]
Overview
Atopic dermatitis is a chronic or relapsing hypersensitive manifestation of the skin. Common physical examination findings of atopic dermatitis include pruritus, eczematous lesions, xerosis and lichenification. The lesions are usually age-specific and can be at various stages of development. The lesions can involve any area of the body in severe cases, but usually, it is uncommon to find lesions in the axillary, gluteal, or groin area.
Physical Examination
The clinical presentation of atopic dermatitis is highly variable, depending upon the patient's age and disease activity.[1]
Appearance of the Patient
- Patients with atopic dermatitis usually appear normal.
Vital Signs
- Vitals signs in atopic dermatitis patients are usually within normal limits.
Skin
Primary findings:
- Primary findings are present in all cases of atopic dermaitis.[2]
Other findings:
- Symmetrical lesions
- Constant scratching may lead to lichenification
- An acute eczematoid eruption (with erythematous papules) appears after patients scratch their skin.
- Most severe form of atopic dermatitis can include erythroderma
Typical morphology and distribution:
- Eczematous dermatitis:[3]erythema is more frequently violaceous or even invisible in Black patients. The
lesions are characterized by papules, papulovesicles, edema, crusting, and scaling
| Acute atopic dermatitis | Subacute or chronic atopic dermatitis |
|---|---|
|
|
Age-specific patterns:
| Infants and young children(zero to two years) | ||
|---|---|---|
| ||
| Older children and adolescents (2 to 16 years) | ||
| ||
| Adults (from puberty onward) | ||
| ||
Associated symptoms with atopic dermatitis:[6][1]
| Atopic stigmata
(associated cutaneous findings seen in atopic dermatitis patients) | ||
|---|---|---|
| ||
Clinical phenotypes of atopic dermatitis:
- Localized and morphological variants of atopic dermatitis are present in both children and adults.
- These variants can present as only clinical features of atopic dermatitis or can present in association with age-related manifestations.
| Different phenotypes of atopic dermatitis[7] | |
|---|---|
| |
| Localized variants | Morphological variants |
| |
- Localized variants:[7]
- Atopic hand eczema:[8][1]
- Atopic hand eczema typically affects volar wrists and dorsum of the hands[1]
- One-third of patients with atopic hand eczema, also reports foot eczema[9]
- Common in adults with past medical history of history of atopic dermatitis, and currently do not have dermatitis in typical areas (i.e. flexural)
- Most common in adults exposed to wet environments
- Eyelid eczema:[10]
- Some patients of atopic dermatitis, may present with eyelid eczema alone
- Associated with lichenification and presence of Dennie-Morgan lines
- Atopic cheilitis:
- Also known as lip eczema or cheilitis sicca
- Presents as dryness, peeling, and fissuring of the lips
- Juvenile papular dermatitis:[11]
- Primarily occurs in the spring and summer - associated with pollinosis
- Localized mainly to the elbows and knees
- Juvenile palmar and plantar dermatitis
- Painful variant of atopic dermatitis
- Localized on the anterior part of the sole
- Atopic hand eczema:[8][1]
- Morphological variants:[7]
- Nummular (discoid eczema):
- Sharply demarcated patches and plaques with inflammation of skin
- Secondarily infection with Staphylococcus aureus common
- Commonly affected areas- extremities and buttocks
- Very difficult to treat
- Nummular (discoid eczema):
HEENT
- In patients with atopic dermatitis, eczematous lesions can be present on the face, depending on the age of the patients.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic dermatitis
Neck
- Neck examination of patients with atopic dermatitis is usually normal.
- Eczematous lesions can be present depending on the age of the patients.
Lungs
- Pulmonary examination of patients with atopic dermatitis is usually normal.
Heart
- Cardiovascular examination of patients with atopic dermatitis is usually normal.
Abdomen
- Abdominal examination of patients with atopic dermatitis is usually normal.
Back
- In patients with atopic dermatitis, eczematous lesions can be present on the trunk, depending on the age of the patients.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
Genitourinary
- Genitourinary examination of patients with atopic dermatitis is usually normal.
Neuromuscular
- Neuromuscular examination of patients with atopic dermatitis is usually normal.
Extremities
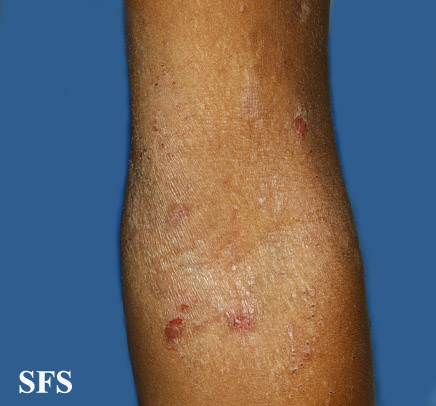
- In patients with atopic dermatitis, eczematous lesions can be present on extremities, depending on the age of the patients.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic Dermatitis. Adapted from Dermatology Atlas.
-
Atopic dermatitis
(Images courtesy of Charlie Goldberg, M.D.)
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Ständer, Sonja; Ropper, Allan H. (2021). "Atopic Dermatitis". New England Journal of Medicine. 384 (12): 1136–1143. doi:10.1056/NEJMra2023911. ISSN 0028-4793.
- ↑ Thestrup-Pedersen, K. (2000). "Clinical aspects of atopic dermatitis". Clinical and Experimental Dermatology. 25 (7): 535–543. doi:10.1046/j.1365-2230.2000.00696.x. ISSN 0307-6938.
- ↑ "Japanese Dermatological Association Criteria for the diagnosis of atopic dermatitis". The Journal of Dermatology. 29 (6): 398–398. 2002. doi:10.1111/j.1346-8138.2002.tb00292.x. ISSN 0385-2407.
- ↑ Rudikoff D, Lebwohl M (June 1998). "Atopic dermatitis". Lancet. 351 (9117): 1715–21. doi:10.1016/S0140-6736(97)12082-7. PMID 9734903.
- ↑ Kulthanan K, Samutrapong P, Jiamton S, Tuchinda P (December 2007). "Adult-onset atopic dermatitis: a cross-sectional study of natural history and clinical manifestation". Asian Pac. J. Allergy Immunol. 25 (4): 207–14. PMID 18402293.
- ↑ Rothe, Marti Jill; Grant-Kels, Jane M (1996). "Diagnostic criteria for atopic dermatitis". The Lancet. 348 (9030): 769–770. doi:10.1016/S0140-6736(05)65206-3. ISSN 0140-6736.
- ↑ 7.0 7.1 7.2 Pugliarello S, Cozzi A, Gisondi P, Girolomoni G (January 2011). "Phenotypes of atopic dermatitis". J Dtsch Dermatol Ges. 9 (1): 12–20. doi:10.1111/j.1610-0387.2010.07508.x. PMID 21054785.
- ↑ Simpson EL, Thompson MM, Hanifin JM (September 2006). "Prevalence and morphology of hand eczema in patients with atopic dermatitis". Dermatitis. 17 (3): 123–7. PMID 16956463.
- ↑ Brans R, Hübner A, Gediga G, John SM (August 2015). "Prevalence of foot eczema and associated occupational and non-occupational factors in patients with hand eczema". Contact Derm. 73 (2): 100–7. doi:10.1111/cod.12370. PMID 25716740.
- ↑ Wolf R, Orion E, Tüzün Y (2014). "Periorbital (eyelid) dermatides". Clin. Dermatol. 32 (1): 131–40. doi:10.1016/j.clindermatol.2013.05.035. PMID 24314387.
- ↑ Rasmussen JE (1978). "Sutton's summer prurigo of the elbows". Acta Derm. Venereol. 58 (6): 547–9. PMID 83084.