Ascending cholangitis pathophysiology
|
Ascending cholangitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ascending cholangitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Ascending cholangitis pathophysiology |
|
Risk calculators and risk factors for Ascending cholangitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Anila Hussain, MD [2]
Overview
Main factors that are involved in the pathogenesis of ascending cholangitis include obstruction of the biliary tract, increased intraluminal pressure and the infection of bile. Bacterial contamination alone in absence of obstruction does not usually result in cholangitis. However increased pressure within the biliary system (above 20 cmH2O)[1] resulting from obstruction in the bile duct widens spaces between the cells lining the duct, bringing bacterially contaminated bile in contact with the bloodstream while affecting the function of infection prevention macrophages (Kupffer cells) at the same time. In addition, high biliary pressure also spreads the infection into biliary canaliculi, hepatic veins and perihepatic lymph vessels resulting in bacteremia (bacteria in the bloodstream).
Pathophysiology
Normal Physiology
Bile is produced by the liver, and serves to eliminate cholesterol and bilirubin from the body, as well as emulsifying of fats to make them more soluble in water and aid in their digestion. Bile is formed in the liver by hepatocytes (liver cells) and excreted into the common hepatic duct. Part of the bile is stored in the gall bladder because of back pressure (exerted by the sphincter of Oddi) and may be released at the time of digestion. The gallbladder also concentrates the bile by absorbing water and dissolved salts from it. All bile reaches the duodenum (first part of the small intestine) through the common bile duct and the ampulla of Vater. The sphincter of Oddi, located at the junction of the ampulla of Vater and the duodenum, is a circular muscle that controls the release of both bile and pancreatic secretions into the digestive tract.
The biliary tree is normally relatively free of bacteria because of certain protective mechanisms.
- The sphincter of Oddi acts as a mechanical barrier.
- The biliary system normally has low pressure (8 to 12 cmH2O)[2] and allows bile to flow freely through.
- The continuous forward flow of the bile in the duct flushes bacteria, if present, into the duodenum, and does not allow the establishment of an infection.
- The constitution of bile—bile salts and immunoglobulin secreted by the epithelium of the bile duct also has a protective role.
Pathogenesis
Main factors that are involved in the pathogenesis of ascending cholangitis include
- Obstruction of biliary tract
- Increased intraluminal pressure
- Infection of bile
Bacteria gain entry to the biliary system when normal defense mechanisms are disrupted. Bacterial contamination alone in absence of obstruction does not usually result in cholangitis. However increased pressure within the biliary system (above 20 cmH2O)[1] resulting from obstruction in the bile duct widens spaces between the cells lining the duct, bringing bacterially contaminated bile in contact with the bloodstream. It also adversely affects the function of Kupffer cells, which are specialized macrophage cells that assist in preventing bacteria from entering the biliary system. Finally, increased biliary pressure decreases production of IgA immunoglobulins in the bile[3] . In addition, high biliary pressure spreads the infection into biliary canaliculi, hepatic veins and perihepatic lymph vessels resulting in bacteremia (bacteria in the bloodstream) and gives rise to the systemic inflammatory response syndrome (SIRS) comprising fever (often with rigors), tachycardia, increased respiratory rate and increased white blood cell count; SIRS in the presence of suspected or confirmed infection is called sepsis. Biliary obstruction itself disadvantages the immune system and impairs its capability to fight infection, by impairing the function of certain immune system cells (neutrophil granulocytes) and modifying the levels of immune hormones (cytokines).
In ascending cholangitis, it is assumed that organisms migrate backward up the bile duct from the duodenum as a result of partial obstruction and decreased the function of the sphincter of Oddi or portal venous blood. Other theories about the origin of the bacteria, such as through the portal vein or transmigration from the colon, are considered less likely.
Gross Pathology
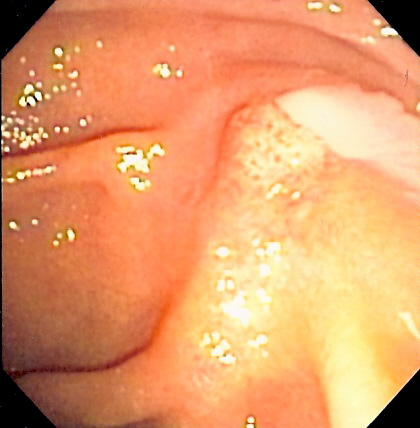
On gross pathology following are characteristic findings of cholangitis[4]
- Thickening of bile ducts
- Bile stasis (cholestasis) as shown by greenish discoloration of parenchyma
- Abscesses or pus in the bile duct, as seen in the picture (seen more commonly in acute suppurative cholangitis)
- Erosions or ulcers in the bile duct
Microscopic Pathology
On microscopic histopathological analysis, the following features are characteristic findings of acute cholangitis:
- Cholestasis of bile canaliculi and/or ducts with or without neutrophils
- Presence of neutrophils in the ductular walls and lumina.
- Acute cholangitis in a patient with multiple bile duct procedures. After the biopsy, removal of bile duct stones released pus[5].
References
- ↑ 1.0 1.1 Huang T, Bass JA, Williams RD (1969). "The significance of biliary pressure in cholangitis". Arch Surg. 98 (5): 629–632. PMID 4888283. Unknown parameter
|month=ignored (help) - ↑ Dooley JS (1999). Oxford textbook of clinical hepatology. Oxford University Press. p. 1650. ISBN 0-19-262515-2.
- ↑ Sung JY, Costerton JW, Shaffer EA (1992). "Defense system in the biliary tract against bacterial infection". Dig Dis Sci. 37 (5): 689–96. doi:10.1007/BF01296423. PMID 1563308. Unknown parameter
|month=ignored (help) - ↑ Fyfe, Billie, and Dylan V. Miller. Diagnostic pathology. Philadelphia, PA: Amirsys/Elsevier, 2016. Print.
- ↑ 9.11.2 Medical Liver disease-Libre Pathology