Tricuspid regurgitation surgery
|
Tricuspid Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tricuspid regurgitation surgery On the Web |
|
American Roentgen Ray Society Images of Tricuspid regurgitation surgery |
|
Risk calculators and risk factors for Tricuspid regurgitation surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2] Fatimo Biobaku M.B.B.S [3]
Overview
Pulmonary hypertension or myocardial disease are two factors that affect the treatment of secondary TR. The surgical approach is considered for selected patients with severe TR (stage C,D) at the time of surgery for left-sided valve lesions and to prevent later development of severe TR in patients with progressive TR (Stage B). For selected patients with isolated TR (either primary TR or secondary TR attributable to annular dilation in the absence of pulmonary hypertension or dilated cardiomyopathy), surgical intervention is recommended. Mortality rate is high in patients undergone interventions for severe isolated TR due to end-organ damage at the time of surgery. However, outcomes of patients with severe primary TR are poor with medical management. Earlier surgery for patients with severe isolated TR before the onset of severe RV dysfunction or end-organ damage is recommended.
Surgery
Indications for Surgery
| Recommendations for intervention in tricuspid valve disease | |
| Primary Tricuspid Regurgitation (Class I, Level of Evidence C): | |
|
❑Surgery is recommended in patients with severe primary tricuspid regurgitation undergoing left-sided valve surgery | |
| Primary Tricuspid Regurgitation (Class IIa, Level of Evidence C): | |
|
❑Surgery should be considered in patients with moderate primary tricuspid regurgitation undergoing left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class I, Level of Evidence B): | |
|
❑Surgery is recommended in patients with severe secondary tricuspid regurgitation undergoing left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class IIa, Level of Evidence B): | |
|
❑Surgery should be considered in patients with mild or moderate secondary tricuspid regurgitation with a dilated annulus (≥40 mm or >21 mm/m2 by 2D echocardiography) undergoing
left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class IIb, Level of Evidence C): | |
|
❑Transcatheter treatment of symptomatic secondary severe tricuspid regurgitation may be considered in inoperable patients |
| The above table adopted from 2021 ESC Guideline[1] |
|---|
- Severe TR of either a primary or secondary etiology may not improve predictably after treatment of the left-sided valve lesion and reduction of RV afterload; as such, severe TR should be addressed as part of the index procedure.1,2,28–31 Reoperation for severe, isolated TR after left-sided valve surgery is associated with a perioperative mortality rate of 10% to 25%.1,29 Tricuspid valve repair does not add appreciably to the risks of surgery.1,2,28–31 There has been a significant increase in the number of tricuspid valve repairs performed for this indication over the past decade. Tricuspid valve repair is preferable to replacement, but replacement may be necessary if there is marked dilation of the annulus or intrinsic disease of the tricuspid leaflets.28,31 Observational data have shown a lower operative risk with tricuspid valve repair than with replacement, but this may be related to patient selection, given that the latter would be inserted in patients with a severely dilated annulus and abnormal leaflets to prevent recurrent or residual regurgitation. The risks and benefits of tricuspid valve operation should be carefully considered in the presence of severe RV systolic dysfunction or irreversible pulmonary hypertension because of the possibility of RV failure after operation.
2. Left uncorrected at the time of left-sided valve surgery, mild or moderate degrees of secondary TR may progress over time in approximately 25% of patients and result in reduced long-term functional outcome and survival.32 Risk factors for persistence or progression of TR include tricuspid annulus dilation (>40 mm diameter or 21 mm/m2 diameter indexed to body surface area on preoperative TTE measured at end diastole; >70 mm diameter on direct intraoperative measurement of the intercomissural distance), degree of RV dysfunction or remodeling, leaflet tethering height, pulmonary artery hypertension, AF, and intra-annular RV pacemaker or implantable cardioverter-defibrillator leads.3–10,33–36 Several observational studies and one prospective RCT have demonstrated the benefit of tricuspid repair at the time of mitral valve surgery for progressive TR (Stage B) with tricuspid annulus dilation on echocardiographic and functional parameters, although data on outcomes such as survival and major adverse events are lacking.3–10,33–35 Because the severity of TR may be dynamic, dependent on the preload and pulmonary pressures, a past history of signs or symptoms of right-sided HF indicates the propensity to develop more severe TR and should be considered an indication for concomitant tricuspid valve repair. 3. In patients with symptomatic severe primary TR, reduction or elimination of the regurgitant volume load by tricuspid valve surgery can alleviate systemic venous and hepatic congestion and decrease reliance on diuretics.11,12,20 Patients with severe congestive hepatopathy may also benefit from surgery to prevent irreversible cirrhosis of the liver. Quality and duration of long-term survival are related to residual RV function. In patients with severe symptomatic primary TR from either device leads or endomyocardial biopsy, TR develops rapidly, and surgery can be done before the onset of RV dysfunction.11,37 Correction of symptomatic severe primary TR (Stage D) in patients without left-sided valve disease would preferentially be performed before the onset of significant RV dysfunction or end-organ damage. Randomized studies of early intervention are lacking, and the benefit might be limited by the risk of intervention, suboptimal reduction in TR severity, or suboptimal durability of currently available approaches to tricuspid valve repair and replacement. 4. There is now recognition that TR can develop in association with AF and annular dilation (a form of secondary TR).23–25 Notably, AF-related TR appears to represent a fundamentally different pathophysiology from other forms of secondary TR, with greater basal dilation and annular enlargement, as compared with the RV elongation with leaflet tethering seen in patients who have secondary TR caused by pulmonary hypertension or myocardial disease.24 These patients with AF-related TR have rapid progression of TR severity and right-sided chamber dilation. In appropriately selected symptomatic patients with AF-related severe TR, quality of life and symptoms can be improved by surgical intervention for TR. In patients undergoing intervention, overall outcomes are better in those without severe RV dysfunction or end-organ damage. Newer surgical techniques and a better selection process resulted in an acceptable operative mortality rate (<4% to 5%) for isolated TR in selected patients.2,11,12,15–19,22,38 5. The optimal timing of tricuspid valve surgery for asymptomatic or minimally symptomatic patients with severe primary TR has not been established. Extrapolation from limited experiences reported for patients with stable carcinoid heart disease and patients with a flail tricuspid leaflet, as well as application of the management principles adopted for patients with severe MR, suggest that serial assessments of RV size and function might trigger consideration of corrective surgery in selected patients with severe primary TR when a pattern of continued deterioration can be established and the surgical risk is considered acceptable.13,14 In otherwise healthy patients without other comorbidities, such as patients with severe TR attributable to trauma, the surgical risk associated with tricuspid valve operation is low (<1% to 2% operative mortality rate) in the absence of RV dysfunction or pulmonary hypertension. 6. Isolated tricuspid valve surgery for severe TR historically has been performed relatively late in the natural history of the disease, when patients have become symptomatic with signs of right-sided HF. Unadjusted mortality rates for isolated tricuspid valve surgery have therefore exceeded those reported for isolated aortic or mitral valve surgery, and this trend has been even more pronounced for reoperative tricuspid surgery late after left-sided valve surgery.1,2,39 This high reoperative mortality rate is likely related to the advanced nature of RV failure encountered at the time of the second procedure, residual pulmonary hypertension, LV dysfunction, and other valve abnormalities. The hazards imposed by reoperation have influenced decision-making for initial repair of functional TR at the time of left-sided valve surgery in an attempt to prevent the development of severe TR later after the left-sided valve surgery. However, if there is no significant pulmonary hypertension or severe RV systolic dysfunction, operation for severe symptomatic isolated TR years after surgery for left-sided disease may improve symptoms of right-sided HF, if done before the onset of severe RV dysfunction or end-organ damage with either hepatic or renal dysfunction.11,18
Surgical Methods
Annuloplasty
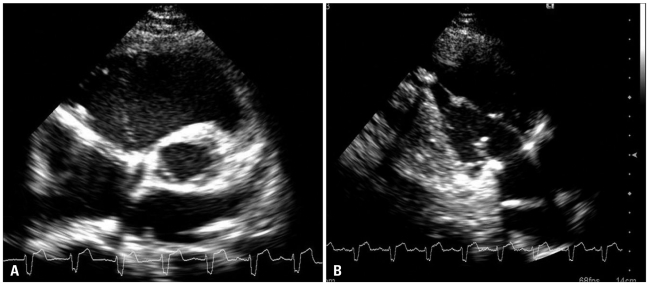
The principal surgical repair for secondary TR is tricuspid annuloplasty. The aim of tricuspid annuloplasty is to improve leaflet coaptation by correcting annular dilatation and restoring annular geometry. The two principle surgical methods are:[2][3]
- Ring annuloplasty: It is regarded as the standard for surgical repair. The size of the tricuspid annulus is permanently fixed by implantation of a rigid or semi rigid prosthesis, undersized ring, and it is associated with a reduced incidence of late, recurrent tricuspid regurgitation.
- Suture annuloplasty: It is technically easy and can be done quickly. Also, compared with the ring annuloplasty, a prosthetic implant is not used with suture annuloplasty and the risk of postoperative conduction disturbances is lower.
Other methods:[2]
- Adjunctive repair techniques: This may be necessary for augmentation of the effects of the ring annuloplasty in patients with marked leaflet tethering and right ventricular remodeling. The long-term outcomes and durability of these adjunctive techniques are not well established. Types of adjunctive repair techniques are listed in the table below.
| Anterior leaflet augmentation using an autologous pericardial patch | ''Clover'' technique | Double orifice valve technique |
|---|---|---|
| Helps improve leaflet coaptation while maintaining leaflet mobility |
|
|
- Tricuspid valve replacement
- Should be undertaken when valve repair is not technically feasible or predictably durable.
- Valve repair should be considered as the first option in patients with secondary tricuspid regurgitation and marked right ventricular remodeling and leaflet tethering, and in patients with complex primary tricuspid regurgitation or severe tricuspid stenosis.
- Bioprosthetic valves are currently favored, however, no differences in survival or adverse events at long-term follow-up have been recorded in patients receiving mechanical or biological valves.
- Transcatheter therapies
- The safety and feasibility of transcatheter therapies for treating severe tricuspid regurgitation are still being investigated.
- Three types of transcatheter therapies have recently emerged for treating severe tricuspid regurgitation:
- Heterotopic caval transcatheter valve implantation
- Transcatheter tricuspid valve annuloplasty
- Coaptation device
- Transcatheter tricuspid valve replacement
- This is an experimental study that has been carried out in animals (ewes), it is yet to be done in humans.[5]
References
- ↑ Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, Conradi L, De Bonis M, De Paulis R, Delgado V, Freemantle N, Gilard M, Haugaa KH, Jeppsson A, Jüni P, Pierard L, Prendergast BD, Sádaba JR, Tribouilloy C, Wojakowski W (February 2022). "2021 ESC/EACTS Guidelines for the management of valvular heart disease". Eur Heart J. 43 (7): 561–632. doi:10.1093/eurheartj/ehab395. PMID 34453165 Check
|pmid=value (help). - ↑ 2.0 2.1 Rodés-Cabau J, Taramasso M, O'Gara PT (2016). "Diagnosis and treatment of tricuspid valve disease: current and future perspectives". Lancet. 388 (10058): 2431–2442. doi:10.1016/S0140-6736(16)00740-6. PMID 27048553 PMID: 27048553 Check
|pmid=value (help). - ↑ Taramasso M, Vanermen H, Maisano F, Guidotti A, La Canna G, Alfieri O (2012). "The growing clinical importance of secondary tricuspid regurgitation". J Am Coll Cardiol. 59 (8): 703–10. doi:10.1016/j.jacc.2011.09.069. PMID 22340261.
- ↑ "A Case of Traumatic Tricuspid Regurgitation Caused by Multiple Papillary Muscle Rupture".
- ↑ Boudjemline Y, Agnoletti G, Bonnet D, Behr L, Borenstein N, Sidi D et al. (2005) Steps toward the percutaneous replacement of atrioventricular valves an experimental study. J Am Coll Cardiol 46 (2):360-5. DOI:10.1016/j.jacc.2005.01.063 PMID: 16022968 PMID 16022968