Tricuspid regurgitation surgery: Difference between revisions
(/* 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852) |
|||
| Line 145: | Line 145: | ||
* '''Transcatheter tricuspid valve replacement''' | * '''Transcatheter tricuspid valve replacement''' | ||
**This is an experimental study that has been carried out in animals (ewes), it is yet to be done in humans.<ref name="pmid16022968">Boudjemline Y, Agnoletti G, Bonnet D, Behr L, Borenstein N, Sidi D et al. (2005) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=16022968 Steps toward the percutaneous replacement of atrioventricular valves an experimental study.] ''J Am Coll Cardiol'' 46 (2):360-5. [http://dx.doi.org/10.1016/j.jacc.2005.01.063 DOI:10.1016/j.jacc.2005.01.063] PMID: [https://pubmed.gov/PMID 16022968 PMID 16022968]</ref> | **This is an experimental study that has been carried out in animals (ewes), it is yet to be done in humans.<ref name="pmid16022968">Boudjemline Y, Agnoletti G, Bonnet D, Behr L, Borenstein N, Sidi D et al. (2005) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=16022968 Steps toward the percutaneous replacement of atrioventricular valves an experimental study.] ''J Am Coll Cardiol'' 46 (2):360-5. [http://dx.doi.org/10.1016/j.jacc.2005.01.063 DOI:10.1016/j.jacc.2005.01.063] PMID: [https://pubmed.gov/PMID 16022968 PMID 16022968]</ref> | ||
==2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) <ref name="pmid18820172">{{cite journal |author=Bonow RO, Carabello BA, Chatterjee K, ''et al.'' |title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons |journal=Circulation |volume=118 |issue=15 |pages=e523–661 |year=2008 |month=October |pmid=18820172 |doi=10.1161/CIRCULATIONAHA.108.190748 |url=}}</ref>== | ==2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) <ref name="pmid18820172">{{cite journal |author=Bonow RO, Carabello BA, Chatterjee K, ''et al.'' |title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons |journal=Circulation |volume=118 |issue=15 |pages=e523–661 |year=2008 |month=October |pmid=18820172 |doi=10.1161/CIRCULATIONAHA.108.190748 |url=}}</ref>== | ||
Revision as of 04:26, 4 June 2022
|
Tricuspid Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tricuspid regurgitation surgery On the Web |
|
American Roentgen Ray Society Images of Tricuspid regurgitation surgery |
|
Risk calculators and risk factors for Tricuspid regurgitation surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2] Fatimo Biobaku M.B.B.S [3]
Overview
Severe primary/secondary tricuspid regurgitation does not predictably improve after left-sided valve surgery, even with correction of any associated pulmonary hypertension, and should be addressed at the time of the index left-sided valve surgery.
Surgery
Indications for Surgery
| Recommendations for intervention in tricuspid valve disease | |
| Primary Tricuspid Regurgitation (Class I, Level of Evidence C): | |
|
❑Surgery is recommended in patients with severe primary tricuspid regurgitation undergoing left-sided valve surgery | |
| Primary Tricuspid Regurgitation (Class IIa, Level of Evidence C): | |
|
❑Surgery should be considered in patients with moderate primary tricuspid regurgitation undergoing left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class I, Level of Evidence B): | |
|
❑Surgery is recommended in patients with severe secondary tricuspid regurgitation undergoing left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class IIa, Level of Evidence B): | |
|
❑Surgery should be considered in patients with mild or moderate secondary tricuspid regurgitation with a dilated annulus (≥40 mm or >21 mm/m2 by 2D echocardiography) undergoing
left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class IIb, Level of Evidence C): | |
|
❑Transcatheter treatment of symptomatic secondary severe tricuspid regurgitation may be considered in inoperable patients |
| The above table adopted from 2021 ESC Guideline[1] |
|---|
- Shown below is an algorithm depicting the indications for tricuspid valve surgery adapted from the 2014 AHA/ACC guideline for the management of patients with valvular heart disease.
- If the patient does not meet any of the decision pathways in the algorithm, regular monitoring with medical therapy is recommended and surgery is not indicated.[2][3]
| Determine the stage of the tricuspid regurgitation (TR) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Progressive functional (Stage B) | Asymptomatic severe (Stage C) | Symptomatic severe (Stage D) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Is TR mild or moderate? | What is the underlying cause of TR? | Has the TR been previously operated on? | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| What is the underlying cause of TR? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Mild | Moderate | Functional | Primary | Functional | Primary | ||||||||||||||||||||||||||||||||||||||||||||||||||
| The patient is undergoing left-sided valve surgery | The patient is undergoing left-sided valve surgery | The patient is experiencing progressive right ventricular dysfunction AND/OR systolic dysfunction | The patient has persistent symptoms AND The patient has preserved right ventricular function and the pulmonary hypertension is not severe | The patient is undergoing left-sided valve surgery | The patient is unresponsive to medical therapy | ||||||||||||||||||||||||||||||||||||||||||||||||||
| The patient has tricuspid annular dilatation OR Prior evidence of right heart failure | The patient has pulmonary hypertension without tricuspid annular dilatation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Tricuspid valve repair (Class IIa) | Tricuspid valve repair (Class IIb) | Tricuspid valve repair or replacement (Class I) | Tricuspid valve repair or replacement (Class IIb) | Tricuspid valve repair or replacement (Class I) | Tricuspid valve repair or replacement (Class IIa) | ||||||||||||||||||||||||||||||||||||||||||||||||||
Surgical Methods
Annuloplasty
The principal surgical repair for secondary TR is tricuspid annuloplasty. The aim of tricuspid annuloplasty is to improve leaflet coaptation by correcting annular dilatation and restoring annular geometry. The two principle surgical methods are:[4][5]
- Ring annuloplasty: It is regarded as the standard for surgical repair. The size of the tricuspid annulus is permanently fixed by implantation of a rigid or semi rigid prosthesis, undersized ring, and it is associated with a reduced incidence of late, recurrent tricuspid regurgitation.
- Suture annuloplasty: It is technically easy and can be done quickly. Also, compared with the ring annuloplasty, a prosthetic implant is not used with suture annuloplasty and the risk of postoperative conduction disturbances is lower.
Other methods:[4]
- Adjunctive repair techniques: This may be necessary for augmentation of the effects of the ring annuloplasty in patients with marked leaflet tethering and right ventricular remodeling. The long-term outcomes and durability of these adjunctive techniques are not well established. Types of adjunctive repair techniques are listed in the table below.
| Anterior leaflet augmentation using an autologous pericardial patch | ''Clover'' technique | Double orifice valve technique |
|---|---|---|
| Helps improve leaflet coaptation while maintaining leaflet mobility |
|
|
- Tricuspid valve replacement
- Should be undertaken when valve repair is not technically feasible or predictably durable.
- Valve repair should be considered as the first option in patients with secondary tricuspid regurgitation and marked right ventricular remodeling and leaflet tethering, and in patients with complex primary tricuspid regurgitation or severe tricuspid stenosis.
- Bioprosthetic valves are currently favored, however, no differences in survival or adverse events at long-term follow-up have been recorded in patients receiving mechanical or biological valves.
- Transcatheter therapies
- The safety and feasibility of transcatheter therapies for treating severe tricuspid regurgitation are still being investigated.
- Three types of transcatheter therapies have recently emerged for treating severe tricuspid regurgitation:
- Heterotopic caval transcatheter valve implantation
- Transcatheter tricuspid valve annuloplasty
- Coaptation device
- Transcatheter tricuspid valve replacement
- This is an experimental study that has been carried out in animals (ewes), it is yet to be done in humans.[7]
2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) [8]
Tricuspid Valve Replacement (DO NOT EDIT) [8]
| Class I |
| "1. Tricuspid valve repair is beneficial for severe TR in patients with mitral valve disease requiring mitral valve surgery. (Level of Evidence: B)" |
| Class III |
| "1. Tricuspid valve replacement or annuloplasty is not indicated in asymptomatic patients with TR whose pulmonary artery systolic pressure is less than 60 mm Hg in the presence of a normal mitral valve. (Level of Evidence: C)" |
| "2. Tricuspid valve replacement or annuloplasty is not indicated in patients with mild primary TR. (Level of Evidence: C)" |
| Class IIa |
| "1. Tricuspid valve replacement or annuloplasty is reasonable for severe primary TR when symptomatic. (Level of Evidence: C)" |
| "2. Tricuspid valve replacement is reasonable for severe TR secondary to diseased/abnormal tricuspid valve leaflets not amenable to annuloplasty or repair. (Level of Evidence: C)" |
| Class IIb |
| "1. Tricuspid valve replacement or annuloplasty is reasonable for severe primary TR when symptomatic. (Level of Evidence: C)" |
Indications for Intervention Adolescents (DO NOT EDIT) [8]
| Class I |
| "1. Surgery for severe TR is recommended for adolescent and young adult patients with deteriorating exercise capacity (NYHA functional class III or IV). (Level of Evidence: C)" |
| "2. Surgery for severe TR is recommended for adolescent and young adult patients with progressive cyanosis and arterial saturation less than 80% at rest or with exercise. (Level of Evidence: C)" |
| "3. Interventional catheterization closure of the atrial communication is recommended for the adolescent or young adult with TR who is hypoxemic at rest and with exercise intolerance due to increasing hypoxemia with exercise, when the tricuspid valve appears difficult to repair surgically. (Level of Evidence: C)" |
| Class IIa |
| "1. Surgery for severe TR is reasonable in adolescent and young adult patients with NYHA functional class II symptoms if the valve appears to be repairable. (Level of Evidence: C)" |
| "2. Surgery for severe TR is reasonable in adolescent and young adult patients with atrial fibrillation. (Level of Evidence: C)" |
| Class IIb |
| "1. Surgery for severe TR may be considered in asymptomatic adolescent and young adult patients with increasing heart size and a cardiothoracic ratio of more than 65%. (Level of Evidence: C)" |
| "2. Surgery for severe TR may be considered in asymptomatic adolescent and young adult patients with stable heart size and an arterial saturation of less than 85% when the tricuspid valve appears repairable. (Level of Evidence: C)" |
| "3. In adolescent and young adult patients with TR who are mildly cyanotic at rest but who become very hypoxemic with exercise, closure of the atrial communication by interventional catheterization may be considered when the valve does not appear amenable to repair. (Level of Evidence: C)" |
| "4. If surgery for Ebstein’s anomaly is planned in adolescents and young adult patients (tricuspid valve repair or replacement), a preoperative electrophysiological study may be considered to identify accessory pathways. If present, these may be considered for mapping and ablation either preoperatively or at the time of surgery. (Level of Evidence: C)" |
Tricuspid Valve Surgery (DO NOT EDIT) [8]
| Class I |
| "1. Severe TR in the setting of surgery for multivalvular disease should be corrected. (Level of Evidence: C)" |
| Class IIa |
| "1. Tricuspid annuloplasty is reasonable for mild TR in patients undergoing MV surgery when there is pulmonary hypertension or tricuspid annular dilatation. (Level of Evidence: C)" |
Intraoperative Assessment (DO NOT EDIT) [8]
| Class I |
| "1. Intraoperative transesophageal echocardiography is recommended for valve repair surgery. (Level of Evidence: B)" |
| "2. Intraoperative transesophageal echocardiography is recommended for valve replacement surgery with a stentless xenograft, homograft, or autograft valve.(Level of Evidence: B)" |
| Class IIa |
| "1. Intraoperative transesophageal echocardiography is reasonable for all patients undergoing cardiac valve surgery. (Level of Evidence: C)" |
References
- ↑ Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, Conradi L, De Bonis M, De Paulis R, Delgado V, Freemantle N, Gilard M, Haugaa KH, Jeppsson A, Jüni P, Pierard L, Prendergast BD, Sádaba JR, Tribouilloy C, Wojakowski W (February 2022). "2021 ESC/EACTS Guidelines for the management of valvular heart disease". Eur Heart J. 43 (7): 561–632. doi:10.1093/eurheartj/ehab395. PMID 34453165 Check
|pmid=value (help). - ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Rodés-Cabau J, Taramasso M, O'Gara PT (2016). "Diagnosis and treatment of tricuspid valve disease: current and future perspectives". Lancet. 388 (10058): 2431–2442. doi:10.1016/S0140-6736(16)00740-6. PMID 27048553.
- ↑ 4.0 4.1 Rodés-Cabau J, Taramasso M, O'Gara PT (2016). "Diagnosis and treatment of tricuspid valve disease: current and future perspectives". Lancet. 388 (10058): 2431–2442. doi:10.1016/S0140-6736(16)00740-6. PMID 27048553 PMID: 27048553 Check
|pmid=value (help). - ↑ Taramasso M, Vanermen H, Maisano F, Guidotti A, La Canna G, Alfieri O (2012). "The growing clinical importance of secondary tricuspid regurgitation". J Am Coll Cardiol. 59 (8): 703–10. doi:10.1016/j.jacc.2011.09.069. PMID 22340261.
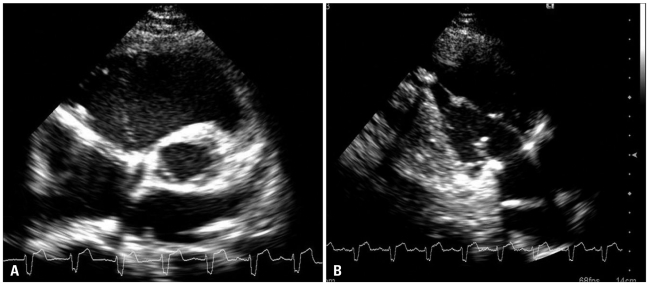
- ↑ "A Case of Traumatic Tricuspid Regurgitation Caused by Multiple Papillary Muscle Rupture".
- ↑ Boudjemline Y, Agnoletti G, Bonnet D, Behr L, Borenstein N, Sidi D et al. (2005) Steps toward the percutaneous replacement of atrioventricular valves an experimental study. J Am Coll Cardiol 46 (2):360-5. DOI:10.1016/j.jacc.2005.01.063 PMID: 16022968 PMID 16022968
- ↑ 8.0 8.1 8.2 8.3 8.4 Bonow RO, Carabello BA, Chatterjee K; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172. Unknown parameter
|month=ignored (help)