Supraventricular tachycardia: Difference between revisions
No edit summary |
No edit summary |
||
| (107 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="-webkit-user-select: none;"> | |||
{| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" | |||
|- | |||
|- | |||
|} | |||
__NOTOC__ | |||
{| class="infobox" style="float:right;" | |||
|- | |||
|} | |||
'''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | |||
{{ | |||
{{CMG}}; {{AE}} {{AIA}} | |||
{{SK}} SVT | |||
==Overview== | |||
There are several classification systems for [[supraventricular tachycardia]], based on site of origin, [[QRS complex|QRS]] width, pulse regularity, and [[Atrioventricular node|AV node]] dependence. There are different types of [[supraventricular tachycardia]], including [[sinus tachycardia]], [[inappropriate sinus tachycardia]], sinus node re-entry tachycardia, [[atrial fibrillation]], atrial flutter, [[AV nodal reentrant tachycardia|AV nodal re-entry tachycardia]], AV reciprocating tachycardia, [[junctional tachycardia]], [[multifocal atrial tachycardia]], and [[Wolff-Parkinson-White syndrome|Wolff-Parkinson White]] syndrome. The general symptoms of SVTs include [[anxiety]], [[chest pain]] or sensation of tightness, [[dizziness]] or [[fainting]], [[Palpitation|palpitations]], [[shortness of breath]], [[syncope]] in cases of [[AVNRT]], and [[sweating]]. The individual subtypes of SVT can be distinguished from each other by certain physiological and electrical characteristics, many of which present in the patient's EKG. [[Supraventricular tachycardias]] must be differentiated from each other because the management strategies may vary. In general, [[SVT]] is not life threatening, but episodes should be treated or prevented. While some treatment modalities can be applied to all SVTs with impunity, there are specific therapies available to cure some of the different sub-types. Cure requires intimate knowledge of how and where the [[arrhythmia]] is initiated and propagated. SVTs can be separated into two groups, based on whether they involve the [[Atrioventricular node|AV node]] for impulse maintenance or not. Those that involve the [[AV node]] can be terminated by slowing conduction through the [[Atrioventricular node|AV node]]. Those that do not involve the AV node will not usually be stopped by AV nodal blocking maneuvers. These maneuvers are still useful however, as transient [[AV block]] will often unmask the underlying rhythm abnormality. Once the acute episode has been terminated, ongoing treatment may be indicated to prevent a recurrence of the [[Cardiac arrhythmia|arrhythmia]]. Patients who have a single isolated episode, or infrequent and minimally symptomatic episodes usually do not warrant any treatment except observation. Patients who have more frequent or disabling symptoms from their episodes generally warrant some form of preventative therapy. A variety of drugs including simple AV nodal blocking agents like [[Beta-blocker|beta-blockers]] and [[verapamil]], as well as [[antiarrhythmics]] may be used, usually with good effect, although the risks of these therapies need to be weighed against the potential benefits. | |||
The individual subtypes of SVT can be distinguished from each other by certain physiological and electrical characteristics, many of which present in the patient's EKG. | |||
== | ==Classification== | ||
There are several classification systems for [[supraventricular tachycardia]], based on site of origin, [[QRS complex|QRS]] width, pulse regularity, and [[Atrioventricular node|AV node]] dependence.<ref name="pmid28835834">{{cite journal| author=Lundqvist CB, Potpara TS, Malmborg H| title=Supraventricular Arrhythmias in Patients with Adult Congenital Heart Disease. | journal=Arrhythm Electrophysiol Rev | year= 2017 | volume= 6 | issue= 2 | pages= 42-49 | pmid=28835834 | doi=10.15420/aer.2016:29:3 | pmc=5517371 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28835834 }} </ref><ref name="pmid28833859">{{cite journal| author=Massari F, Scicchitano P, Potenza A, Sassara M, Sanasi M, Liccese M | display-authors=etal| title=Supraventricular tachycardia, pregnancy, and water: A new insight in lifesaving treatment of rhythm disorders. | journal=Ann Noninvasive Electrocardiol | year= 2018 | volume= 23 | issue= 3 | pages= e12490 | pmid=28833859 | doi=10.1111/anec.12490 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28833859 }} </ref> | |||
*[[Supraventricular tachycardia]] can be classified based on the site of origin into: | |||
** Physiological [[sinus tachycardia]] | |||
**[[Atrial tachycardia]] | |||
**[[Atrioventricular]] tachycardia | |||
*[[Supraventricular tachycardia]] can be classified based on [[QRS complex|QRS]] width into: | |||
**Narrow complex tachycardia: [[Sinus tachycardia]], [[atrial flutter]], [[atrial fibrillation]], focal/[[multifocal atrial tachycardia]], Sinus node re-entry, [[AV nodal reentrant tachycardia|AVNRT]], and [[junctional tachycardia]]. | |||
**Wide complex tachycardia: AF with aberrations and [[Atrial fibrillation|AF]] with [[Wolff-Parkinson-White syndrome|WPW]]. | |||
*[[Supraventricular tachycardia]] can be classified based on pulse regularity into: | |||
**Regular: [[Sinus tachycardia]], [[atrial flutter]], Sinus node re-entry tachycardia, [[AV nodal reentrant tachycardia|AVNRT]], and [[junctional tachycardia]]. | |||
**Irregular: [[Atrial fibrillation]] and [[multifocal atrial tachycardia]] | |||
*[[Supraventricular tachycardia]] can be classified based on [[Atrioventricular node|AV node]] dependence into: | |||
**AV node dependent: [[AV nodal reentrant tachycardia|AVNRT]]<nowiki/>s and AVRTs | |||
**AV node independent: [[Focal atrial tachycardia]] and [[atrial flutter]] | |||
*** | |||
AV nodal | ==Causes== | ||
===Causes by Organ System=== | |||
There are several causes of [[supraventricular tachycardia]] in almost all body systems.<ref name="pmid28376069">{{cite journal| author=Corwin DJ, Scarfone RJ| title=Supraventricular Tachycardia Associated With Severe Anemia. | journal=Pediatr Emerg Care | year= 2018 | volume= 34 | issue= 4 | pages= e75-e78 | pmid=28376069 | doi=10.1097/PEC.0000000000001134 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28376069 }} </ref><ref name="pmid29954742">{{cite journal| author=Khurshid S, Choi SH, Weng LC, Wang EY, Trinquart L, Benjamin EJ | display-authors=etal| title=Frequency of Cardiac Rhythm Abnormalities in a Half Million Adults. | journal=Circ Arrhythm Electrophysiol | year= 2018 | volume= 11 | issue= 7 | pages= e006273 | pmid=29954742 | doi=10.1161/CIRCEP.118.006273 | pmc=6051725 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29954742 }} </ref> A comprehensive list can be found in the table below. | |||
{| border="1" style="width:80%; height:100px" | |||
| bgcolor="LightSteelBlue" style="width:25%" ; border="1" |'''Cardiovascular''' | |||
| bgcolor="Beige" style="width:75%" ; border="1" |[[Air embolism]], [[amyloidosis]], [[aortic regurgitation]], [[aortic stenosis]], [[arteriovenous fistula]], [[Atrial infarction|atrial ischemia]], [[atrial myxoma]], [[atrial septal defect]], [[cardiac tamponade]], [[cardiac tumors]], [[cardiomyopathy]], [[The heart in Chagas' disease|Chagas heart disease]], [[congestive heart failure]], [[constrictive pericarditis]], [[coronary artery bypass graft surgery]], [[coronary artery disease]], [[dilated cardiomyopathy]], [[Ebstein's anomaly]], [[endocarditis]], [[familial atrial fibrillation]], [[familial atrioventricular nodal reentry tachycardia]], [[heart bypass surgery]], [[heart failure]], [[hemochromatosis]], [[holiday heart syndrome]], [[hypertensive heart disease]], [[hypertrophic cardiomyopathy]], [[hypokalemia]], [[hypotension]], [[hypoxia]], [[ischemic heart disease]], [[Kawasaki disease]], [[left ventricular hypertrophy]], [[Lown-Ganong-Levine syndrome]], [[Long QT Syndrome classification#LQT4|LQT type 4]], [[Lutembacher syndrome]], [[Mahaim fibers|mahaim fiber tachycardia]], [[mitral regurgitation]], [[mitral valve stenosis]], [[myocardial infarction]], [[myocarditis]], [[Coxsackie A virus#Diseases|neonatal coxsackie myocarditis]], [[open heart surgery]], [[pericarditis]], [[peripartum cardiomyopathy]], [[Cardiac surgery|post cardiac surgery]], [[pulmonary embolism]], [[pulmonary hypertension]], [[rheumatic heart disease]], [[shock]], [[sick sinus syndrome]], [[stroke]], [[temporary cardiac pacing]], [[tricuspid regurgitation]], [[tricuspid stenosis]], [[unstable angina]], [[uremic pericarditis]], [[valvular heart disease]], [[Wolff-Parkinson-White syndrome]] | |||
|- | |||
| bgcolor="LightSteelBlue" |'''Chemical/Poisoning''' | |||
| bgcolor="Beige" |[[Breath spray]], [[carbon monoxide poisoning]], [[cyanide]], [[grayanotoxin]], [[mercury poisoning]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Dental''' | |||
| bgcolor="Beige" |No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Dermatologic''' | |||
| bgcolor="Beige" |[[Psoriatic arthritis]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Drug Side Effect''' | |||
| bgcolor="Beige" |[[Albuterol]], [[alprazolam]], [[amiodarone]], [[amphetamines]], [[amrinone]], [[atomoxetine]], [[atropine]], [[beta blockers]], [[caffeine]], [[Carbamazepine#Adverse effects|carbamazepine poisoning]], [[cimetidine]], [[clonidine]], [[conivaptan]], [[diazoxide]], [[Cyanide poisoning#Treatment of poisoning and antidotes|dicobalt edetate]], [[diltiazem]], [[disopyramide]], [[dobutamine]], [[docetaxel]], [[dopexamine]], [[doxapram]], [[doxorubicin]], [[ephedrine]], [[epirubicin]], [[fentanyl]], [[flecainide]], [[flumazenil]], [[fluvoxamine]], [[guanethidine]], [[hexamethonium]], [[hydralazine]], [[ibutilide]], [[isoprenaline]], [[isoproterenol infusion]], [[lithium]], [[methamphetamines]], [[methyldopa]], [[methylphenidate]], [[methysergide]], [[minoxidil]], [[nelarabine]], [[nicotine]], [[orlistat]], [[palonosetron]], [[paroxetine]], [[phenoxybenzamine]], [[phentolamine]], [[porfimer sodium]], [[pramipexole]], [[procainamide]], [[propafenone]], [[quinidine]], [[ramucirumab]], [[reserpine]], [[ritodrine]], [[romidepsin]], [[salbutamol]], [[salmeterol]], [[sargramostim]], [[sibutramine]], [[theophylline]], [[trimethaphan]], [[Antiarrhythmic agent#Class Ia agents|type Ia antiarrhythmic agents]], [[Antiarrhythmic agent#Class Ic agents|type Ic antiarrhythmic agents]], [[Antiarrhythmic agent#Class III agents|type III antiarrhythmic agents]], [[verapamil]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Ear Nose Throat''' | |||
| bgcolor="Beige" |No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Endocrine''' | |||
| bgcolor="Beige" |[[Amyloidosis]], [[diabetes mellitus]], [[fatigue]], [[hemochromatosis]], [[hyperthyroidism]], [[hypoglycemia]], [[hypothyroidism]], [[pheochromocytoma]], [[thyrotoxicosis]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Environmental''' | |||
| bgcolor="Beige" |No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Gastroenterologic''' | |||
| bgcolor="Beige" |[[Crohn's disease]], [[hemochromatosis]], [[ulcerative colitis]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Genetic''' | |||
| bgcolor="Beige" |[[Channelopaties]], [[Emery-Dreifuss muscular dystrophy]], [[hemochromatosis]], [[Long QT Syndrome classification#LQT4|LQT type 4]], [[muscular dystrophy]], [[myotonic dystrophy]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Hematologic''' | |||
| bgcolor="Beige" |[[Anemia]], [[fat embolism]], [[fatigue]], [[hemochromatosis]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Iatrogenic''' | |||
| bgcolor="Beige" |[[Cardiac surgery]], [[cardiac transplantation]], [[Catheter ablation|incomplete ablation procedures]], [[Cardiac surgery|post cardiac surgery]], [[postoperative complication]], [[surgery]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Infectious Disease''' | |||
| bgcolor="Beige" |[[Amoebiasis]], [[The heart in Chagas' disease|chagas heart disease]], [[diphtheria]], [[fever]], [[leptospirosis]], [[Lyme disease]], [[myocarditis]], [[myotonic dystrophy]], [[Coxsackie A virus#Diseases|neonatal coxsackie myocarditis]], [[rheumatic fever]], [[Salmonella|salmonella typhosa]], [[sepsis]], [[trichinosis]], [[viral infections]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Musculoskeletal/Orthopedic''' | |||
| bgcolor="Beige" |[[Emery-Dreifuss muscular dystrophy]], [[fat embolism]], [[hemochromatosis]], [[muscular dystrophy]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Neurologic''' | |||
| bgcolor="Beige" |[[Diabetic neuropathy|Diabetic autonomic neuropathy]], [[fat embolism]], [[fatigue]], [[Guillain-Barré syndrome]], [[obstructive sleep apnea]], [[stroke]], [[subarachnoid hemorrhage]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Nutritional/Metabolic''' | |||
| bgcolor="Beige" |[[Dehydration]], [[hypercapnia]], [[hypervitaminosis D]], [[hypokalemia]], [[hypomagnesemia]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Obstetric/Gynecologic''' | |||
| bgcolor="Beige" |[[Hydrops fetalis|nonimmune hydrops fetalis]], [[peripartum cardiomyopathy]], [[pregnancy]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Oncologic''' | |||
| bgcolor="Beige" |[[atrial myxoma]], [[bronchogenic carcinoma]], [[cardiac tumors]], [[fatigue]], [[lung cancer]], [[pheochromocytoma]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Ophthalmologic''' | |||
| bgcolor="Beige" |No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Overdose/Toxicity''' | |||
| bgcolor="Beige" |[[Alcoholism|Alcohol overdose]], [[alcohol withdrawal]], [[Aminophylline|aminophylline toxicity]], [[binge drinking]], [[Carbamazepine#Adverse effects|carbamazepine poisoning]], [[Cocaine|cocaine overdose]], [[digitalis toxicity]], [[salicylate poisoning]], [[tricyclic antidepressant overdose]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Psychiatric''' | |||
| bgcolor="Beige" |[[Anxiety]], [[bulimia nervosa]], [[fatigue]], [[panic disorder]], [[psychological stress]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Pulmonary''' | |||
| bgcolor="Beige" |[[Air embolism]], [[bronchogenic carcinoma]], [[chronic obstructive pulmonary disease]], [[emphysema]], [[fat embolism]], [[hypoxia]], [[lung cancer]], [[pneumonia]], [[sarcoidosis]], [[tension pneumothorax]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Renal/Electrolyte''' | |||
| bgcolor="Beige" |[[Chronic kidney disease]], [[chronic renal failure]], [[dehydration]], [[electrolyte disturbance]], [[renal insufficiency]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Rheumatology/Immunology/Allergy''' | |||
| bgcolor="Beige" |[[Amyloidosis]], [[ankylosing spondylitis]], [[collagen vascular disease]], [[juvenile idiopathic arthritis]], [[psoriatic arthritis]], [[reactive arthritis]], [[rheumatic fever]], [[rheumatic heart disease]], [[sarcoidosis]], [[scleroderma]], [[spondyloarthritis]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Sexual''' | |||
| bgcolor="Beige" |No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Trauma''' | |||
| bgcolor="Beige" |[[Commotio cordis|Cardiac injury from blunt trauma]], [[drowning]], [[electric shock]] | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Urologic''' | |||
| bgcolor="Beige" |No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
|'''Miscellaneous''' | |||
| bgcolor="Beige" |[[Binge drinking]], [[drowning]], [[fever]], [[hypothermia]], [[malignant hyperthermia]], [[pain]], [[stress]] | |||
|- | |||
|} | |||
==Differentiating Among the Different Types of Supraventricular Tachycardia== | |||
The individual subtypes of SVT can be distinguished from each other by certain physiological and electrical characteristics, many of which present in the patient's EKG. [[Supraventricular tachycardias]] must be differentiated from each other because the management strategies may vary<ref name="pmid28838545">{{cite journal| author=Padeletti L, Bagliani G| title=General Introduction, Classification, and Electrocardiographic Diagnosis of Cardiac Arrhythmias. | journal=Card Electrophysiol Clin | year= 2017 | volume= 9 | issue= 3 | pages= 345-363 | pmid=28838545 | doi=10.1016/j.ccep.2017.05.009 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28838545 }} </ref>. | |||
{| class="wikitable" | |||
|+ | |||
! | |||
!Epidemiology | |||
!Rate | |||
!Rhythm | |||
!P waves | |||
!PR Interval | |||
!QRS complex | |||
!Response to maneuvers | |||
|- | |||
|'''Sinus Tachycardia''' | |||
|More common in children and elderly. | |||
|Greater than 100 bpm | |||
|Regular | |||
|Upright, consistent, and normal in morphology | |||
|0.12–0.20 sec and shortens with high heart rate | |||
|Less than 0.12 seconds, consistent, and normal in morphology | |||
|May break with [[vagal maneuvers]] | |||
|- | |||
|'''Atrial Fibrillation''' | |||
|More common in the elderly, following [[bypass surgery]], in mitral valve disease, [[hyperthyroidism]] | |||
|110 to 180 bpm | |||
|Irregularly irregular | |||
|Absent, fibrillatory waves | |||
|Absent | |||
|Less than 0.12 seconds, consistent, and normal in morphology in the absence of aberrant conduction | |||
|Does not break with [[adenosine]] or [[vagal maneuvers]] | |||
|- | |||
|'''Atrial Flutter''' | |||
|More common in the elderly, after alcohol | |||
|75 (4:1 block), 100 (3:1 block) and 150 (2:1 block) bpm, but 150 is more common | |||
|Regular | |||
|Sawtooth pattern of [[P waves]] at 250 to 350 beats per minute | |||
|Varies depending upon the magnitude of the block, but is short | |||
|Less than 0.12 seconds, consistent, and normal in morphology | |||
|Conduction may vary in response to drugs and maneuvers dropping the rate from 150 to 100 or to 75 bpm | |||
|- | |||
|'''AV Nodal Reentry Tachycardia (AVNRT)''' | |||
|Accounts for 60%-70% of all SVTs. 80% to 90% of cases are due to antegrade conduction down a slow pathway and retrograde up a fast pathway. | |||
|In adults the range is 140-250 bpm, but in children the rate can exceed 250 bpm | |||
|Regular | |||
|The [[P wave]] is usually superimposed on or buried within the [[QRS complex]] | |||
|Cannot be calculated as the P wave is generally obscured by the [[QRS complex]] | |||
|Less than 0.12 seconds, consistent, and normal in morphology | |||
|May break with [[adenosine]] or [[vagal maneuvers]] | |||
|- | |||
|'''AV Reciprocating Tachycardia (AVRT)''' | |||
|More common in males, whereas [[AV nodal reentrant tachycardia|AVNRT]] is more common in females, occurs at a younger age. | |||
|More rapid than [[AV nodal reentrant tachycardia|AVNRT]] | |||
|Regular | |||
|A [[retrograde P wave]] is seen either at the end of the [[QRS complex]] or at the beginning of the ST segment | |||
|Less than 0.12 seconds | |||
|Less than 0.12 seconds, consistent, and normal in morphology | |||
|May break with [[adenosine]] or [[vagal maneuvers]] | |||
|- | |||
|'''Inappropriate Sinus Tachycardia''' | |||
|The disorder is uncommon. Most patients are in their late 20s to early 30s. More common in women. | |||
|> 95 beats per minute. A nocturnal reduction in heart rate is present. There is an inappropriate heart rate response on exertion. | |||
|Regular | |||
|Normal morphology and precede the [[QRS complex]] | |||
|Normal and < 0.20 seconds | |||
|Less than 0.12 seconds, consistent, and normal in morphology | |||
|Does not break with [[adenosine]] or [[vagal maneuvers]] | |||
|- | |||
|'''Junctional Tachycardia''' | |||
|Common after [[heart surgery]], [[digitalis toxicity]], as an escape rhythm in [[AV block]] | |||
|> 60 beats per minute | |||
|Regular | |||
|Usually inverted, may be burried in the [[QRS complex]] | |||
|The [[P wave]] is usually buried in the [[QRS complex]] | |||
|Less than 0.12 seconds, consistent, and normal in morphology | |||
|Does not break with [[adenosine]] or [[vagal maneuvers]] | |||
|- | |||
|'''Multifocal Atrial Tachycardia (MAT)''' | |||
|High incidence in the elderly and in those with [[COPD]] | |||
|Atrial rate is > 100 beats per minute (bpm) | |||
|Irregular | |||
|P waves of varying morphology from at least three different foci | |||
|Variable [[PR interval]]s, [[RR interval]]s, and [[PP interval]]s | |||
|Less than 0.12 seconds, consistent, and normal in morphology | |||
|Does not terminate with [[adenosine]] or [[vagal maneuvers]] | |||
|- | |||
|'''Sinus Node Reentry Tachycardia''' | |||
|Between 2% and 17% among individuals undergoing [[EKG]] for SVTs | |||
|100 to 150 bpm | |||
|Regular | |||
|Upright [[P waves]] precede each regular, narrow [[QRS]] complex | |||
|[[Short PR interval]] | |||
|Less than 0.12 seconds, consistent, and normal in morphology | |||
|Does often terminate with [[vagal maneuvers]] unlike [[sinus tachycardia]]. | |||
|- | |||
|'''Wolff-Parkinson-White syndrome''' | |||
|Estimated prevalence of [[Wolff-Parkinson-White syndrome|WPW]] syndrome is 100 - 300 per 100,000 in the entire world. | |||
|Atrial rate is nearly 300 bpm and ventricular rate is at 150 bpm. | |||
|Regular | |||
|[[P wave]] generally follows the [[QRS]] complex due to a bypass tract | |||
|Less than 0.12 seconds | |||
|[[Delta wave]] and evidence of ventricular [[pre-excitation]] if there is conduction to the ventricle via ante-grade conduction down an [[accessory pathway]] | |||
|May break in response to [[procainamide]], [[adenosine]], [[vagal maneuvers]] | |||
|} | |||
==Differentiating Supraventricular Tachycardia from Ventricular Tachycardia== | |||
For a detailed discussion of how to distinguish [[ventricular tachycardia]] ([[VT]]) from [[supraventricular tachycardia]] ([[SVT]]), please visit the [[wide complex tachycardia differential diagnosis]] page. | |||
In brief, the diagnosis of [[VT]] is more likely if: | |||
* There is a history of [[myocardial infarction]], [[congestive heart failure]] or [[structural heart disease]] | |||
* [[VT]] is more common in the elderly | |||
* The [[electrical axis]] is -90 to -180 degrees (a “northwest” or “superior” axis) | |||
* The [[QRS]] is > 140 msec | |||
* There is [[AV dissociation]]. [[P waves]] are normal in morphology, upright, but dissociated from the QRS complex (i.e. "march through" the [[QRS complex]]) | |||
* There are positive or negative [[QRS]] complexes in all the precordial leads | |||
* The morphology of the [[QRS]] complexes resembles that of a previous [[premature ventricular contraction]] ([[PVC]]). | |||
* Rate: More than 100 bpm and usually 150-200 bpm | |||
* Rhythm: The rhythm is regular | |||
* [[PR interval]]: Variable PR interval | |||
* Response to Maneuvers: VT does not terminate in response to [[adenosine]] or [[vagal maneuvers]] | |||
== Diagnosis == | |||
=== | === Symptoms === | ||
Symptoms that are common to all types of SVT include the following<ref name="pmid31378331">{{cite journal| author=Mahtani AU, Nair DG| title=Supraventricular Tachycardia. | journal=Med Clin North Am | year= 2019 | volume= 103 | issue= 5 | pages= 863-879 | pmid=31378331 | doi=10.1016/j.mcna.2019.05.007 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31378331 }} </ref>: | |||
* [[Anxiety]] | |||
* [[Chest pain]] or sensation of tightness | |||
* [[Dizziness]], or [[lightheadedness]] (near-faint), or [[fainting]] | |||
* [[Lightheadedness]] | |||
* [[Palpitation|Palpitations]] (the sensation of the heart racing, fluttering or pounding strongly in the chest or the [[carotid arteries]]) | |||
* [[Shortness of breath]] | |||
* [[Syncope]] in cases of [[AVNRT]] | |||
* [[Sweating]] | |||
=== Electrocardiogram === | |||
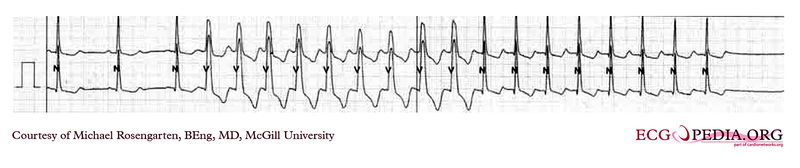
Shown below is an [[The electrocardiogram|EKG]] depicting a [[tachycardia]] at a rate of 190/min with narrow [[QRS complexes]] indicating [[supraventricular tachycardia]].[[Image:SVT.jpg|center|500px|link=https://www.wikidoc.org/index.php/File:SVT.jpg|Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/File:De-AW00011.jpg ]]Shown below is an EKG recording of a patient who goes from sinus rhythm to a [[wide complex tachycardia]] at about 130/min. | |||
* The [[wide QRS]] though disappears after nine complexes and is replaced by narrow complexes at a slightly slower rate. | |||
* No [[P wave]] activity is seen. | |||
* This is a [[supraventricular tachycardia]] with a form of aberrancy. | |||
* In this case, we are probably seeing a rate-dependent [[left bundle branch block]] or the effect of a [[left bundle branch block]] which persists for the nine complexes because of continued block in the left bundle from the depolarizations from the intact right bundle. | |||
[[Image: Supraventricular tachycardia.jpg|center|500px|link=https://www.wikidoc.org/index.php/File:Supraventricular_tachycardia.jpg|Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page]] | |||
== Treatment == | |||
===Acute Treatment=== | |||
== | * In general, [[SVT]] is not life threatening, but episodes should be treated or prevented. While some treatment modalities can be applied to all SVTs with impunity, there are specific therapies available to cure some of the different sub-types<ref name="pmid23050527">{{cite journal| author=Link MS| title=Clinical practice. Evaluation and initial treatment of supraventricular tachycardia. | journal=N Engl J Med | year= 2012 | volume= 367 | issue= 15 | pages= 1438-48 | pmid=23050527 | doi=10.1056/NEJMcp1111259 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23050527 }} </ref>. | ||
* Cure requires intimate knowledge of how and where the [[arrhythmia]] is initiated and propagated. | |||
* The SVTs can be separated into two groups, based on whether they involve the [[Atrioventricular node|AV node]] for impulse maintenance or not. | |||
* Those that involve the [[AV node]] can be terminated by slowing conduction through the [[Atrioventricular node|AV node]]. | |||
* Those that do not involve the [[Atrioventricular node|AV node]] will not usually be stopped by AV nodal blocking maneuvers. | |||
* These maneuvers are still useful however, as transient [[AV block]] will often unmask the underlying rhythm abnormality<ref name="pmid28290912">{{cite journal| author=Mironov NY, Golitsyn SP| title=[Overwiew of New Clinical Guidelines for the Diagnosis and Treatment of Supraventricular Tachycardias (2015) of the American College of Cardiology/American Heart Association/Society for Heart Rhythm Disturbances (ACC/AHA/HRS)]. | journal=Kardiologiia | year= 2016 | volume= 56 | issue= 7 | pages= 84-90 | pmid=28290912 | doi=10.18565/cardio.2016.7.84-90 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28290912 }} </ref>. | |||
====Acute Pharmacotherapy==== | |||
* Another modality involves treatment with medications<ref name="pmid27484659">{{cite journal| author=Al-Zaiti SS, Magdic KS| title=Paroxysmal Supraventricular Tachycardia: Pathophysiology, Diagnosis, and Management. | journal=Crit Care Nurs Clin North Am | year= 2016 | volume= 28 | issue= 3 | pages= 309-16 | pmid=27484659 | doi=10.1016/j.cnc.2016.04.005 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27484659 }} </ref>. | |||
* Pre-hospital care providers and hospital clinicians might administer [[adenosine]], an ultra short acting AV nodal blocking agent. | |||
* If this works, follow-up therapy with [[diltiazem]], [[verapamil]] or [[metoprolol]] may be indicated. | |||
* SVT that does NOT involve the AV node may respond to other anti-arrhythmic drugs such as [[sotalol]] or [[amiodarone]]. | |||
* In [[pregnancy]], [[metoprolol]] is the treatment of choice as recommended by the [[American Heart Association]]<ref name="pmid28290912">{{cite journal| author=Mironov NY, Golitsyn SP| title=[Overwiew of New Clinical Guidelines for the Diagnosis and Treatment of Supraventricular Tachycardias (2015) of the American College of Cardiology/American Heart Association/Society for Heart Rhythm Disturbances (ACC/AHA/HRS)]. | journal=Kardiologiia | year= 2016 | volume= 56 | issue= 7 | pages= 84-90 | pmid=28290912 | doi=10.18565/cardio.2016.7.84-90 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28290912 }} </ref>. | |||
==Prevention== | |||
* Once the acute episode has been terminated, ongoing treatment may be indicated to prevent a recurrence of the [[Cardiac arrhythmia|arrhythmia]]<ref name="pmid3644291">{{cite journal| author=Ordonez RV| title=Monitoring the patient with supraventricular dysrhythmias. | journal=Nurs Clin North Am | year= 1987 | volume= 22 | issue= 1 | pages= 49-59 | pmid=3644291 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3644291 }} </ref>. | |||
* Patients who have a single isolated episode, or infrequent and minimally symptomatic episodes usually do not warrant any treatment except observation. | |||
== | * Patients who have more frequent or disabling symptoms from their episodes generally warrant some form of preventative therapy. | ||
* | * A variety of drugs including simple AV nodal blocking agents like [[Beta-blocker|beta-blockers]] and [[verapamil]], as well as [[antiarrhythmics]] may be used, usually with good effect, although the risks of these therapies need to be weighed against the potential benefits<ref name="pmid28030653">{{cite journal| author=Al-Khatib SM, Page RL| title=Ongoing Management of Patients With Supraventricular Tachycardia. | journal=JAMA Cardiol | year= 2017 | volume= 2 | issue= 3 | pages= 332-333 | pmid=28030653 | doi=10.1001/jamacardio.2016.5085 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28030653 }} </ref>. | ||
* | |||
==References== | ==References== | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
<references /> | |||
Latest revision as of 16:18, 17 February 2020
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Abdelrahman Ibrahim Abushouk, MD[2]
Synonyms and keywords: SVT
Overview
There are several classification systems for supraventricular tachycardia, based on site of origin, QRS width, pulse regularity, and AV node dependence. There are different types of supraventricular tachycardia, including sinus tachycardia, inappropriate sinus tachycardia, sinus node re-entry tachycardia, atrial fibrillation, atrial flutter, AV nodal re-entry tachycardia, AV reciprocating tachycardia, junctional tachycardia, multifocal atrial tachycardia, and Wolff-Parkinson White syndrome. The general symptoms of SVTs include anxiety, chest pain or sensation of tightness, dizziness or fainting, palpitations, shortness of breath, syncope in cases of AVNRT, and sweating. The individual subtypes of SVT can be distinguished from each other by certain physiological and electrical characteristics, many of which present in the patient's EKG. Supraventricular tachycardias must be differentiated from each other because the management strategies may vary. In general, SVT is not life threatening, but episodes should be treated or prevented. While some treatment modalities can be applied to all SVTs with impunity, there are specific therapies available to cure some of the different sub-types. Cure requires intimate knowledge of how and where the arrhythmia is initiated and propagated. SVTs can be separated into two groups, based on whether they involve the AV node for impulse maintenance or not. Those that involve the AV node can be terminated by slowing conduction through the AV node. Those that do not involve the AV node will not usually be stopped by AV nodal blocking maneuvers. These maneuvers are still useful however, as transient AV block will often unmask the underlying rhythm abnormality. Once the acute episode has been terminated, ongoing treatment may be indicated to prevent a recurrence of the arrhythmia. Patients who have a single isolated episode, or infrequent and minimally symptomatic episodes usually do not warrant any treatment except observation. Patients who have more frequent or disabling symptoms from their episodes generally warrant some form of preventative therapy. A variety of drugs including simple AV nodal blocking agents like beta-blockers and verapamil, as well as antiarrhythmics may be used, usually with good effect, although the risks of these therapies need to be weighed against the potential benefits.
Classification
There are several classification systems for supraventricular tachycardia, based on site of origin, QRS width, pulse regularity, and AV node dependence.[1][2]
- Supraventricular tachycardia can be classified based on the site of origin into:
- Physiological sinus tachycardia
- Atrial tachycardia
- Atrioventricular tachycardia
- Supraventricular tachycardia can be classified based on QRS width into:
- Narrow complex tachycardia: Sinus tachycardia, atrial flutter, atrial fibrillation, focal/multifocal atrial tachycardia, Sinus node re-entry, AVNRT, and junctional tachycardia.
- Wide complex tachycardia: AF with aberrations and AF with WPW.
- Supraventricular tachycardia can be classified based on pulse regularity into:
- Regular: Sinus tachycardia, atrial flutter, Sinus node re-entry tachycardia, AVNRT, and junctional tachycardia.
- Irregular: Atrial fibrillation and multifocal atrial tachycardia
- Supraventricular tachycardia can be classified based on AV node dependence into:
- AV node dependent: AVNRTs and AVRTs
- AV node independent: Focal atrial tachycardia and atrial flutter
Causes
Causes by Organ System
There are several causes of supraventricular tachycardia in almost all body systems.[3][4] A comprehensive list can be found in the table below.
Differentiating Among the Different Types of Supraventricular Tachycardia
The individual subtypes of SVT can be distinguished from each other by certain physiological and electrical characteristics, many of which present in the patient's EKG. Supraventricular tachycardias must be differentiated from each other because the management strategies may vary[5].
| Epidemiology | Rate | Rhythm | P waves | PR Interval | QRS complex | Response to maneuvers | |
|---|---|---|---|---|---|---|---|
| Sinus Tachycardia | More common in children and elderly. | Greater than 100 bpm | Regular | Upright, consistent, and normal in morphology | 0.12–0.20 sec and shortens with high heart rate | Less than 0.12 seconds, consistent, and normal in morphology | May break with vagal maneuvers |
| Atrial Fibrillation | More common in the elderly, following bypass surgery, in mitral valve disease, hyperthyroidism | 110 to 180 bpm | Irregularly irregular | Absent, fibrillatory waves | Absent | Less than 0.12 seconds, consistent, and normal in morphology in the absence of aberrant conduction | Does not break with adenosine or vagal maneuvers |
| Atrial Flutter | More common in the elderly, after alcohol | 75 (4:1 block), 100 (3:1 block) and 150 (2:1 block) bpm, but 150 is more common | Regular | Sawtooth pattern of P waves at 250 to 350 beats per minute | Varies depending upon the magnitude of the block, but is short | Less than 0.12 seconds, consistent, and normal in morphology | Conduction may vary in response to drugs and maneuvers dropping the rate from 150 to 100 or to 75 bpm |
| AV Nodal Reentry Tachycardia (AVNRT) | Accounts for 60%-70% of all SVTs. 80% to 90% of cases are due to antegrade conduction down a slow pathway and retrograde up a fast pathway. | In adults the range is 140-250 bpm, but in children the rate can exceed 250 bpm | Regular | The P wave is usually superimposed on or buried within the QRS complex | Cannot be calculated as the P wave is generally obscured by the QRS complex | Less than 0.12 seconds, consistent, and normal in morphology | May break with adenosine or vagal maneuvers |
| AV Reciprocating Tachycardia (AVRT) | More common in males, whereas AVNRT is more common in females, occurs at a younger age. | More rapid than AVNRT | Regular | A retrograde P wave is seen either at the end of the QRS complex or at the beginning of the ST segment | Less than 0.12 seconds | Less than 0.12 seconds, consistent, and normal in morphology | May break with adenosine or vagal maneuvers |
| Inappropriate Sinus Tachycardia | The disorder is uncommon. Most patients are in their late 20s to early 30s. More common in women. | > 95 beats per minute. A nocturnal reduction in heart rate is present. There is an inappropriate heart rate response on exertion. | Regular | Normal morphology and precede the QRS complex | Normal and < 0.20 seconds | Less than 0.12 seconds, consistent, and normal in morphology | Does not break with adenosine or vagal maneuvers |
| Junctional Tachycardia | Common after heart surgery, digitalis toxicity, as an escape rhythm in AV block | > 60 beats per minute | Regular | Usually inverted, may be burried in the QRS complex | The P wave is usually buried in the QRS complex | Less than 0.12 seconds, consistent, and normal in morphology | Does not break with adenosine or vagal maneuvers |
| Multifocal Atrial Tachycardia (MAT) | High incidence in the elderly and in those with COPD | Atrial rate is > 100 beats per minute (bpm) | Irregular | P waves of varying morphology from at least three different foci | Variable PR intervals, RR intervals, and PP intervals | Less than 0.12 seconds, consistent, and normal in morphology | Does not terminate with adenosine or vagal maneuvers |
| Sinus Node Reentry Tachycardia | Between 2% and 17% among individuals undergoing EKG for SVTs | 100 to 150 bpm | Regular | Upright P waves precede each regular, narrow QRS complex | Short PR interval | Less than 0.12 seconds, consistent, and normal in morphology | Does often terminate with vagal maneuvers unlike sinus tachycardia. |
| Wolff-Parkinson-White syndrome | Estimated prevalence of WPW syndrome is 100 - 300 per 100,000 in the entire world. | Atrial rate is nearly 300 bpm and ventricular rate is at 150 bpm. | Regular | P wave generally follows the QRS complex due to a bypass tract | Less than 0.12 seconds | Delta wave and evidence of ventricular pre-excitation if there is conduction to the ventricle via ante-grade conduction down an accessory pathway | May break in response to procainamide, adenosine, vagal maneuvers |
Differentiating Supraventricular Tachycardia from Ventricular Tachycardia
For a detailed discussion of how to distinguish ventricular tachycardia (VT) from supraventricular tachycardia (SVT), please visit the wide complex tachycardia differential diagnosis page.
In brief, the diagnosis of VT is more likely if:
- There is a history of myocardial infarction, congestive heart failure or structural heart disease
- VT is more common in the elderly
- The electrical axis is -90 to -180 degrees (a “northwest” or “superior” axis)
- The QRS is > 140 msec
- There is AV dissociation. P waves are normal in morphology, upright, but dissociated from the QRS complex (i.e. "march through" the QRS complex)
- There are positive or negative QRS complexes in all the precordial leads
- The morphology of the QRS complexes resembles that of a previous premature ventricular contraction (PVC).
- Rate: More than 100 bpm and usually 150-200 bpm
- Rhythm: The rhythm is regular
- PR interval: Variable PR interval
- Response to Maneuvers: VT does not terminate in response to adenosine or vagal maneuvers
Diagnosis
Symptoms
Symptoms that are common to all types of SVT include the following[6]:
- Anxiety
- Chest pain or sensation of tightness
- Dizziness, or lightheadedness (near-faint), or fainting
- Lightheadedness
- Palpitations (the sensation of the heart racing, fluttering or pounding strongly in the chest or the carotid arteries)
- Shortness of breath
- Syncope in cases of AVNRT
- Sweating
Electrocardiogram
Shown below is an EKG depicting a tachycardia at a rate of 190/min with narrow QRS complexes indicating supraventricular tachycardia.
- The wide QRS though disappears after nine complexes and is replaced by narrow complexes at a slightly slower rate.
- No P wave activity is seen.
- This is a supraventricular tachycardia with a form of aberrancy.
- In this case, we are probably seeing a rate-dependent left bundle branch block or the effect of a left bundle branch block which persists for the nine complexes because of continued block in the left bundle from the depolarizations from the intact right bundle.
Treatment
Acute Treatment
- In general, SVT is not life threatening, but episodes should be treated or prevented. While some treatment modalities can be applied to all SVTs with impunity, there are specific therapies available to cure some of the different sub-types[7].
- Cure requires intimate knowledge of how and where the arrhythmia is initiated and propagated.
- The SVTs can be separated into two groups, based on whether they involve the AV node for impulse maintenance or not.
- Those that involve the AV node can be terminated by slowing conduction through the AV node.
- Those that do not involve the AV node will not usually be stopped by AV nodal blocking maneuvers.
- These maneuvers are still useful however, as transient AV block will often unmask the underlying rhythm abnormality[8].
Acute Pharmacotherapy
- Another modality involves treatment with medications[9].
- Pre-hospital care providers and hospital clinicians might administer adenosine, an ultra short acting AV nodal blocking agent.
- If this works, follow-up therapy with diltiazem, verapamil or metoprolol may be indicated.
- SVT that does NOT involve the AV node may respond to other anti-arrhythmic drugs such as sotalol or amiodarone.
- In pregnancy, metoprolol is the treatment of choice as recommended by the American Heart Association[8].
Prevention
- Once the acute episode has been terminated, ongoing treatment may be indicated to prevent a recurrence of the arrhythmia[10].
- Patients who have a single isolated episode, or infrequent and minimally symptomatic episodes usually do not warrant any treatment except observation.
- Patients who have more frequent or disabling symptoms from their episodes generally warrant some form of preventative therapy.
- A variety of drugs including simple AV nodal blocking agents like beta-blockers and verapamil, as well as antiarrhythmics may be used, usually with good effect, although the risks of these therapies need to be weighed against the potential benefits[11].
References
- ↑ Lundqvist CB, Potpara TS, Malmborg H (2017). "Supraventricular Arrhythmias in Patients with Adult Congenital Heart Disease". Arrhythm Electrophysiol Rev. 6 (2): 42–49. doi:10.15420/aer.2016:29:3. PMC 5517371. PMID 28835834.
- ↑ Massari F, Scicchitano P, Potenza A, Sassara M, Sanasi M, Liccese M; et al. (2018). "Supraventricular tachycardia, pregnancy, and water: A new insight in lifesaving treatment of rhythm disorders". Ann Noninvasive Electrocardiol. 23 (3): e12490. doi:10.1111/anec.12490. PMID 28833859.
- ↑ Corwin DJ, Scarfone RJ (2018). "Supraventricular Tachycardia Associated With Severe Anemia". Pediatr Emerg Care. 34 (4): e75–e78. doi:10.1097/PEC.0000000000001134. PMID 28376069.
- ↑ Khurshid S, Choi SH, Weng LC, Wang EY, Trinquart L, Benjamin EJ; et al. (2018). "Frequency of Cardiac Rhythm Abnormalities in a Half Million Adults". Circ Arrhythm Electrophysiol. 11 (7): e006273. doi:10.1161/CIRCEP.118.006273. PMC 6051725. PMID 29954742.
- ↑ Padeletti L, Bagliani G (2017). "General Introduction, Classification, and Electrocardiographic Diagnosis of Cardiac Arrhythmias". Card Electrophysiol Clin. 9 (3): 345–363. doi:10.1016/j.ccep.2017.05.009. PMID 28838545.
- ↑ Mahtani AU, Nair DG (2019). "Supraventricular Tachycardia". Med Clin North Am. 103 (5): 863–879. doi:10.1016/j.mcna.2019.05.007. PMID 31378331.
- ↑ Link MS (2012). "Clinical practice. Evaluation and initial treatment of supraventricular tachycardia". N Engl J Med. 367 (15): 1438–48. doi:10.1056/NEJMcp1111259. PMID 23050527.
- ↑ 8.0 8.1 Mironov NY, Golitsyn SP (2016). "[Overwiew of New Clinical Guidelines for the Diagnosis and Treatment of Supraventricular Tachycardias (2015) of the American College of Cardiology/American Heart Association/Society for Heart Rhythm Disturbances (ACC/AHA/HRS)]". Kardiologiia. 56 (7): 84–90. doi:10.18565/cardio.2016.7.84-90. PMID 28290912.
- ↑ Al-Zaiti SS, Magdic KS (2016). "Paroxysmal Supraventricular Tachycardia: Pathophysiology, Diagnosis, and Management". Crit Care Nurs Clin North Am. 28 (3): 309–16. doi:10.1016/j.cnc.2016.04.005. PMID 27484659.
- ↑ Ordonez RV (1987). "Monitoring the patient with supraventricular dysrhythmias". Nurs Clin North Am. 22 (1): 49–59. PMID 3644291.
- ↑ Al-Khatib SM, Page RL (2017). "Ongoing Management of Patients With Supraventricular Tachycardia". JAMA Cardiol. 2 (3): 332–333. doi:10.1001/jamacardio.2016.5085. PMID 28030653.