Squamous cell carcinoma of the skin pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
{{CMG}}; '''Associate Editor(s)-in-Chief:''' [[User:Aditya Govindavarjhulla|Aditya Govindavarjhulla, M.B.B.S.]] [mailto:agovi@wikidoc.org], [[User:Raviteja Reddy Guddeti|Raviteja Guddeti, M.B.B.S.]] [mailto:ravitheja.g@gmail.com] | {{CMG}}; '''Associate Editor(s)-in-Chief:''' [[User:Aditya Govindavarjhulla|Aditya Govindavarjhulla, M.B.B.S.]] [mailto:agovi@wikidoc.org], [[User:Raviteja Reddy Guddeti|Raviteja Guddeti, M.B.B.S.]] [mailto:ravitheja.g@gmail.com] | ||
== Overview == | == Overview == | ||
[[Squamous cell carcinoma]] (SCC) is type of non-[[melanoma]] [[skin cancer]]. The [[Cancer (medicine)|cancer]] arises as a result of uncontrolled [[growth]] of the [[Squamous cell|squamous cells]] in the [[epidermis]] of the [[Skin Changes|skin]]. Unlike it's counter part, the [[basal cell carcinoma]] which also belongs to the group of non-[[melanoma]] [[cancer]], [[squamous cell carcinoma]] is rapid growing and invasive. [[Squamous cell carcinoma|SCCs]] may occur on all areas of the [[body]] including the [[mucous membranes]] and [[genitals]], but are most common in areas frequently exposed to the [[Sun exposure|sun]], such as the rim of the [[ear]], [[Lip|lower lip]], [[face]], [[ | [[Squamous cell carcinoma]] (SCC) is type of non-[[melanoma]] [[skin cancer]]. The [[Cancer (medicine)|cancer]] arises as a result of uncontrolled [[growth]] of the [[Squamous cell|squamous cells]] in the [[epidermis]] of the [[Skin Changes|skin]]. Unlike it's counter part, the [[basal cell carcinoma]] which also belongs to the group of non-[[melanoma]] [[cancer]], [[squamous cell carcinoma]] is rapid growing and [[invasive]]. [[Squamous cell carcinoma|SCCs]] may occur on all areas of the [[body]] including the [[mucous membranes]] and [[genitals]], but are most common in areas frequently exposed to the [[Sun exposure|sun]], such as the rim of the [[ear]], [[Lip|lower lip]], [[face]], bald [[scalp]], [[neck]], [[hands]], [[Arm|arms]] and [[Leg|legs]]. Wrinkling, changes in [[pigmentation]], and loss of [[Elastic|elasticity]] of the [[skin]] are often the telltale [[signs]] of [[Sun exposure|sun]] damage. | ||
== Pathophysiology == | == Pathophysiology == | ||
*<nowiki/>[[p53]] is mutated commonly in | *<nowiki/>[[p53]] is mutated commonly in [[Actinic keratosis]], demonstrating that [[Dysplastic change|dysplastic]] lesions have acquired the initial [[Genetic mutations|ge]]<nowiki/>[[Genetic mutations|netic mutation]]<nowiki/>s prior to becoming [[cutaneous squamous cell carcinoma]].<ref name="pmid11966728">{{cite journal |vauthors=Ortonne JP |title=From actinic keratosis to squamous cell carcinoma |journal=Br. J. Dermatol. |volume=146 Suppl 61 |issue= |pages=20–3 |date=April 2002 |pmid=11966728 |doi= |url=}}</ref> | ||
* The mechanism leading to genomic instability in [[keratinocytes]] likely results from UVB-induced inactivation of [[P53 gene|p5]]<nowiki/>[[P53 gene|3]], since approximately 58% of [[cutaneous squamous cell carcinoma]] harbor [[UVB]] signature [[mutations]] such as CC→TT and C→T transitions.<ref name="pmid52880">{{cite journal |vauthors=Borelli D, Salas J |title=[The use of trypan blue instead of cotton blue in mycology] |language=Spanish; Castilian |journal=Rev. Latinoam. Microbiol. |volume=17 |issue=3 |pages=185–6 |date=1975 |pmid=52880 |doi= |url=}}</ref> | * The mechanism leading to genomic instability in [[keratinocytes]] likely results from [[UVB radiation|UVB-induced]] inactivation of [[P53 gene|p5]]<nowiki/>[[P53 gene|3]], since approximately 58% of [[cutaneous squamous cell carcinoma]] harbor [[UVB]] signature [[mutations]] such as CC→TT and C→T transitions.<ref name="pmid52880">{{cite journal |vauthors=Borelli D, Salas J |title=[The use of trypan blue instead of cotton blue in mycology] |language=Spanish; Castilian |journal=Rev. Latinoam. Microbiol. |volume=17 |issue=3 |pages=185–6 |date=1975 |pmid=52880 |doi= |url=}}</ref> | ||
* Aberrant activation of [[EGFR]] and [[Fyn-related kinase|Fyn]], a Src-family tyrosine kinase (SFK), are seen in [[human]] [[cutaneous squamous cell carcinoma]]. | * Aberrant activation of [[EGFR]] and [[Fyn-related kinase|Fyn]], a Src-family tyrosine kinase (SFK), are seen in [[human]] [[cutaneous squamous cell carcinoma]]. | ||
* [[Kinases]] downregulate [[p53]] mRNA and protein levels through a [[C-Jun|c-Jun–dependent mechanism]] (28, 29), revealing another mechanism for controlling [[P53 gene|p53]] function<ref name="pmid2747621">{{cite journal |vauthors=Strabala TJ, Bednarek SY, Bertoni G, Amasino RM |title=Isolation and characterization of an ipt gene from the Ti plasmid Bo542 |journal=Mol. Gen. Genet. |volume=216 |issue=2-3 |pages=388–94 |date=April 1989 |pmid=2747621 |doi= |url=}}</ref> | * [[Kinases]] downregulate [[p53]] [[mRNA]] and [[protein]] levels through a [[C-Jun|c-Jun–dependent mechanism]] (28, 29), revealing another mechanism for controlling [[P53 gene|p53]] function<ref name="pmid2747621">{{cite journal |vauthors=Strabala TJ, Bednarek SY, Bertoni G, Amasino RM |title=Isolation and characterization of an ipt gene from the Ti plasmid Bo542 |journal=Mol. Gen. Genet. |volume=216 |issue=2-3 |pages=388–94 |date=April 1989 |pmid=2747621 |doi= |url=}}</ref> | ||
* Amplification and activating mutations of the [[Ras oncogene]] have been found in | * Amplification and activating [[mutations]] of the [[Ras oncogene]] have been found in [[squamous cell carcinoma]] and [[Actinic keratosis|Actnic keratosis]] | ||
* [[Ras gene|Ras]] is an upstream activator of the Raf/Mek/Erk1/Erk2 kinase pathway, and activating [[mutations]] in [[Ras gene|Ras]] can promote [[cutaneous squamous cell carcinoma]]. formation. <ref name="pmid7611795">{{cite journal |vauthors=Spencer JM, Kahn SM, Jiang W, DeLeo VA, Weinstein IB |title=Activated ras genes occur in human actinic keratoses, premalignant precursors to squamous cell carcinomas |journal=Arch Dermatol |volume=131 |issue=7 |pages=796–800 |date=July 1995 |pmid=7611795 |doi= |url=}}</ref> | * [[Ras gene|Ras]] is an upstream activator of the Raf/Mek/Erk1/Erk2 [[kinase pathway]], and activating [[mutations]] in [[Ras gene|Ras]] can promote [[cutaneous squamous cell carcinoma]]. formation. <ref name="pmid7611795">{{cite journal |vauthors=Spencer JM, Kahn SM, Jiang W, DeLeo VA, Weinstein IB |title=Activated ras genes occur in human actinic keratoses, premalignant precursors to squamous cell carcinomas |journal=Arch Dermatol |volume=131 |issue=7 |pages=796–800 |date=July 1995 |pmid=7611795 |doi= |url=}}</ref> | ||
* Expression of β1-[[integrins]] and their [[ligands]] correlates with [[Tumor cell|tumor]] progression in human [[skin]]. | * Expression of β1-[[integrins]] and their [[ligands]] correlates with [[Tumor cell|tumor]] progression in [[human]] [[skin]]. | ||
* [[Ras gene|Ras]] family members of [[Proto-oncogene|proto-oncogenes]] transduce cellular growth and proliferation signals downstream of [[Cell membranes|cell membrane]]–bound [[receptor]] [[tyrosine kinases]] (RTKs). [[Ras gene|Ras]] can be activated by [[gene]] [[amplification]], activating [[mutations]], or overexpression of upstream RTKs. Aberrant Ras activation promotes several key tumorigenic [[phenotypes]] including [[mitogenesis]], [[resistance]] to [[apoptosis]], [[drug]] [[resistance]], and <ref name="pmid16541145">{{cite journal |vauthors=Khavari PA |title=Modelling cancer in human skin tissue |journal=Nat. Rev. Cancer |volume=6 |issue=4 |pages=270–80 |date=April 2006 |pmid=16541145 |doi=10.1038/nrc1838 |url=}}</ref> | * [[Ras gene|Ras]] family members of [[Proto-oncogene|proto-oncogenes]] transduce [[cellular]] growth and [[proliferation]] signals downstream of [[Cell membranes|cell membrane]]–bound [[receptor]] [[tyrosine kinases]] (RTKs). [[Ras gene|Ras]] can be activated by [[gene]] [[amplification]], activating [[mutations]], or overexpression of upstream RTKs. Aberrant [[Ras gene|Ras]] activation promotes several key tumorigenic [[phenotypes]] including [[mitogenesis]], [[resistance]] to [[apoptosis]], [[drug]] [[resistance]], and <ref name="pmid16541145">{{cite journal |vauthors=Khavari PA |title=Modelling cancer in human skin tissue |journal=Nat. Rev. Cancer |volume=6 |issue=4 |pages=270–80 |date=April 2006 |pmid=16541145 |doi=10.1038/nrc1838 |url=}}</ref> | ||
[[Squamous cell carcinoma]] is a potentially [[invasive]] [[cancer]] that arises from the surface [[epithelium]].The development of [[squamous cell carcinoma]] is frequently a multistep process. Early lesions tend to be either [[actinic keratoses]], with atypia of the basal keratinocytic layer of the [[epidermis]] or [[squamous cell carcinoma]] in situ, in which [[keratinocytic]] atypia spans the full thickness [[epidermis]]. | [[Squamous cell carcinoma]] is a potentially [[invasive]] [[cancer]] that arises from the surface [[epithelium]].The development of [[squamous cell carcinoma]] is frequently a multistep process. Early lesions tend to be either [[actinic keratoses]], with atypia of the basal [[Keratinocytes|keratinocytic]] layer of the [[epidermis]] or [[squamous cell carcinoma]] in situ, in which [[Keratinocytes|keratinocytic]] atypia spans the full thickness [[epidermis]]. | ||
These precursors are frequently present adjacent to invasive [[squamous cell carcinomas]] which invade the [[dermis]] as nests, islands, or cords [[Squamous cell|squamous cells]] with or occasionally as individual [[Cells (biology)|cells]]. Several [[Grading (tumors)|grading]] schemes have been developed for [[squamous cell carcinoma]] and incorporate the extent of [[keratinization]] (a form of differentiation) and [[nuclear]] atypia. A widely used scheme divides [[tumors]] into well, moderately, or poorly [[Differentiate|differentiated]]. | These precursors are frequently present adjacent to invasive [[squamous cell carcinomas]] which invade the [[dermis]] as nests, islands, or cords [[Squamous cell|squamous cells]] with or occasionally as individual [[Cells (biology)|cells]]. Several [[Grading (tumors)|grading]] schemes have been developed for [[squamous cell carcinoma]] and incorporate the extent of [[keratinization]] (a form of differentiation) and [[nuclear]] atypia. A widely used scheme divides [[tumors]] into well, moderately, or poorly [[Differentiate|differentiated]]. | ||
Although poorly differentiated [[tumors]] tend to behave more aggressively, well-differentiated [[tumors]] can also give rise to [[metastasis]] and result in death. Several | Although poorly differentiated [[tumors]] tend to behave more aggressively, well-differentiated [[tumors]] can also give rise to [[metastasis]] and result in death. Several [[histological]] variants of [[squamous cell carcinoma]] have been documented, including [[Verrucous carcinoma|verrucous]], [[Spindle cells|spindle cell]] and [[pseudovascular]]. | ||
Frequently an [[actinic keratosis]] or [[squamous cell carcinoma]] overlies the [[invasive]] component and the two are focally [[contiguous]]. Occasionally [[squamous]] [[tumors]] arise rapidly, have a crater-form morphology and spontaneously regress. These [[tumors]] are known as [[Keratoacanthoma|keratoacanthomas]]. Some craterform [[squamous]] lesions do not regress, but continue to invade and grow and represent [[invasive]] [[squamous cell carcinomas]]. | Frequently an [[actinic keratosis]] or [[squamous cell carcinoma]] overlies the [[invasive]] component and the two are focally [[contiguous]]. Occasionally [[squamous]] [[tumors]] arise rapidly, have a crater-form morphology and spontaneously regress. These [[tumors]] are known as [[Keratoacanthoma|keratoacanthomas]]. Some craterform [[squamous]] lesions do not [[Regression|regress]], but continue to invade and grow and represent [[invasive]] [[squamous cell carcinomas]]. | ||
=== Microscopic Pathology === | === Microscopic Pathology === | ||
[[Histopathological examination]] confirms diagnosis and aids in the staging of the disease. [[Histopathological|Histopathology]] | [[Histopathological|Histopathological examination]] confirms diagnosis and aids in the [[Staging (pathology)|staging]] of the [[disease]]. [[Histopathological|Histopathology]] evaluates in detail the following characteristics of the specimen; | ||
*Invasion | |||
*Differentiation | |||
*[[Invasion]] | |||
*[[Differentiation]] | |||
*Depth | *Depth | ||
The various types of biopsy that may be obtained includes shave, punch, and excisional biopsies. The sample may be obtained at a physician's office under local anesthesia. The type of biopsy method chosen is based upon the size of lesion. | The various types of [[biopsy]] that may be obtained includes shave, punch, and [[Excisional biopsy|excisional biopsies]]. The sample may be obtained at a physician's office under [[local anesthesia]]. The type of [[biopsy]] method chosen is based upon the size of lesion. | ||
*For smaller lesions in easy accessible region of the body, an excisional biopsy is preferred. This may be therapeutic as well as diagnostic. | *For smaller lesions in easy accessible region of the body, an [[excisional biopsy]] is preferred. This may be [[therapeutic]] as well as [[diagnostic]]. | ||
*For lesions which are large and for which the cosmetic appearance may be of concern, a punch biopsy is advisable. Further treatment is based upon the results of histopathological evaluation. | *For lesions which are large and for which the [[Cosmetics|cosmetic]] appearance may be of concern, a [[punch biopsy]] is advisable. Further treatment is based upon the results of [[Histopathological|histopathological evaluation]]. | ||
*A shave biopsy is seldom recommended in cases where the lesion is suspected to be malignant. | *A shave [[biopsy]] is seldom recommended in cases where the lesion is suspected to be [[malignant]]. | ||
Important principles to consider when taking a sample for biopsy. | Important principles to consider when taking a sample for [[biopsy]]. | ||
* A full thickness biopsy should be taken to best evaluate the true depth of the lesion and extent of invasion. Depth of the lesion is an important determinant in the prognosis and staging of cancer.<ref>Brantsch KD, Meisner C, Schönfisch B, Trilling B, Wehner-Caroli J, Röcken M, et al. Analysis of risk factors determining prognosis of cutaneous squamous-cell carcinoma: a prospective study. Lancet Oncol. Aug 2008;9(8):713-20</ref> | * A full thickness biopsy should be taken to best evaluate the true depth of the lesion and extent of invasion. Depth of the lesion is an important determinant in the prognosis and staging of cancer.<ref>Brantsch KD, Meisner C, Schönfisch B, Trilling B, Wehner-Caroli J, Röcken M, et al. Analysis of risk factors determining prognosis of cutaneous squamous-cell carcinoma: a prospective study. Lancet Oncol. Aug 2008;9(8):713-20</ref> | ||
* The biopsy specimen should also include samples of normal tissue as a comparison. | * The biopsy specimen should also include samples of normal tissue as a comparison. | ||
* Large lesions require a thorough sample that will adequately assess the entirity of the lesion. | * Large lesions require a thorough sample that will adequately assess the entirity of the lesion. | ||
Toluidine Blue can be used for the early detection of the oral lesions of squamous cell carcinoma. It has high sensitivity, specificity and accuracy in detecting premalignant lesions. <ref>name="pmid22259809">{{cite journal |author=Rahman F, Tippu SR, Khandelwal S, Girish KL, Manjunath BC, Bhargava A |title=A study to evaluate the efficacy of toluidine blue and cytology in detecting oral cancer and dysplastic lesions |journal=Quintessence Int |volume=43 |issue=1 |pages=51–9 |year=2012 |month=January |pmid=22259809 |doi= |url=}}</ref> The basic principle surrounding the use of toluidine blue staining is that it doesn't stain the normal mucosa, however the dye is easily absorbed by the nuclei of malignant cells. | Toluidine Blue can be used for the early detection of the [[oral]] [[lesions]] of [[squamous cell carcinoma]]. It has high [[sensitivity]], [[specificity]] and [[accuracy]] in detecting [[premalignant]] lesions. <ref>name="pmid22259809">{{cite journal |author=Rahman F, Tippu SR, Khandelwal S, Girish KL, Manjunath BC, Bhargava A |title=A study to evaluate the efficacy of toluidine blue and cytology in detecting oral cancer and dysplastic lesions |journal=Quintessence Int |volume=43 |issue=1 |pages=51–9 |year=2012 |month=January |pmid=22259809 |doi= |url=}}</ref> The basic principle surrounding the use of toluidine blue staining is that it doesn't stain the normal [[mucosa]], however the dye is easily absorbed by the [[nuclei]] of [[malignant]] [[cells]]. | ||
Patients found to have regional lymphadenopathy on physical exam, or in imaging studies, should undergo lymph node biopsy or fine needle aspiration biopsy. | Patients found to have regional [[lymphadenopathy]] on [[physical exam]], or in [[imaging studies]], should undergo [[Lymph nodes|lymph node]] [[biopsy]] or [[Fine needle aspiration|fine needle aspiration biopsy.]] | ||
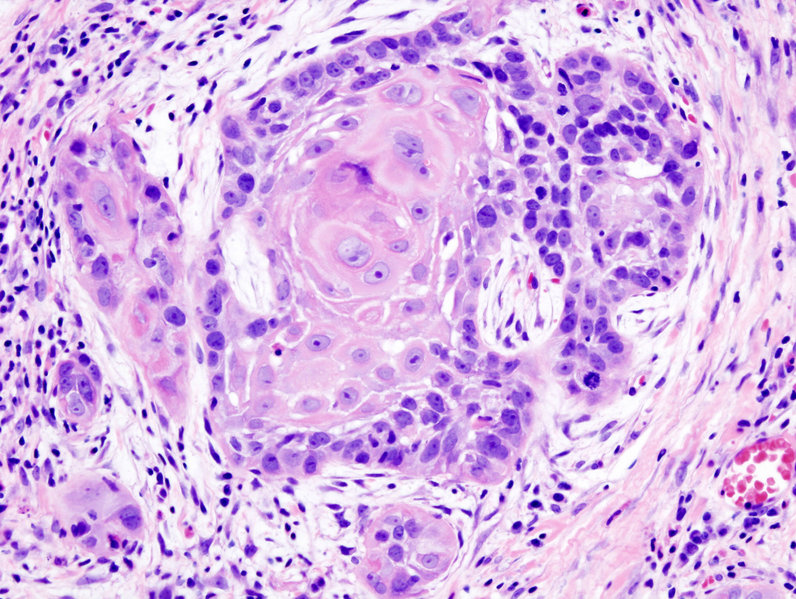
'''<u>Histological Findings</u>''' | '''<u>Histological Findings</u>''' | ||
Histopathological evaluation is important in determining the next step in the grade and treatment of the cancer. The neoplastic cells may demonstrate varying degrees of squamous differentiation and atypia uncder the microscope. | [[Histopathological|Histopathological evaluation]] is important in determining the next step in the [[Grading (tumors)|grade]] and treatment of the [[Cancer (medicine)|cancer.]] The [[Neoplastic|neoplastic cells]] may demonstrate varying degrees of [[squamous]] [[differentiation]] and [[atypia]] uncder the [[Microscopes|microscope]]. | ||
*The most conspicuous finding under a microscope are keratin pearls(well formed desmosome attachments and intracytoplasmic bundles of keratin tonofilaments). | *The most conspicuous finding under a [[Microscopes|microscope]] are [[Keratin|keratin pearls]](well formed [[Desmosomes|desmosome]] attachments and intracytoplasmic bundles of [[keratin]] tonofilaments). | ||
*SCC can be graded up to grade 3. | *SCC can be graded up to [[Grading (tumors)|grade]] 3. | ||
**Well differentiated: nuclei which are more normal, abundant cytoplasm & extracellular keratin pearls | **Well differentiated: nuclei which are more normal, abundant [[cytoplasm]] & [[extracellular]] keratin pearls | ||
**Poorly differentiated: High degree of nuclear atypia, greater nuclear:cytoplasmic ratio and less keratinization. Due to poor differentiation it may mimic mesenchymal tumors. Poorly differentiated carcinoma has a higher rate of metastasis and high rates of invasion into surrounding tissues. | **Poorly differentiated: High degree of nuclear atypia, greater nuclear:cytoplasmic ratio and less [[keratinization]]. Due to poor differentiation it may mimic mesenchymal tumors. Poorly differentiated carcinoma has a higher rate of metastasis and high rates of invasion into surrounding tissues. | ||
**Moderately differentiated: Has an appearance that is midway between poorly differentiated and well differentiated. | **Moderately differentiated: Has an appearance that is midway between poorly differentiated and well differentiated. | ||
**Squamous cell carcinoma in situ - has full thick atypia of squamous cells (including surfaces) without invasion through the basement membrane. | **Squamous cell carcinoma in situ - has full thick atypia of squamous cells (including surfaces) without invasion through the basement membrane. | ||
Revision as of 19:19, 28 May 2019
|
Squamous cell carcinoma of the skin Microchapters |
|
Differentiating Squamous cell carcinoma of the skin from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Squamous cell carcinoma of the skin pathophysiology On the Web |
|
American Roentgen Ray Society Images of Squamous cell carcinoma of the skin pathophysiology |
|
Squamous cell carcinoma of the skin pathophysiology in the news |
|
Blogs on Squamous cell carcinoma of the skin pathophysiology |
|
Directions to Hospitals Treating Squamous cell carcinoma of the skin |
|
Risk calculators and risk factors for Squamous cell carcinoma of the skin pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aditya Govindavarjhulla, M.B.B.S. [2], Raviteja Guddeti, M.B.B.S. [3]
Overview
Squamous cell carcinoma (SCC) is type of non-melanoma skin cancer. The cancer arises as a result of uncontrolled growth of the squamous cells in the epidermis of the skin. Unlike it's counter part, the basal cell carcinoma which also belongs to the group of non-melanoma cancer, squamous cell carcinoma is rapid growing and invasive. SCCs may occur on all areas of the body including the mucous membranes and genitals, but are most common in areas frequently exposed to the sun, such as the rim of the ear, lower lip, face, bald scalp, neck, hands, arms and legs. Wrinkling, changes in pigmentation, and loss of elasticity of the skin are often the telltale signs of sun damage.
Pathophysiology
- p53 is mutated commonly in Actinic keratosis, demonstrating that dysplastic lesions have acquired the initial genetic mutations prior to becoming cutaneous squamous cell carcinoma.[1]
- The mechanism leading to genomic instability in keratinocytes likely results from UVB-induced inactivation of p53, since approximately 58% of cutaneous squamous cell carcinoma harbor UVB signature mutations such as CC→TT and C→T transitions.[2]
- Aberrant activation of EGFR and Fyn, a Src-family tyrosine kinase (SFK), are seen in human cutaneous squamous cell carcinoma.
- Kinases downregulate p53 mRNA and protein levels through a c-Jun–dependent mechanism (28, 29), revealing another mechanism for controlling p53 function[3]
- Amplification and activating mutations of the Ras oncogene have been found in squamous cell carcinoma and Actnic keratosis
- Ras is an upstream activator of the Raf/Mek/Erk1/Erk2 kinase pathway, and activating mutations in Ras can promote cutaneous squamous cell carcinoma. formation. [4]
- Expression of β1-integrins and their ligands correlates with tumor progression in human skin.
- Ras family members of proto-oncogenes transduce cellular growth and proliferation signals downstream of cell membrane–bound receptor tyrosine kinases (RTKs). Ras can be activated by gene amplification, activating mutations, or overexpression of upstream RTKs. Aberrant Ras activation promotes several key tumorigenic phenotypes including mitogenesis, resistance to apoptosis, drug resistance, and [5]
Squamous cell carcinoma is a potentially invasive cancer that arises from the surface epithelium.The development of squamous cell carcinoma is frequently a multistep process. Early lesions tend to be either actinic keratoses, with atypia of the basal keratinocytic layer of the epidermis or squamous cell carcinoma in situ, in which keratinocytic atypia spans the full thickness epidermis.
These precursors are frequently present adjacent to invasive squamous cell carcinomas which invade the dermis as nests, islands, or cords squamous cells with or occasionally as individual cells. Several grading schemes have been developed for squamous cell carcinoma and incorporate the extent of keratinization (a form of differentiation) and nuclear atypia. A widely used scheme divides tumors into well, moderately, or poorly differentiated.
Although poorly differentiated tumors tend to behave more aggressively, well-differentiated tumors can also give rise to metastasis and result in death. Several histological variants of squamous cell carcinoma have been documented, including verrucous, spindle cell and pseudovascular.
Frequently an actinic keratosis or squamous cell carcinoma overlies the invasive component and the two are focally contiguous. Occasionally squamous tumors arise rapidly, have a crater-form morphology and spontaneously regress. These tumors are known as keratoacanthomas. Some craterform squamous lesions do not regress, but continue to invade and grow and represent invasive squamous cell carcinomas.
Microscopic Pathology
Histopathological examination confirms diagnosis and aids in the staging of the disease. Histopathology evaluates in detail the following characteristics of the specimen;
- Invasion
- Differentiation
- Depth
The various types of biopsy that may be obtained includes shave, punch, and excisional biopsies. The sample may be obtained at a physician's office under local anesthesia. The type of biopsy method chosen is based upon the size of lesion.
- For smaller lesions in easy accessible region of the body, an excisional biopsy is preferred. This may be therapeutic as well as diagnostic.
- For lesions which are large and for which the cosmetic appearance may be of concern, a punch biopsy is advisable. Further treatment is based upon the results of histopathological evaluation.
- A shave biopsy is seldom recommended in cases where the lesion is suspected to be malignant.
Important principles to consider when taking a sample for biopsy.
- A full thickness biopsy should be taken to best evaluate the true depth of the lesion and extent of invasion. Depth of the lesion is an important determinant in the prognosis and staging of cancer.[6]
- The biopsy specimen should also include samples of normal tissue as a comparison.
- Large lesions require a thorough sample that will adequately assess the entirity of the lesion.
Toluidine Blue can be used for the early detection of the oral lesions of squamous cell carcinoma. It has high sensitivity, specificity and accuracy in detecting premalignant lesions. [7] The basic principle surrounding the use of toluidine blue staining is that it doesn't stain the normal mucosa, however the dye is easily absorbed by the nuclei of malignant cells.
Patients found to have regional lymphadenopathy on physical exam, or in imaging studies, should undergo lymph node biopsy or fine needle aspiration biopsy.
Histological Findings Histopathological evaluation is important in determining the next step in the grade and treatment of the cancer. The neoplastic cells may demonstrate varying degrees of squamous differentiation and atypia uncder the microscope.
- The most conspicuous finding under a microscope are keratin pearls(well formed desmosome attachments and intracytoplasmic bundles of keratin tonofilaments).
- SCC can be graded up to grade 3.
- Well differentiated: nuclei which are more normal, abundant cytoplasm & extracellular keratin pearls
- Poorly differentiated: High degree of nuclear atypia, greater nuclear:cytoplasmic ratio and less keratinization. Due to poor differentiation it may mimic mesenchymal tumors. Poorly differentiated carcinoma has a higher rate of metastasis and high rates of invasion into surrounding tissues.
- Moderately differentiated: Has an appearance that is midway between poorly differentiated and well differentiated.
- Squamous cell carcinoma in situ - has full thick atypia of squamous cells (including surfaces) without invasion through the basement membrane.
- Invasive carcinomas cause the most inflammation upon invasion of the surrounding tissues.
Skin
Persons who present with Squamous cell carcinoma of skin may have one of the following risk factors like
- significant sun exposure
- benign lesions like Chalazion
- chronic ulcers.
-
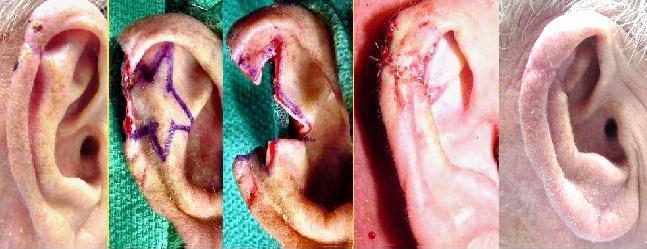
Squamous cell skin cancer.[8]
-
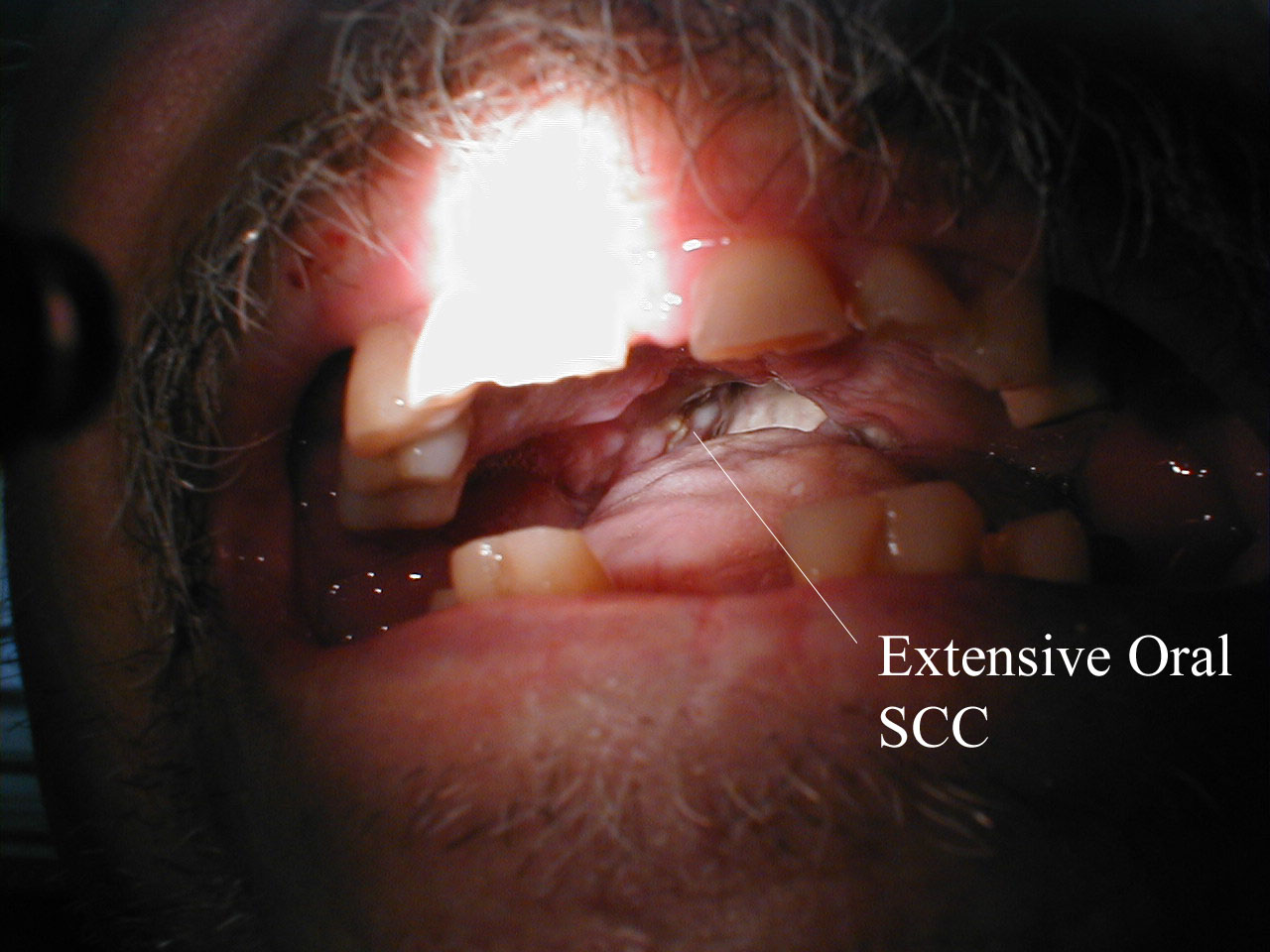
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
This patient had two adjacent cancers. The flat black lesion below the antitragus is a malignant melanoma. The white elevated keratotic lesion is a squamous cell carcinoma [9].
Presentation : They usually notice plaque. Ulcers are commonly seen over the face causing disfiguration. At times they can be exophytic over the lips etc.
Tongue and Esophagus
Persons who present with Squamous cell carcinoma of tongue and esophagus are most likely to have following risk factor
- Tobacco chewing/smoking
- Alcohol Abuse
- Poor dental hygiene
-
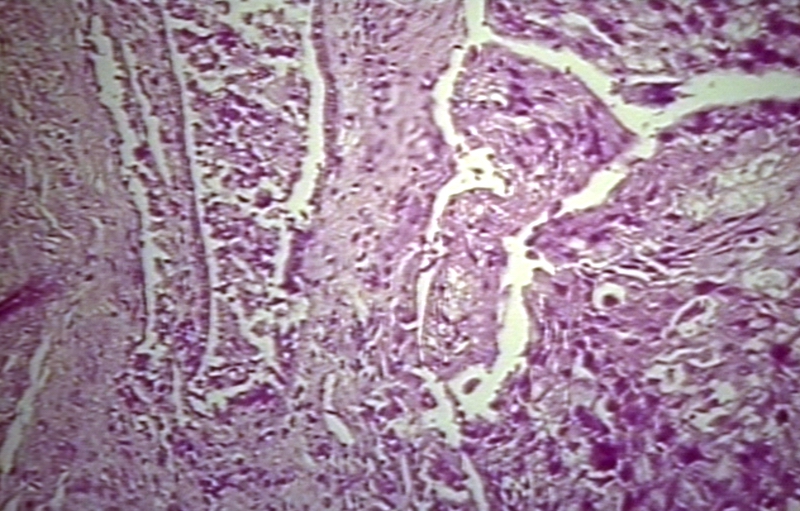
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
A large squamous cell carcinoma of the tongue[10]
Presentation : Its usually ulcerated in the lateral part of the tongue, pink - red color. Patient finds tough to eat or swallow. As it bleeds on touch or biting. They have dysphagia/ odynophagia when esophagus is involved. In later stages even liquids are tough to go thru. Swelling of lymph nodes is seen in advanced stages where we can find lumps in the neck
Nasopharynx
Persons who have SCC of this region seldom have any risk factors. It most of the times caused by EBV infection.
Presentation : Patient presents with symptoms from the mass effect of the tumour. They include nasal discharge, bleeding, obstruction; ear infection, deafness , tinnitus are complained. Other important complaints include headache and neck swelling due to lymph nodal spread.[11]
Lungs
Persons who have SCC of lungs usually have risk factors like
- Therapeutic radiation (PUVA for psoriais)
- Tobacco smoking
-
Biopsy of a highly differentiated squamous cell carcinoma of the mouth.Haematoxylin & eosin stain.
-
Photograph of a squamous cell carcinoma. Tumour is on the left, obstructing the bronchus (lung). Beyond the tumour the bronchus is inflammed and contains mucus
Presentation : Persons who present with SCC of lungs doesn't present usually with any typical symptoms of pulmonary. But in few we may see persistent cough, hemoptysis when it is exophytic and occupies whole of the bronchi which can even lead to recurrent infections.
Penis
Persons who present with Squamous cell carcinoma of penis are most likely to have
- Pre-malignanat lesions (Bowen's disease, Condyloma , Warts)
- Smoking and tobacco chewing
Presentation : Unhealed lesions, subtle indurations may be the intial presentation. Often presentation to the clinic is delayed due to embarrassment most of the times. Warts can be a pre-disposing factor.Large warts lead to infections and necrosis leading to hemorrhages at times.
Others
-
Squamous Cell Cancer of the Mouth: Cancer that began along the lower gum line has spread to left submandibular lymph nodes.
-
Squamous Cell Cancer of the Mouth: Cancer that began along the lower gum line has spread to left submandibular lymph nodes.
-
Recurrent squamous cell carcinoma of the auricle (far left) excised with a stellate incision across the antihelix.
-
The final result of the excision.
-
Squamous Cell Cancer of the Mouth: Irregular, necrotic appearing tissue on the inside of the mouth due to extensive squamous cell cancer. Patient has limited ability to open his mouth (aka trismus) as a result of the infiltrating cancer.
-
Squamous Cell Cancer, Base of Tongue: Note white area with swelling, right base of tongue.
-
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
Cervix: Squamous cell carcinoma
{{#ev:youtube|zB47nE-i8dQ}}
{{#ev:youtube|J3kULzKGzws}}
References
- ↑ Ortonne JP (April 2002). "From actinic keratosis to squamous cell carcinoma". Br. J. Dermatol. 146 Suppl 61: 20–3. PMID 11966728.
- ↑ Borelli D, Salas J (1975). "[The use of trypan blue instead of cotton blue in mycology]". Rev. Latinoam. Microbiol. (in Spanish; Castilian). 17 (3): 185–6. PMID 52880.
- ↑ Strabala TJ, Bednarek SY, Bertoni G, Amasino RM (April 1989). "Isolation and characterization of an ipt gene from the Ti plasmid Bo542". Mol. Gen. Genet. 216 (2–3): 388–94. PMID 2747621.
- ↑ Spencer JM, Kahn SM, Jiang W, DeLeo VA, Weinstein IB (July 1995). "Activated ras genes occur in human actinic keratoses, premalignant precursors to squamous cell carcinomas". Arch Dermatol. 131 (7): 796–800. PMID 7611795.
- ↑ Khavari PA (April 2006). "Modelling cancer in human skin tissue". Nat. Rev. Cancer. 6 (4): 270–80. doi:10.1038/nrc1838. PMID 16541145.
- ↑ Brantsch KD, Meisner C, Schönfisch B, Trilling B, Wehner-Caroli J, Röcken M, et al. Analysis of risk factors determining prognosis of cutaneous squamous-cell carcinoma: a prospective study. Lancet Oncol. Aug 2008;9(8):713-20
- ↑ name="pmid22259809">Rahman F, Tippu SR, Khandelwal S, Girish KL, Manjunath BC, Bhargava A (2012). "A study to evaluate the efficacy of toluidine blue and cytology in detecting oral cancer and dysplastic lesions". Quintessence Int. 43 (1): 51–9. PMID 22259809. Unknown parameter
|month=ignored (help) - ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ http://www.ghorayeb.com
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ Sham JS, Poon YF, Wei WI, Choy D. Nasopharyngeal carcinoma in young patients. Cancer. Jun 1 1990;65(11):2606-10.
![Squamous cell skin cancer.[8]](/images/1/17/Squamous_cell_skin_cancer.jpg)

![This patient had two adjacent cancers. The flat black lesion below the antitragus is a malignant melanoma. The white elevated keratotic lesion is a squamous cell carcinoma [9].](/images/f/f4/AuricleMelanoma_SqCC.jpg)

![A large squamous cell carcinoma of the tongue[10]](/images/e/e9/Squamous_cell_carcinoma.jpg)