Sporothrix schenckii: Difference between revisions
Shanshan Cen (talk | contribs) No edit summary |
No edit summary |
||
| (40 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Sporotrichosis}} | |||
{{Taxobox | {{Taxobox | ||
| image = | | image = Sporopix.png | ||
| image_width = 220px | | image_width = 220px | ||
| image_caption = | | image_caption = A micrograph of ''Sporothrix schenckii'' conidia stained with lactophenol cotton blue | ||
| regnum = [[Fungi]] | | regnum = [[Fungi]] | ||
| divisio = [[Ascomycota]] | | divisio = [[Ascomycota]] | ||
| Line 13: | Line 15: | ||
| binomial_authority = Hektoen & C.F.Perkins (1900) | | binomial_authority = Hektoen & C.F.Perkins (1900) | ||
}} | }} | ||
{{About0|Sporotrichosis}} | |||
{{CMG}} | |||
{{CMG}}; {{AE}} {{AJL}} | |||
==Overview== | ==Overview== | ||
'''''Sporothrix schenckii''''' is a [[fungus]] that can be found world | '''''Sporothrix schenckii''''' is a [[fungus]] that can be found throughout the world. Areas characterized by warm, humid climates, are ideal for the [[fungus]] to thrive. The [[species]] is present in soil as well as in and on living and decomposing plant material such as [[sphagnum|peat moss]]. It can infect humans as well as animals and is the causative agent of [[sporotrichosis]], commonly known as "rose handler's disease".<ref name="Vasquez">{{cite journal |author=Vásquez-del-Mercado E, Arenas R, Padilla-Desgarenes C |title=Sporotrichosis |journal=Clin. Dermatol. |volume=30 |issue=4 |pages=437–43 |date=July 2012 |pmid=22682194 |doi=10.1016/j.clindermatol.2011.09.017}}</ref> Posttraumatic inoculation of S. schenckii is the typical method of infection. However, sporotrichosis may also develop as a result of spore inhalation, although this mode of transmission is infrequent. Infection commonly occurs in otherwise [[immunocompetence|healthy]] individuals but is rarely life-threatening and can be treated with [[#Treatment|antifungals]]. In the environment, ''Sporothrix schenckii'' exists as a [[filamentous]] [[hypha]]e. In host tissue, ''S. schenckii'' thrives as a [[yeast]]. The transition from its [[Hyphae|hyphal]] form to [[yeast]] form is temperature dependent, making ''S. schenckii'' a [[thermally dimorphic fungus]].<ref name="Barros">{{cite journal |author=Barros MB, de Almeida Paes R, Schubach AO |title=''Sporothrix schenckii'' and Sporotrichosis |journal=Clin. Microbiol. Rev. |volume=24 |issue=4 |pages=633–54 |date=October 2011 |pmc=3194828 |doi=10.1128/cmr.00007-11 |pmid=21976602}}</ref> | ||
==Morphology== | ==Morphology== | ||
''Sporothrix schenckii'' can be found in one of two [[morphology (biology)|morphologies]], mold or [[yeast]], making it a dimorphic fungus. The saprophytic form is found in the environment on plants and decaying matter. When the [[fungus]] infects a host, the yeast form predominates as a result of its [[Thermally dimorphic fungus|temperature dependent morphology]].<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> | |||
===Hyphal=== | ===Saprophytic/Hyphal Form=== | ||
* At {{convert|25|C|F}}, in the environment or grown in the laboratory (in malt extract agar or [[Potato dextrose broth|potato dextrose agar]]), ''S. schenckii'' assumes its saprophytic stage.<ref name="Morris-Jones" /> | |||
* Macroscopically, colonies are characterized by apparent filaments, a smooth to leathery texture, and a finely wrinkled surface. Initially appearing off-white to creamy, the color may later become dark brown to black (“dirty candle-wax” color).<ref name="Barros" /> Some strains are capable of growing darkly colored colonies from initial formation. | |||
* Microscopically, composed of [[hyaline]], [[hyphae]] are [[hypha#Structure|septate]] and approximately 1 to 2μm in diameter. Arising from undifferentiated [[hyphae]], conidiogenous cells form clusters of [[conidia]] on denticles. [[Conidia]], which do not generate chains, are tear to clavate shaped and glass-like in appearance. They may be colorless or darkly colored. [[Conidia]] are sometimes referred to as resembling a flower.<ref name="MycologyOnline">[http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Hyphomycetes_%28dematiaceous%29/Sporothrix/] Mycology Online - University of Adelaide</ref> | |||
** Frequently, dark thick-walled [[conidia]] form adjacent to [[hyphae]], and serve as a tool to distinguish ''S. schenckii'' from alternative, nonpathogenic species of ''Sporothrix''. | |||
===Yeast=== | ===Yeast=== | ||
At {{convert|37|C|F}} either in | * At {{convert|37|C|F}} either in a laboratory or in host tissue, ''S. schenckii'' assumes its [[yeast]] form. | ||
* [[Macroscopic scale|Macroscopically]], the [[yeast]] form grows as smooth, white to tan colonies. | |||
* Microscopically, [[yeast]] cells are 2 to 6μm in diameter and have a round to oval shape. Typically, the cells appear to have elongated cigar-shaped buds stemming from a narrow origin.<ref name="Barros" /> <ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> | |||
== | |||
==Virulence Factors== | ==Virulence Factors== | ||
Virulence factors of ''S. schenckii'' are the microbial characteristics that catalyze or augment microbial growth in host tissue. | |||
===Melanin Production=== | ===Melanin Production=== | ||
''S. schenckii'' synthesizes [[melanin]] both ''in vitro'' and ''[[in vivo]]''<ref name = "Morris-Jones">{{cite journal |author=Morris-Jones R, Youngchim S, Gomez BL, ''et al.'' |title=Synthesis of melanin-like pigments by ''Sporothrix schenckii'' in vitro and during mammalian infection |journal=Infect. Immun. |volume=71 |issue=7 |pages=4026–33 |date=July 2003 |pmc=161969 |doi=10.1128/iai.71.7.4026-4033.2003 |pmid=12819091}}</ref> | *''S. schenckii'' synthesizes [[melanin]] both ''[[in vitro]]'' and ''[[in vivo]]'',<ref name="Morris-Jones">{{cite journal |author=Morris-Jones R, Youngchim S, Gomez BL, ''et al.'' |title=Synthesis of melanin-like pigments by ''Sporothrix schenckii'' in vitro and during mammalian infection |journal=Infect. Immun. |volume=71 |issue=7 |pages=4026–33 |date=July 2003 |pmc=161969 |doi=10.1128/iai.71.7.4026-4033.2003 |pmid=12819091}}</ref> meaning that both morphologies, [[yeast]] and mold, have the capacity to produce [[melanin]]. | ||
Melanin production is a virulence factor found in many fungi | *[[Melanin]] production is a virulence factor found in many pathogenic [[Fungus|fungi]]<ref name="Revankar">{{cite journal |author=Revankar SG, Sutton DA |title=Melanized fungi in human disease |journal=Clin. Microbiol. Rev. |volume=23 |issue=4 |pages=884–928 |date=October 2010 |pmc=2952981 |doi=10.1128/cmr.00019-10 |pmid=20930077}}</ref> and its production in ''S. schenckii'' protects the [[fungus]] from [[oxidative stress]] as well as [[ultraviolet]] light and [[macrophage]] killing. | ||
*[[Melanin]] has been shown to be synthesized using the 1,8-DHN pentaketide pathway.<ref name="Morris-Jones" /> | |||
*Melanization in ''S. schenckii'' is dependent on environmental factors such as, pH, temperature, and nutrient availability. Conidial menanization helps to enable the first stage of host infection, as it increases microbial resistance to macrophage [[phagocytosis]].<ref name="pmid25668479">{{cite journal| author=Freitas DF, Santos SS, Almeida-Paes R, de Oliveira MM, do Valle AC, Gutierrez-Galhardo MC et al.| title=Increase in virulence of Sporothrix brasiliensis over five years in a patient with chronic disseminated sporotrichosis. | journal=Virulence | year= 2015 | volume= 6 | issue= 2 | pages= 112-20 | pmid=25668479 | doi=10.1080/21505594.2015.1014274 | pmc=PMC4601271 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25668479 }} </ref> | |||
===Adhesins=== | ===Adhesins=== | ||
*Primary adhesion to [[extracellular matrix]] components and to [[epithelial]] and [[Endothelial cells|endothelial]] cells are necessary steps to effective pathogenesis. | |||
*Both the [[yeast]] and conidia cells of ''S. schenckii'' display an increased ability to recognize and subsequently bind<ref name="Barros" /> to [[extracellular matrix]] glycoproteins, [[fibronectin]], type II collagen, and [[laminin]], using separate receptors that are specific for these proteins<ref name="Lima">{{cite journal |author=Lima OC, Bouchara JP, Renier G, Marot-Leblond A, Chabasse D, Lopes-Bezerra LM |title=Immunofluorescence and flow cytometry analysis of fibronectin and laminin binding to ''Sporothrix schenckii'' yeast cells and conidia |journal=Microb. Pathog. |volume=37 |issue=3 |pages=131–40 |date=September 2004 |pmid=15351036 |doi=10.1016/j.micpath.2004.06.005}}</ref>. | |||
:*The [[fibronectin]] adhesions, which are found on the surface of [[yeast]] cells, are directly connected to virulence.<ref name="pmid19762444">{{cite journal| author=Teixeira PA, de Castro RA, Nascimento RC, Tronchin G, Torres AP, Lazéra M et al.| title=Cell surface expression of adhesins for fibronectin correlates with virulence in Sporothrix schenckii. | journal=Microbiology | year= 2009 | volume= 155 | issue= Pt 11 | pages= 3730-8 | pmid=19762444 | doi=10.1099/mic.0.029439-0 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19762444 }} </ref> | |||
*''S. schenckii'' is capable of crossing intercellular space, enabling hematogenous dissemination.<ref name="pmid15001223">{{cite journal| author=Figueiredo CC, De Lima OC, De Carvalho L, Lopes-Bezerra LM, Morandi V| title=The in vitro interaction of Sporothrix schenckii with human endothelial cells is modulated by cytokines and involves endothelial surface molecules. | journal=Microb Pathog | year= 2004 | volume= 36 | issue= 4 | pages= 177-88 | pmid=15001223 | doi=10.1016/j.micpath.2003.11.003 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15001223 }} </ref> | |||
===Proteases=== | ===Proteases=== | ||
''S. schenckii'' breaks down proteins by producing two separate [[protease]]s, a [[serine protease]] and an [[ | * ''S. schenckii'' breaks down proteins by producing two separate [[protease]]s, a [[serine protease]] and an [[Aspartic proteases|aspartic protease]].<ref name="Hogan">{{cite journal |author=Hogan LH, Klein BS, Levitz SM |title=Virulence factors of medically important fungi |journal=Clin. Microbiol. Rev. |volume=9 |issue=4 |pages=469–88 |date=October 1996 |pmc=172905 |pmid=8894347}}</ref> | ||
* These proteases appear to be essential for [[Fungus|fungal]] growth, however, they have some functional overlap. The inactivation of either protein does not affect growth, but inactivation of both inhibits the [[fungus]].<ref name="Tsuboi">{{cite journal |author=Tsuboi R, Sanada T, Ogawa H |title=Influence of culture medium pH and proteinase inhibitors on extracellular proteinase activity and cell growth of ''Sporothrix schenckii'' |journal=J. Clin. Microbiol. |volume=26 |issue=7 |pages=1431–3 |date=July 1988 |pmc=266631 |pmid=3045155}}</ref> | |||
* Protease activity has been shown to be important in ''[[in vivo]]'' infection of mice.<ref name="Hogan" /> Substrates for these proteases include the skin proteins [[type-I collagen]], [[stratum corneum]], and [[elastin]].<ref name="Hogan" /> | |||
===Heat Tolerance=== | ===Heat Tolerance=== | ||
Growing at host body temperature ({{convert|37|C|F}}) is an important requirement for pathogenesis. | *Growing at host body temperature ({{convert|37|C|F}}) is an important requirement for pathogenesis. | ||
*Strains of ''S. schenckii'' that are capable of growth at {{convert|35|C|F}}, but not {{convert|37|C|F}}, are only capable of causing the fixed cutaneous form of Sporotrichosis, as this form manifests with epidermal lesions (the skin is cooler than the body's interior). | |||
*Strains that are able to thrive at {{convert|37|C|F}} are responsible for lymphatic, disseminated, and extracutaneous/systematic forms of Sporotrichosis.<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> <ref name="Hogan" /> | |||
==Immune Response== | ==Immune Response== | ||
Infection by ''S. schenckii'' is generally [[self-limiting (biology)|self-limiting]] in immunocompetent hosts. The immune response prevents fungal dissemination and is the reason that most ''Sporothrix'' infections are [[#Cutaneous and Lymphocutaneous|cutaneous]].<ref name = "Carlos">{{cite journal |author=Carlos IZ, Sassá MF, da Graça Sgarbi DB, Placeres MC, Maia DC |title=Current research on the immune response to experimental sporotrichosis |journal=Mycopathologia |volume=168 |issue=1 |pages=1–10 |date=July 2009 |pmid=19241140 |doi=10.1007/s11046-009-9190-z}}</ref> | Infection by ''S. schenckii'' is generally [[self-limiting (biology)|self-limiting]] in [[immunocompetent]] hosts. The immune response prevents [[Fungus|fungal]] dissemination and is the reason that most ''Sporothrix'' infections are [[#Cutaneous and Lymphocutaneous|cutaneous]].<ref name="Carlos">{{cite journal |author=Carlos IZ, Sassá MF, da Graça Sgarbi DB, Placeres MC, Maia DC |title=Current research on the immune response to experimental sporotrichosis |journal=Mycopathologia |volume=168 |issue=1 |pages=1–10 |date=July 2009 |pmid=19241140 |doi=10.1007/s11046-009-9190-z}}</ref> | ||
===Innate=== | ===Innate=== | ||
The yeast form of ''S. schenckii'' is effectively [[phagocytosis|phagocytosed]] by [[innate immune system#Cells of the innate immune response|cells of the innate immune system]]<ref name = "Carlos" /> and are recognized based on the sugars displayed on their surface<ref name = "Oda">{{cite journal |author=Oda LM, Kubelka CF, Alviano CS, Travassos LR |title=Ingestion of yeast forms of ''Sporothrix schenckii'' by mouse peritoneal macrophages |journal=Infect. Immun. |volume=39 |issue=2 |pages=497–504 |date=February 1983 |pmc=347978 |pmid=6832808}}</ref> or lipids in the yeast cell | The yeast form of ''S. schenckii'' is effectively [[phagocytosis|phagocytosed]] by [[innate immune system#Cells of the innate immune response|cells of the innate immune system]]<ref name="Carlos" /> and are recognized based on the sugars displayed on their surface<ref name="Oda">{{cite journal |author=Oda LM, Kubelka CF, Alviano CS, Travassos LR |title=Ingestion of yeast forms of ''Sporothrix schenckii'' by mouse peritoneal macrophages |journal=Infect. Immun. |volume=39 |issue=2 |pages=497–504 |date=February 1983 |pmc=347978 |pmid=6832808}}</ref> or [[lipids]] in the [[yeast]] [[cell membrane]].<ref name="Carlos" /> Although they are taken up, they are not efficiently killed. It is hypothesized that ergosterol peroxide reacts with and detoxifies [[reactive oxygen species]] generated by the [[respiratory burst]] used by phagocytes to kill cells they have ingested.<ref name="Carlos" /> ''S. schenckii'' is also capable of modulating the immune response to promote its own survival by blocking [[cytokine]] production by macrophages.<ref name="Carlos" /> | ||
===Specific=== | ===Specific=== | ||
The specific immune response | The specific immune response becomes active at later stages of infection and involves both [[B cell]]s and [[T cell]]s. Severe sporotrichosis is rare in endemic areas where humans are in near constant contact with ''S. schenckii'' spores. This fact, combined with the increased severity of disease in [[Immunocompromised host|immunocompromised patients]], suggests an important role for [[adaptive immune system|specific immunity]] in ''S. schenckii'' infection.<ref name="Carlos" /> Patients with sporotrichosis have been shown to produce [[antibodies]] specific to ''S. schenckii''<ref name="Scott">{{cite journal |author=Scott EN, Muchmore HG |title=Immunoblot analysis of antibody responses to ''Sporothrix schenckii'' |journal=J. Clin. Microbiol. |volume=27 |issue=2 |pages=300–4 |date=February 1989 |pmc=267296 |pmid=2915023}}</ref> and these [[antibodies]] may actually be protective against the disease.<ref name="Barros" /> | ||
===Culture and Identification=== | |||
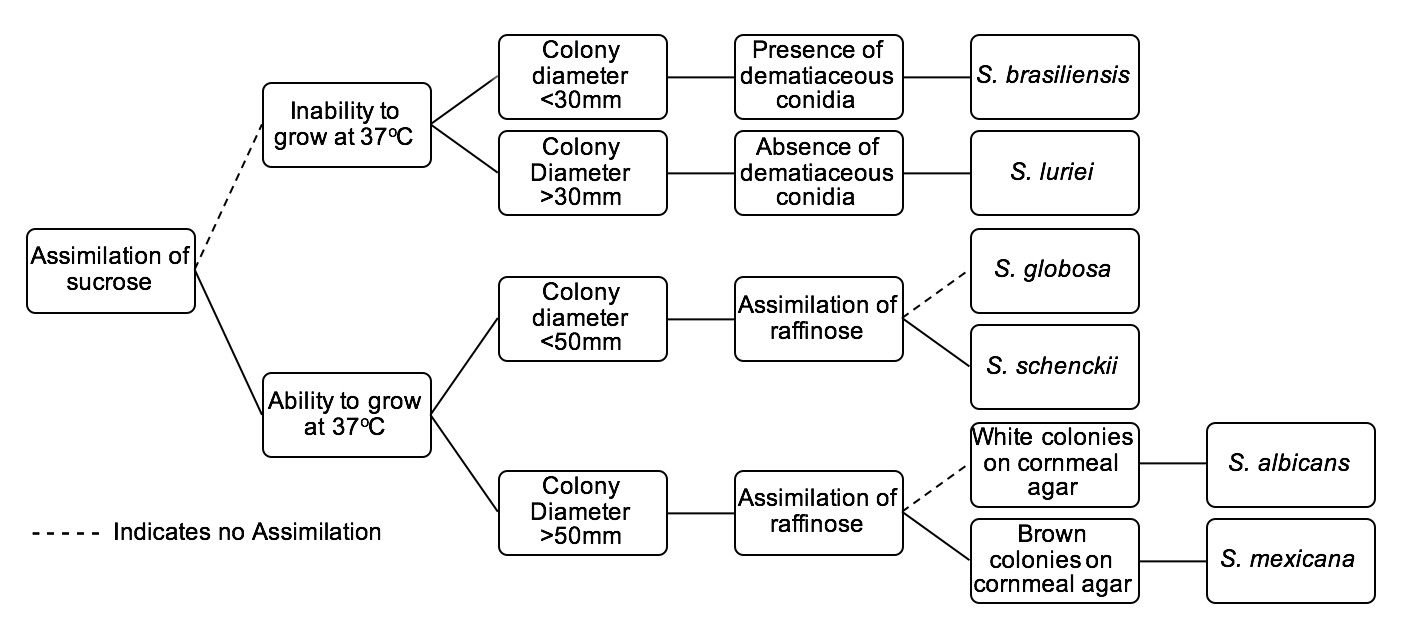
[[Image:Sporotree.jpg|thumb|none|800px|Identification tree for ''Sporothrix'' species of clinical interest. These clinically significant ''Sporothrix'' species include: ''S. brasiliensis'', ''S. luriei'', ''S. globosa'', ''S. schenckii'', ''S. albicans'', and ''S. mexicana''. When cultivating at 37°C, specimens are to be cultured on Potato Dextrose Agar.<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> ]] | |||
==References== | ==References== | ||
| Line 94: | Line 78: | ||
*[http://botit.botany.wisc.edu/toms_fungi/feb2003.html Fungus Page: ''Sporothrix schenckii'', cause of Rose-picker's Disease] | *[http://botit.botany.wisc.edu/toms_fungi/feb2003.html Fungus Page: ''Sporothrix schenckii'', cause of Rose-picker's Disease] | ||
*[http://emedicine.medscape.com/article/228723-overview EMedicine: Sporotrichosis] | *[http://emedicine.medscape.com/article/228723-overview EMedicine: Sporotrichosis] | ||
*[http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Hyphomycetes_%28dematiaceous%29/Sporothrix/ | *[http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Hyphomycetes_%28dematiaceous%29/Sporothrix/ Adelaide University: ''Sporothrix schenckii''] | ||
*[http://cmr.asm.org/content/24/4/633.abstract American Society for Microbiology: ''Sporothrix schenckii'' and Sporotrichosis] | *[http://cmr.asm.org/content/24/4/633.abstract American Society for Microbiology: ''Sporothrix schenckii'' and Sporotrichosis] | ||
*[http://microbewiki.kenyon.edu/index.php/Sporothrix_schenckii Microbe wiki: ''Sporothrix schenckii''] | *[http://microbewiki.kenyon.edu/index.php/Sporothrix_schenckii Microbe wiki: ''Sporothrix schenckii''] | ||
Latest revision as of 15:27, 28 January 2016
|
Sporotrichosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sporothrix schenckii On the Web |
|
American Roentgen Ray Society Images of Sporothrix schenckii |
| style="background:#Template:Taxobox colour;"|Template:Taxobox name | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
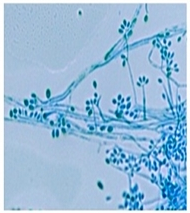 A micrograph of Sporothrix schenckii conidia stained with lactophenol cotton blue
| ||||||||||||||
| style="background:#Template:Taxobox colour;" | Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Sporothrix schenckii Hektoen & C.F.Perkins (1900) |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-in-Chief: Alison Leibowitz [3]
Overview
Sporothrix schenckii is a fungus that can be found throughout the world. Areas characterized by warm, humid climates, are ideal for the fungus to thrive. The species is present in soil as well as in and on living and decomposing plant material such as peat moss. It can infect humans as well as animals and is the causative agent of sporotrichosis, commonly known as "rose handler's disease".[1] Posttraumatic inoculation of S. schenckii is the typical method of infection. However, sporotrichosis may also develop as a result of spore inhalation, although this mode of transmission is infrequent. Infection commonly occurs in otherwise healthy individuals but is rarely life-threatening and can be treated with antifungals. In the environment, Sporothrix schenckii exists as a filamentous hyphae. In host tissue, S. schenckii thrives as a yeast. The transition from its hyphal form to yeast form is temperature dependent, making S. schenckii a thermally dimorphic fungus.[2]
Morphology
Sporothrix schenckii can be found in one of two morphologies, mold or yeast, making it a dimorphic fungus. The saprophytic form is found in the environment on plants and decaying matter. When the fungus infects a host, the yeast form predominates as a result of its temperature dependent morphology.[3]
Saprophytic/Hyphal Form
- At 25 °C (77 °F), in the environment or grown in the laboratory (in malt extract agar or potato dextrose agar), S. schenckii assumes its saprophytic stage.[4]
- Macroscopically, colonies are characterized by apparent filaments, a smooth to leathery texture, and a finely wrinkled surface. Initially appearing off-white to creamy, the color may later become dark brown to black (“dirty candle-wax” color).[2] Some strains are capable of growing darkly colored colonies from initial formation.
- Microscopically, composed of hyaline, hyphae are septate and approximately 1 to 2μm in diameter. Arising from undifferentiated hyphae, conidiogenous cells form clusters of conidia on denticles. Conidia, which do not generate chains, are tear to clavate shaped and glass-like in appearance. They may be colorless or darkly colored. Conidia are sometimes referred to as resembling a flower.[5]
Yeast
- At 37 °C (98.6 °F) either in a laboratory or in host tissue, S. schenckii assumes its yeast form.
- Macroscopically, the yeast form grows as smooth, white to tan colonies.
- Microscopically, yeast cells are 2 to 6μm in diameter and have a round to oval shape. Typically, the cells appear to have elongated cigar-shaped buds stemming from a narrow origin.[2] [3]
Virulence Factors
Virulence factors of S. schenckii are the microbial characteristics that catalyze or augment microbial growth in host tissue.
Melanin Production
- S. schenckii synthesizes melanin both in vitro and in vivo,[4] meaning that both morphologies, yeast and mold, have the capacity to produce melanin.
- Melanin production is a virulence factor found in many pathogenic fungi[6] and its production in S. schenckii protects the fungus from oxidative stress as well as ultraviolet light and macrophage killing.
- Melanin has been shown to be synthesized using the 1,8-DHN pentaketide pathway.[4]
- Melanization in S. schenckii is dependent on environmental factors such as, pH, temperature, and nutrient availability. Conidial menanization helps to enable the first stage of host infection, as it increases microbial resistance to macrophage phagocytosis.[7]
Adhesins
- Primary adhesion to extracellular matrix components and to epithelial and endothelial cells are necessary steps to effective pathogenesis.
- Both the yeast and conidia cells of S. schenckii display an increased ability to recognize and subsequently bind[2] to extracellular matrix glycoproteins, fibronectin, type II collagen, and laminin, using separate receptors that are specific for these proteins[8].
- The fibronectin adhesions, which are found on the surface of yeast cells, are directly connected to virulence.[9]
- S. schenckii is capable of crossing intercellular space, enabling hematogenous dissemination.[10]
Proteases
- S. schenckii breaks down proteins by producing two separate proteases, a serine protease and an aspartic protease.[11]
- These proteases appear to be essential for fungal growth, however, they have some functional overlap. The inactivation of either protein does not affect growth, but inactivation of both inhibits the fungus.[12]
- Protease activity has been shown to be important in in vivo infection of mice.[11] Substrates for these proteases include the skin proteins type-I collagen, stratum corneum, and elastin.[11]
Heat Tolerance
- Growing at host body temperature (37 °C (98.6 °F)) is an important requirement for pathogenesis.
- Strains of S. schenckii that are capable of growth at 35 °C (95 °F), but not 37 °C (98.6 °F), are only capable of causing the fixed cutaneous form of Sporotrichosis, as this form manifests with epidermal lesions (the skin is cooler than the body's interior).
- Strains that are able to thrive at 37 °C (98.6 °F) are responsible for lymphatic, disseminated, and extracutaneous/systematic forms of Sporotrichosis.[3] [11]
Immune Response
Infection by S. schenckii is generally self-limiting in immunocompetent hosts. The immune response prevents fungal dissemination and is the reason that most Sporothrix infections are cutaneous.[13]
Innate
The yeast form of S. schenckii is effectively phagocytosed by cells of the innate immune system[13] and are recognized based on the sugars displayed on their surface[14] or lipids in the yeast cell membrane.[13] Although they are taken up, they are not efficiently killed. It is hypothesized that ergosterol peroxide reacts with and detoxifies reactive oxygen species generated by the respiratory burst used by phagocytes to kill cells they have ingested.[13] S. schenckii is also capable of modulating the immune response to promote its own survival by blocking cytokine production by macrophages.[13]
Specific
The specific immune response becomes active at later stages of infection and involves both B cells and T cells. Severe sporotrichosis is rare in endemic areas where humans are in near constant contact with S. schenckii spores. This fact, combined with the increased severity of disease in immunocompromised patients, suggests an important role for specific immunity in S. schenckii infection.[13] Patients with sporotrichosis have been shown to produce antibodies specific to S. schenckii[15] and these antibodies may actually be protective against the disease.[2]
Culture and Identification
References
- ↑ Vásquez-del-Mercado E, Arenas R, Padilla-Desgarenes C (July 2012). "Sporotrichosis". Clin. Dermatol. 30 (4): 437–43. doi:10.1016/j.clindermatol.2011.09.017. PMID 22682194.
- ↑ 2.0 2.1 2.2 2.3 2.4 Barros MB, de Almeida Paes R, Schubach AO (October 2011). "Sporothrix schenckii and Sporotrichosis". Clin. Microbiol. Rev. 24 (4): 633–54. doi:10.1128/cmr.00007-11. PMC 3194828. PMID 21976602.
- ↑ 3.0 3.1 3.2 3.3 Barros MB, de Almeida Paes R, Schubach AO (2011). "Sporothrix schenckii and Sporotrichosis". Clin Microbiol Rev. 24 (4): 633–54. doi:10.1128/CMR.00007-11. PMC 3194828. PMID 21976602.
- ↑ 4.0 4.1 4.2 Morris-Jones R, Youngchim S, Gomez BL; et al. (July 2003). "Synthesis of melanin-like pigments by Sporothrix schenckii in vitro and during mammalian infection". Infect. Immun. 71 (7): 4026–33. doi:10.1128/iai.71.7.4026-4033.2003. PMC 161969. PMID 12819091.
- ↑ [1] Mycology Online - University of Adelaide
- ↑ Revankar SG, Sutton DA (October 2010). "Melanized fungi in human disease". Clin. Microbiol. Rev. 23 (4): 884–928. doi:10.1128/cmr.00019-10. PMC 2952981. PMID 20930077.
- ↑ Freitas DF, Santos SS, Almeida-Paes R, de Oliveira MM, do Valle AC, Gutierrez-Galhardo MC; et al. (2015). "Increase in virulence of Sporothrix brasiliensis over five years in a patient with chronic disseminated sporotrichosis". Virulence. 6 (2): 112–20. doi:10.1080/21505594.2015.1014274. PMC 4601271. PMID 25668479.
- ↑ Lima OC, Bouchara JP, Renier G, Marot-Leblond A, Chabasse D, Lopes-Bezerra LM (September 2004). "Immunofluorescence and flow cytometry analysis of fibronectin and laminin binding to Sporothrix schenckii yeast cells and conidia". Microb. Pathog. 37 (3): 131–40. doi:10.1016/j.micpath.2004.06.005. PMID 15351036.
- ↑ Teixeira PA, de Castro RA, Nascimento RC, Tronchin G, Torres AP, Lazéra M; et al. (2009). "Cell surface expression of adhesins for fibronectin correlates with virulence in Sporothrix schenckii". Microbiology. 155 (Pt 11): 3730–8. doi:10.1099/mic.0.029439-0. PMID 19762444.
- ↑ Figueiredo CC, De Lima OC, De Carvalho L, Lopes-Bezerra LM, Morandi V (2004). "The in vitro interaction of Sporothrix schenckii with human endothelial cells is modulated by cytokines and involves endothelial surface molecules". Microb Pathog. 36 (4): 177–88. doi:10.1016/j.micpath.2003.11.003. PMID 15001223.
- ↑ 11.0 11.1 11.2 11.3 Hogan LH, Klein BS, Levitz SM (October 1996). "Virulence factors of medically important fungi". Clin. Microbiol. Rev. 9 (4): 469–88. PMC 172905. PMID 8894347.
- ↑ Tsuboi R, Sanada T, Ogawa H (July 1988). "Influence of culture medium pH and proteinase inhibitors on extracellular proteinase activity and cell growth of Sporothrix schenckii". J. Clin. Microbiol. 26 (7): 1431–3. PMC 266631. PMID 3045155.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Carlos IZ, Sassá MF, da Graça Sgarbi DB, Placeres MC, Maia DC (July 2009). "Current research on the immune response to experimental sporotrichosis". Mycopathologia. 168 (1): 1–10. doi:10.1007/s11046-009-9190-z. PMID 19241140.
- ↑ Oda LM, Kubelka CF, Alviano CS, Travassos LR (February 1983). "Ingestion of yeast forms of Sporothrix schenckii by mouse peritoneal macrophages". Infect. Immun. 39 (2): 497–504. PMC 347978. PMID 6832808.
- ↑ Scott EN, Muchmore HG (February 1989). "Immunoblot analysis of antibody responses to Sporothrix schenckii". J. Clin. Microbiol. 27 (2): 300–4. PMC 267296. PMID 2915023.