Sheehan's syndrome pathophysiology: Difference between revisions
Iqra Qamar (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (19 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="-webkit-user-select: none;"> | |||
{| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" | |||
|- | |||
| {{#ev:youtube|_LGayYwSj50|450}} | |||
|- | |||
|} | |||
__NOTOC__ | __NOTOC__ | ||
{{Sheehan's syndrome}} | {{Sheehan's syndrome}} | ||
| Line 7: | Line 13: | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Background on | ===Background on pituitary gland blood supply=== | ||
*In order to understand the [[pathophysiology]] of Sheehan's syndrome, it is necessary to know the [[blood]] supply of the [[pituitary gland]], because Sheehan's syndrome occurs mainly by [[ischemia]] through different mechanisms such as compression or [[occlusion]] of blood supply to [[pituitary gland]]. | *In order to understand the [[pathophysiology]] of Sheehan's syndrome, it is necessary to know the [[blood]] supply of the [[pituitary gland]], because Sheehan's syndrome occurs mainly by [[ischemia]] through different mechanisms such as compression or [[occlusion]] of blood supply to [[pituitary gland]]. | ||
*[[Pituitary gland]] is amongst the most vascularized [[tissues]] in the body that normally weighs about 0.5 g but gets doubled in size during pregnancy.<ref name="pmid8325288">{{cite journal |vauthors=Rolih CA, Ober KP |title=Pituitary apoplexy |journal=Endocrinol. Metab. Clin. North Am. |volume=22 |issue=2 |pages=291–302 |year=1993 |pmid=8325288 |doi= |url=}}</ref> | *[[Pituitary gland]] is amongst the most vascularized [[tissues]] in the body that normally weighs about 0.5 g but gets doubled in size during pregnancy.<ref name="pmid8325288">{{cite journal |vauthors=Rolih CA, Ober KP |title=Pituitary apoplexy |journal=Endocrinol. Metab. Clin. North Am. |volume=22 |issue=2 |pages=291–302 |year=1993 |pmid=8325288 |doi= |url=}}</ref> | ||
*The [[pituitary gland]] is composed of two parts [[anterior]] ([[adenohypophysis]]) and [[posterior]] ([[neurohypophysis]]). Both parts are supplied by the [[carotid arteries]]. | *The [[pituitary gland]] is composed of two parts [[anterior]] ([[adenohypophysis]]) and [[posterior]] ([[neurohypophysis]]). Both parts are supplied by the [[carotid arteries]]. | ||
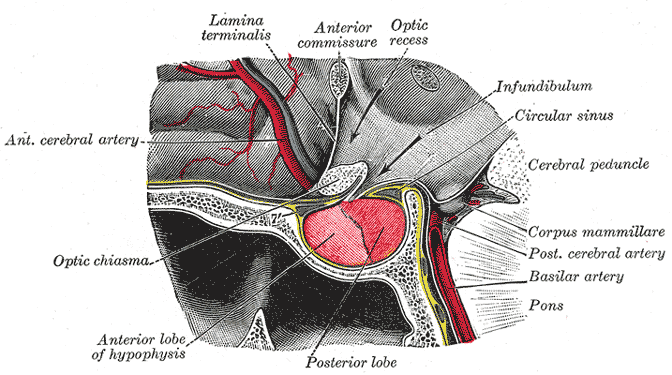
[[Image: Gray1180.png|500 px|thumb|center|A pituitary gland anatomy By Henry Vandyke Carte - Via: Wikimedia.org<ref> Henry Gray (1918) Anatomy of the Human Body, Bartleby.com: Gray's Anatomy, Plate 721, Public Domain, <https://commons.wikimedia.org/w/index.php?curid=541543></ref>]] | |||
=== | === Anterior pituitary (Adenohypophysis) === | ||
*[[Anterior pituitary gland|Anterior pituitary]] does not have a direct [[blood]] supply and is supplied by the [[hypophyseal portal system]]. | *[[Anterior pituitary gland|Anterior pituitary]] does not have a direct [[blood]] supply and is supplied by the [[hypophyseal portal system]]. | ||
*The [[hypophyseal portal system]] is a [[Fenestration|fenestrated]] set of [[capillaries]] that allows rapid exchange of [[hormones]] between the [[hypothalamus]] and [[anterior pituitary]]. | *The [[hypophyseal portal system]] is a [[Fenestration|fenestrated]] set of [[capillaries]] that allows rapid exchange of [[hormones]] between the [[hypothalamus]] and [[anterior pituitary]]. | ||
*Occlusion of the [[blood]] supply and other [[vascular]] abnormalities of the [[hypophyseal portal system]] may also cause [[complications]] with the exchange of [[hormones]] between the [[hypothalamus]] and the [[pituitary gland]] leading to [[hypopituitarism]]. | *Occlusion of the [[blood]] supply and other [[vascular]] abnormalities of the [[hypophyseal portal system]] may also cause [[complications]] with the exchange of [[hormones]] between the [[hypothalamus]] and the [[pituitary gland]] leading to [[hypopituitarism]]. | ||
=== | === Posterior pituitary (Neurohypophysis) === | ||
*[[Posterior pituitary]] has its own [[blood]] supply via [[inferior hypophyseal artery]] and is less commonly affected as compared to [[anterior pituitary]]. | *[[Posterior pituitary]] has its own [[blood]] supply via [[inferior hypophyseal artery]] and is less commonly affected as compared to [[anterior pituitary]]. | ||
*If [[posterior pituitary]] is affected, it can result in [[Neurohypophysis|neurohypophseal]] dysfunction and [[ischemic necrosis]] of [[thirst]] center leading to increased [[osmotic]] threshold for thirst onset.<ref name="pmid17468192">{{cite journal |vauthors=Atmaca H, Tanriverdi F, Gokce C, Unluhizarci K, Kelestimur F |title=Posterior pituitary function in Sheehan's syndrome |journal=Eur. J. Endocrinol. |volume=156 |issue=5 |pages=563–7 |year=2007 |pmid=17468192 |doi=10.1530/EJE-06-0727 |url=}}</ref> | *If [[posterior pituitary]] is affected, it can result in [[Neurohypophysis|neurohypophseal]] dysfunction and [[ischemic necrosis]] of [[thirst]] center leading to increased [[osmotic]] threshold for thirst onset.<ref name="pmid17468192">{{cite journal |vauthors=Atmaca H, Tanriverdi F, Gokce C, Unluhizarci K, Kelestimur F |title=Posterior pituitary function in Sheehan's syndrome |journal=Eur. J. Endocrinol. |volume=156 |issue=5 |pages=563–7 |year=2007 |pmid=17468192 |doi=10.1530/EJE-06-0727 |url=}}</ref> | ||
=== | ===Hypothalamic and pituitary hormones with their action on the target glands=== | ||
{| class="wikitable" | {| class="wikitable" | ||
! | ! | ||
! | !Hypothalamic hormone | ||
!Mode of action | !Mode of action | ||
! | !Pituitary hormone | ||
or target | or target organ | ||
!Action | !Action | ||
|- | |- | ||
| Line 51: | Line 58: | ||
* [[Luteinizing hormone|Leutinizing hormone]] | * [[Luteinizing hormone|Leutinizing hormone]] | ||
| | | | ||
* Males: | * Males: Stimulates [[testosterone]] production and [[spermatogenesis]] | ||
* Female: | * Female: Stimulates [[estradiol]] and [[progesterone]] production, [[ovulation]] and [[folliculogenesis]] | ||
|- | |- | ||
|[[Dopamine]] | |[[Dopamine]] | ||
| Line 72: | Line 79: | ||
|[[Vasopressin]] | |[[Vasopressin]] | ||
|Stimulatory | |Stimulatory | ||
| | |[[Kidney]] | ||
|Stimulates free water reabsorption in the [[collecting ducts]] | |Stimulates free water reabsorption in the [[collecting ducts]] | ||
|- | |- | ||
| Line 82: | Line 89: | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
*Sheehan's syndrome occurs mainly due to [[ischemic necrosis]] of [[pituitary gland]] causing destruction of the [[pituitary gland]] cells that results in decreased production of one or more [[pituitary]] [[hormones]] depending upon the severity of damage. | *Sheehan's syndrome occurs mainly due to [[ischemic necrosis]] of [[pituitary gland]] causing destruction of the [[pituitary gland]] cells, that results in decreased production of one or more [[pituitary]] [[hormones]] depending upon the severity of damage. | ||
* | *Sheehan's syndrome results in mild to severe pituitary dysfunction which can lead to partial or [[panhypopituitarism]], such as [[Growth hormone|GH]], [[thyroid hormone]], [[glucocorticoid]], [[gonadotropins]] ([[LH]], [[FSH]]), and [[prolactin]] hormone deficiencies; that manifest as a wide spectrum of presentation.<ref name="pmid8043090">{{cite journal |vauthors=Vance ML |title=Hypopituitarism |journal=N. Engl. J. Med. |volume=330 |issue=23 |pages=1651–62 |year=1994 |pmid=8043090 |doi=10.1056/NEJM199406093302306 |url=}}</ref> | ||
*Usually, [[Growth hormone|GH]] levels | *Usually, [[Growth hormone|GH]] levels decreased first before others.<ref name="pmid15237929">{{cite journal |vauthors=Keleştimur F |title=Sheehan's syndrome |journal=Pituitary |volume=6 |issue=4 |pages=181–8 |year=2003 |pmid=15237929 |doi= |url=}}</ref>Amongst all [[pituitary]] [[hormones]], the first and the most common [[hormonal]] deficiency seen in [[hypopituitarism]] is growth hormone deficiency followed by deficiencies of [[gonadotropins]] ([[FSH]], [[LH]]), [[TSH]], [[ACTH]] and [[Prolactin|prolactin.]]<ref name="pmid7955461">{{cite journal |vauthors=Toogood AA, Beardwell CG, Shalet SM |title=The severity of growth hormone deficiency in adults with pituitary disease is related to the degree of hypopituitarism |journal=Clin. Endocrinol. (Oxf) |volume=41 |issue=4 |pages=511–6 |year=1994 |pmid=7955461 |doi= |url=}}</ref><ref name="pmid10770165">{{cite journal |vauthors=Benvenga S, Campenní A, Ruggeri RM, Trimarchi F |title=Clinical review 113: Hypopituitarism secondary to head trauma |journal=J. Clin. Endocrinol. Metab. |volume=85 |issue=4 |pages=1353–61 |year=2000 |pmid=10770165 |doi=10.1210/jcem.85.4.6506 |url=}}</ref><ref name="pmid11059653">{{cite journal |vauthors=Kelly DF, Gonzalo IT, Cohan P, Berman N, Swerdloff R, Wang C |title=Hypopituitarism following traumatic brain injury and aneurysmal subarachnoid hemorrhage: a preliminary report |journal=J. Neurosurg. |volume=93 |issue=5 |pages=743–52 |year=2000 |pmid=11059653 |doi=10.3171/jns.2000.93.5.0743 |url=}}</ref> | ||
====Compression of the [[blood vessels]]:==== | ====Compression of the blood vessels==== | ||
< | '''(a) Pituitary gland enlargement''' | ||
{{familytree/start}} | *[[Pituitary gland]] enlargement due to [[hypertrophy]] and [[hyperplasia]] of [[Lactotrophs|lactotrophic cells]] in [[anterior pituitary]] results in [[superior hypophyseal artery]] compression, which is complicated by decreased portal pressure and [[vasospasm]] during delivery, playing an important role in the [[pathogenesis]] of Sheehan's syndrome.<ref name="pmid2159093">{{cite journal |vauthors=Scheithauer BW, Sano T, Kovacs KT, Young WF, Ryan N, Randall RV |title=The pituitary gland in pregnancy: a clinicopathologic and immunohistochemical study of 69 cases |journal=Mayo Clin. Proc. |volume=65 |issue=4 |pages=461–74 |year=1990 |pmid=2159093 |doi= |url=}}</ref> | ||
*[[Pituitary gland]] enlargement results in increasing its [[blood]] and [[oxygen]] demand, thus making it more susceptible to [[ischemia]] in a setting of massive [[hemorrhage]] during or after [[parturition]]. | |||
'''(b) Smaller size of sella''' | |||
* Smaller and rigid [[sella]] may also be associated with compression of [[blood vessels]] supplying the [[pituitary]] resulting in compromised [[blood]] supply. | |||
==== Vascular abnormalities causing vascular occlusion<ref name="pmid15237929">{{cite journal |vauthors=Keleştimur F |title=Sheehan's syndrome |journal=Pituitary |volume=6 |issue=4 |pages=181–8 |year=2003 |pmid=15237929 |doi= |url=}}</ref><ref name="McKayMerrill1953">{{cite journal|last1=McKay|first1=Donald G.|last2=Merrill|first2=Samuel J.|last3=Weiner|first3=Albert E.|last4=Hertig|first4=Arthur T.|last5=Reid|first5=Duncan E.|title=The pathologic anatomy of eclampsia, bilateral renal cortical necrosis, pituitary necrosis, and other acute fatal complications of pregnancy, and its possible relationship to the generalized Shwartzman phenomenon|journal=American Journal of Obstetrics and Gynecology|volume=66|issue=3|year=1953|pages=507–539|issn=00029378|doi=10.1016/0002-9378(53)90068-4}}</ref><ref>{{cite journal |last=Apitz |first=Kurt |date=September 1, 1935 |title=A Study of the Generalized Shwartzman Phenomenon|url=http://www.jimmunol.org/content/29/3/255.short|journal=The Journal of Immunology |volume=29 |issue=3 |pages=255-266}}</ref> ==== | |||
'''(a) Vasospasm''' | |||
*[[Vasospasm]] due to severe [[Postpartum hemorrhage|postpartum hemorrhage (PPH)]] (loss of > 500 ml of blood during the first 24 hr), leading to [[hypotension]] and [[ischemic necrosis]] of [[pituitary gland]], is the most common cause of Sheehan's syndrome.<ref name="pmid15237929">{{cite journal |vauthors=Keleştimur F, Chow YW, Pietranico R, Mukerji A, Wiesmann UN, DiDonato S, Herschkowitz NN, Voigt WG, Johnson CR, Moroi K, Sato T, Keleştimur F, Goswami R, Kochupillai N, Crock PA, Jaleel A, Gupta N, Wrightstone RN, Smith LL, Wilson JB, Vella F, Huisman TH, Marniemi J, Parkki MG, Ward CW, Stellwagen E, Babul J, Pogodina VV, Goswami R, Kochupillai N, Crock PA, Jaleel A, Gupta N, Schmoldt A, Benthe HF, Haberland G, Lyons HA, Thomas JS, Heurich AE, Shepherd DA, Wetmore SD, Mekler LB, Sealey JE, White RP, Laragh JH, Rubin AL, Makar AB, McMartin KE, Palese M, Tephly TR, Frankle RT, Makar AB, McMartin KE, Palese M, Tephly TR, Makar AB, McMartin KE, Palese M, Tephly TR, Makar AB, McMartin KE, Palese M, Tephly TR, Makar AB, McMartin KE, Palese M, Tephly TR, Frankle RT, Thornton JA, Harrison MJ, Stellwagen E, Babul J, Leroy M, Loas G, Perez-Diaz F, Schmoldt A, Benthe HF, Haberland G, Coller BS, Franza BR, Gralnick HR |title=Sheehan's syndrome |journal=Pituitary |volume=6 |issue=4 |pages=181–8 |year=2003 |pmid=15237929 |doi=10.1210/jc.2001-020242 |url=}}</ref> | |||
'''(b) Disseminated intravascular coagulation (DIC)''' | |||
* [[Disseminated intravascular coagulation|DIC]] results in [[intravascular]] [[fibrin]] deposition leading to [[occlusion]] in [[hypophyseal portal system]], thus contributing to the [[ischemia]] of [[pituitary gland]] [[cells]]. | |||
* The pathophysiologic mechanism behind [[intravascular]] [[fibrin]] deposition is found to be similar to that of [[Shwartzman phenomenon|generalized Shwartzman reaction]]. | |||
==== Autoimmunity ==== | |||
*It is believed that [[Necrosis|tissue necrosis]] results in the release of sequestered [[antigens]], precipitating [[autoimmunity]] of the [[pituitary gland]] and [[hypopituitarism]] in [[Sheehan's syndrome]].<ref name="pmid12213861">{{cite journal |vauthors=Goswami R, Kochupillai N, Crock PA, Jaleel A, Gupta N |title=Pituitary autoimmunity in patients with Sheehan's syndrome |journal=J. Clin. Endocrinol. Metab. |volume=87 |issue=9 |pages=4137–41 |year=2002 |pmid=12213861 |doi=10.1210/jc.2001-020242 |url=}}</ref><ref name="urlAUTOANTIBODIES IN SHEEHANS SYNDROME - ScienceDirect">{{cite web |url=http://www.sciencedirect.com/science/article/pii/S0140673665913619?via%3Dihub |title=AUTOANTIBODIES IN SHEEHAN'S SYNDROME - ScienceDirect |format= |work= |accessdate=}}</ref><ref name="pmid24434361">{{cite journal |vauthors=Falorni A, Minarelli V, Bartoloni E, Alunno A, Gerli R |title=Diagnosis and classification of autoimmune hypophysitis |journal=Autoimmun Rev |volume=13 |issue=4-5 |pages=412–6 |year=2014 |pmid=24434361 |doi=10.1016/j.autrev.2014.01.021 |url=}}</ref> | |||
<br>{{familytree/start}} | |||
{{familytree | | A01 | | | A02 | | | A03 | | | A04 | | | A05 | |A01=[[DIC]]<sup>‡</sup>|A02=Severe [[PPH]]<sup>†</sup>|A03=[[Glandular]] [[hypertrophy]] and [[hyperplasia]]|A04=Small [[sella]] size|A05=[[Autoimmunity]]}} | {{familytree | | A01 | | | A02 | | | A03 | | | A04 | | | A05 | |A01=[[DIC]]<sup>‡</sup>|A02=Severe [[PPH]]<sup>†</sup>|A03=[[Glandular]] [[hypertrophy]] and [[hyperplasia]]|A04=Small [[sella]] size|A05=[[Autoimmunity]]}} | ||
{{familytree | | |!| | | | |!| | | | |!| | | | |!| | | | |!| | }} | {{familytree | | |!| | | | |!| | | | |!| | | | |!| | | | |!| | }} | ||
| Line 105: | Line 128: | ||
<br> | <br> | ||
†[[Postpartum Hemorrhage|Postpartum hemorrhage (PPH)]] i.e., >500 ml after [[Vaginal|vaginal delivery]] or 1000 ml after [[C-section]]. | †[[Postpartum Hemorrhage|Postpartum hemorrhage (PPH)]] i.e., >500 ml after [[Vaginal|vaginal delivery]] or 1000 ml after [[C-section]]. | ||
<br> </small></small | <br></small></small> | ||
==Genetics== | ==Genetics== | ||
There is no genetic association found to be associated with Sheehan's syndrome. | There is no [[genetic]] association found to be associated with Sheehan's syndrome. | ||
==Associated Conditions== | ==Associated Conditions== | ||
| Line 130: | Line 149: | ||
*[[Scarring]] of [[Paraventricular nucleus of hypothalamus|paraventricular]] and [[Supraoptic nucleus|supraoptic nuclei]] | *[[Scarring]] of [[Paraventricular nucleus of hypothalamus|paraventricular]] and [[Supraoptic nucleus|supraoptic nuclei]] | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
| |||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category:Medicine]] | |||
[[Category:Endocrinology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Obstetrics]] | |||
Latest revision as of 00:09, 30 July 2020
| _LGayYwSj50|450}} |
|
Sheehan's syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sheehan's syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Sheehan's syndrome pathophysiology |
|
Risk calculators and risk factors for Sheehan's syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Iqra Qamar M.D.[2]
Overview
It is thought that Sheehan's syndrome is the result of ischemic necrosis of pituitary gland, due to pituitary gland enlargement during parturition; precipitated by hypotension due to massive hemorrhage. Apart from pituitary gland enlargement during and before parturition, vasospasm, generalized Schwartzman phenomenon, thrombosis and compression of the hypophyseal arteries, autoimmunity, DIC, and smaller size of sella play a contributing role in pathogenesis of Sheehan syndrome. Occlusion and other vascular anomalies of the hypophyseal portal system can also complicate the exchange of hormones between the hypothalamus and the pituitary gland, leading to hypopituitarism. Sheehan's syndrome may result in mild to severe pituitary dysfunction (partial or panhypopituitarism), which is identified with growth hormone (GH), thyroid hormone, glucocorticoid, gonadotropins, and prolactin hormone deficiencies; manifests as a wide spectrum of presentation. Usually, GH deficiency is the earliest one to develop.
Pathophysiology
Background on pituitary gland blood supply
- In order to understand the pathophysiology of Sheehan's syndrome, it is necessary to know the blood supply of the pituitary gland, because Sheehan's syndrome occurs mainly by ischemia through different mechanisms such as compression or occlusion of blood supply to pituitary gland.
- Pituitary gland is amongst the most vascularized tissues in the body that normally weighs about 0.5 g but gets doubled in size during pregnancy.[1]
- The pituitary gland is composed of two parts anterior (adenohypophysis) and posterior (neurohypophysis). Both parts are supplied by the carotid arteries.
Anterior pituitary (Adenohypophysis)
- Anterior pituitary does not have a direct blood supply and is supplied by the hypophyseal portal system.
- The hypophyseal portal system is a fenestrated set of capillaries that allows rapid exchange of hormones between the hypothalamus and anterior pituitary.
- Occlusion of the blood supply and other vascular abnormalities of the hypophyseal portal system may also cause complications with the exchange of hormones between the hypothalamus and the pituitary gland leading to hypopituitarism.
Posterior pituitary (Neurohypophysis)
- Posterior pituitary has its own blood supply via inferior hypophyseal artery and is less commonly affected as compared to anterior pituitary.
- If posterior pituitary is affected, it can result in neurohypophseal dysfunction and ischemic necrosis of thirst center leading to increased osmotic threshold for thirst onset.[3]
Hypothalamic and pituitary hormones with their action on the target glands
| Hypothalamic hormone | Mode of action | Pituitary hormone
or target organ |
Action | |
|---|---|---|---|---|
| Anterior pituitary hormones | Thyrotropin-releasing hormone | Stimulatory | Thyrotropin | Stimulates triiodothyronine and thyroxine production |
| Corticotropin-releasing hormone | Stimulatory | Corticotropin | Stimulates production of cortisol and adrenal androgens | |
| Stimulatory | Prolactin | Stimulates milk production from breasts in females | ||
| Gonadotropin-releasing hormone | Stimulatory |
| ||
| Dopamine | Inhibitory | Prolactin | _ | |
| Growth hormone-releasing hormone | Stimulatory | Growth hormone | Stimulates insulin-like growth factor 1 production | |
| Somatostatin | Inhibitory | Growth hormone | _ | |
| Posterior pituitary hormones | Vasopressin | Stimulatory | Kidney | Stimulates free water reabsorption in the collecting ducts |
| Oxytocin | Stimulatory | Breast, uterus | Stimulates milk ejection and uterine contraction |
Pathogenesis
- Sheehan's syndrome occurs mainly due to ischemic necrosis of pituitary gland causing destruction of the pituitary gland cells, that results in decreased production of one or more pituitary hormones depending upon the severity of damage.
- Sheehan's syndrome results in mild to severe pituitary dysfunction which can lead to partial or panhypopituitarism, such as GH, thyroid hormone, glucocorticoid, gonadotropins (LH, FSH), and prolactin hormone deficiencies; that manifest as a wide spectrum of presentation.[4]
- Usually, GH levels decreased first before others.[5]Amongst all pituitary hormones, the first and the most common hormonal deficiency seen in hypopituitarism is growth hormone deficiency followed by deficiencies of gonadotropins (FSH, LH), TSH, ACTH and prolactin.[6][7][8]
Compression of the blood vessels
(a) Pituitary gland enlargement
- Pituitary gland enlargement due to hypertrophy and hyperplasia of lactotrophic cells in anterior pituitary results in superior hypophyseal artery compression, which is complicated by decreased portal pressure and vasospasm during delivery, playing an important role in the pathogenesis of Sheehan's syndrome.[9]
- Pituitary gland enlargement results in increasing its blood and oxygen demand, thus making it more susceptible to ischemia in a setting of massive hemorrhage during or after parturition.
(b) Smaller size of sella
- Smaller and rigid sella may also be associated with compression of blood vessels supplying the pituitary resulting in compromised blood supply.
Vascular abnormalities causing vascular occlusion[5][10][11]
(a) Vasospasm
- Vasospasm due to severe postpartum hemorrhage (PPH) (loss of > 500 ml of blood during the first 24 hr), leading to hypotension and ischemic necrosis of pituitary gland, is the most common cause of Sheehan's syndrome.[5]
(b) Disseminated intravascular coagulation (DIC)
- DIC results in intravascular fibrin deposition leading to occlusion in hypophyseal portal system, thus contributing to the ischemia of pituitary gland cells.
- The pathophysiologic mechanism behind intravascular fibrin deposition is found to be similar to that of generalized Shwartzman reaction.
Autoimmunity
- It is believed that tissue necrosis results in the release of sequestered antigens, precipitating autoimmunity of the pituitary gland and hypopituitarism in Sheehan's syndrome.[12][13][14]
| DIC‡ | Severe PPH† | Glandular hypertrophy and hyperplasia | Small sella size | Autoimmunity | |||||||||||||||||||||||||||||||||||||||||||||
| Hypotension/Shock | Pituitary enlargement | Pituitary compression | |||||||||||||||||||||||||||||||||||||||||||||||
| Blood supply compression | |||||||||||||||||||||||||||||||||||||||||||||||||
| Ischemic necrosis | |||||||||||||||||||||||||||||||||||||||||||||||||
| Hypopituitarism | |||||||||||||||||||||||||||||||||||||||||||||||||
| Amenorrhea | Agalactorrhea | Secondary adrenal insufficiency | Hypothyroidism | ||||||||||||||||||||||||||||||||||||||||||||||
‡Disseminated intravascular coagulation (DIC) due to Amniotic fluid embolism or HELLP Syndrome.
†Postpartum hemorrhage (PPH) i.e., >500 ml after vaginal delivery or 1000 ml after C-section.
Genetics
There is no genetic association found to be associated with Sheehan's syndrome.
Associated Conditions
Sheehan's syndrome is associated with:[15]
- Pregnancy
- PPH
- Type 1 diabetes
- Pre-existing vascular diseases such as thrombosis and DIC
- Hypotension
Gross Pathology
- On gross pathology, pituitary gland sequentialy changes from an enlarged pituitary gland to a small shrunken or atrophic gland which is later replaced by remnants of pituitary or CSF.
Microscopic Pathology
On microscopy, the following findings may be observed:
- Ischemic necrosis leading to scarring of neurohypophysis
- Scarring of paraventricular and supraoptic nuclei
References
- ↑ Rolih CA, Ober KP (1993). "Pituitary apoplexy". Endocrinol. Metab. Clin. North Am. 22 (2): 291–302. PMID 8325288.
- ↑ Henry Gray (1918) Anatomy of the Human Body, Bartleby.com: Gray's Anatomy, Plate 721, Public Domain, <https://commons.wikimedia.org/w/index.php?curid=541543>
- ↑ Atmaca H, Tanriverdi F, Gokce C, Unluhizarci K, Kelestimur F (2007). "Posterior pituitary function in Sheehan's syndrome". Eur. J. Endocrinol. 156 (5): 563–7. doi:10.1530/EJE-06-0727. PMID 17468192.
- ↑ Vance ML (1994). "Hypopituitarism". N. Engl. J. Med. 330 (23): 1651–62. doi:10.1056/NEJM199406093302306. PMID 8043090.
- ↑ 5.0 5.1 5.2 Keleştimur F (2003). "Sheehan's syndrome". Pituitary. 6 (4): 181–8. PMID 15237929.
- ↑ Toogood AA, Beardwell CG, Shalet SM (1994). "The severity of growth hormone deficiency in adults with pituitary disease is related to the degree of hypopituitarism". Clin. Endocrinol. (Oxf). 41 (4): 511–6. PMID 7955461.
- ↑ Benvenga S, Campenní A, Ruggeri RM, Trimarchi F (2000). "Clinical review 113: Hypopituitarism secondary to head trauma". J. Clin. Endocrinol. Metab. 85 (4): 1353–61. doi:10.1210/jcem.85.4.6506. PMID 10770165.
- ↑ Kelly DF, Gonzalo IT, Cohan P, Berman N, Swerdloff R, Wang C (2000). "Hypopituitarism following traumatic brain injury and aneurysmal subarachnoid hemorrhage: a preliminary report". J. Neurosurg. 93 (5): 743–52. doi:10.3171/jns.2000.93.5.0743. PMID 11059653.
- ↑ Scheithauer BW, Sano T, Kovacs KT, Young WF, Ryan N, Randall RV (1990). "The pituitary gland in pregnancy: a clinicopathologic and immunohistochemical study of 69 cases". Mayo Clin. Proc. 65 (4): 461–74. PMID 2159093.
- ↑ McKay, Donald G.; Merrill, Samuel J.; Weiner, Albert E.; Hertig, Arthur T.; Reid, Duncan E. (1953). "The pathologic anatomy of eclampsia, bilateral renal cortical necrosis, pituitary necrosis, and other acute fatal complications of pregnancy, and its possible relationship to the generalized Shwartzman phenomenon". American Journal of Obstetrics and Gynecology. 66 (3): 507–539. doi:10.1016/0002-9378(53)90068-4. ISSN 0002-9378.
- ↑ Apitz, Kurt (September 1, 1935). "A Study of the Generalized Shwartzman Phenomenon". The Journal of Immunology. 29 (3): 255–266.
- ↑ Goswami R, Kochupillai N, Crock PA, Jaleel A, Gupta N (2002). "Pituitary autoimmunity in patients with Sheehan's syndrome". J. Clin. Endocrinol. Metab. 87 (9): 4137–41. doi:10.1210/jc.2001-020242. PMID 12213861.
- ↑ "AUTOANTIBODIES IN SHEEHAN'S SYNDROME - ScienceDirect".
- ↑ Falorni A, Minarelli V, Bartoloni E, Alunno A, Gerli R (2014). "Diagnosis and classification of autoimmune hypophysitis". Autoimmun Rev. 13 (4–5): 412–6. doi:10.1016/j.autrev.2014.01.021. PMID 24434361.
- ↑ Abourawi, F (2006). "Diabetes Mellitus and Pregnancy". Libyan Journal of Medicine. 1 (1): 28–41. doi:10.4176/060617. ISSN 1993-2820.