Secondary amyloidosis pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 12: | Line 12: | ||
*[[Amyloid]] deposition can disrupt tissue structure of involved organ and consequently leads to organ failure.<ref name="pmid267192342">{{cite journal |vauthors=Wechalekar AD, Gillmore JD, Hawkins PN |title=Systemic amyloidosis |journal=Lancet |volume=387 |issue=10038 |pages=2641–2654 |date=June 2016 |pmid=26719234 |doi=10.1016/S0140-6736(15)01274-X |url=}}</ref> | *[[Amyloid]] deposition can disrupt tissue structure of involved organ and consequently leads to organ failure.<ref name="pmid267192342">{{cite journal |vauthors=Wechalekar AD, Gillmore JD, Hawkins PN |title=Systemic amyloidosis |journal=Lancet |volume=387 |issue=10038 |pages=2641–2654 |date=June 2016 |pmid=26719234 |doi=10.1016/S0140-6736(15)01274-X |url=}}</ref> | ||
====Secondary Amyloidosis (AA)==== | ====Secondary Amyloidosis (AA)==== | ||
*[[AA amyloidosis|Secondary amyloidosis]] occurs as a reaction to an existing illness. | *[[AA amyloidosis|Secondary amyloidosis]] occurs as a reaction to an existing illness. | ||
*[[AA amyloidosis|Secondary amyloidosis]] is associated with chronic [[inflammation]] (such as [[tuberculosis]] or [[rheumatoid arthritis]]).<ref name="pmid116772762">{{cite journal |vauthors=Khan MF, Falk RH |title=Amyloidosis |journal=Postgrad Med J |volume=77 |issue=913 |pages=686–93 |date=November 2001 |pmid=11677276 |pmc=1742163 |doi= |url=}}</ref> | *[[AA amyloidosis|Secondary amyloidosis]] is associated with chronic [[inflammation]] (such as [[tuberculosis]] or [[rheumatoid arthritis]]).<ref name="pmid116772762">{{cite journal |vauthors=Khan MF, Falk RH |title=Amyloidosis |journal=Postgrad Med J |volume=77 |issue=913 |pages=686–93 |date=November 2001 |pmid=11677276 |pmc=1742163 |doi= |url=}}</ref> | ||
| Line 28: | Line 24: | ||
**[[Protease|Proteases]] | **[[Protease|Proteases]] | ||
== Associated Conditions == | == Associated Conditions == | ||
Conditions associated with amyloidosis include:<ref name=" | * Conditions associated with AA amyloidosis include:<ref name="BlankHegenbart2018">{{cite journal|last1=Blank|first1=Norbert|last2=Hegenbart|first2=Ute|last3=Dietrich|first3=Sascha|last4=Brune|first4=Maik|last5=Beimler|first5=Jörg|last6=Röcken|first6=Christoph|last7=Müller-Tidow|first7=Carsten|last8=Lorenz|first8=Hanns-Martin|last9=Schönland|first9=Stefan O.|title=Obesity is a significant susceptibility factor for idiopathic AA amyloidosis|journal=Amyloid|volume=25|issue=1|year=2018|pages=37–45|issn=1350-6129|doi=10.1080/13506129.2018.1429391}}</ref><ref name="van der HilstYamada2008">{{cite journal|last1=van der Hilst|first1=J. C. H.|last2=Yamada|first2=T.|last3=Op den Camp|first3=H. J. M.|last4=van der Meer|first4=J. W. M.|last5=Drenth|first5=J. P. H.|last6=Simon|first6=A.|title=Increased susceptibility of serum amyloid A 1.1 to degradation by MMP-1: potential explanation for higher risk of type AA amyloidosis|journal=Rheumatology|volume=47|issue=11|year=2008|pages=1651–1654|issn=1462-0324|doi=10.1093/rheumatology/ken371}}</ref><ref name="PapaDoglio2017">{{cite journal|last1=Papa|first1=Riccardo|last2=Doglio|first2=Matteo|last3=Lachmann|first3=Helen J.|last4=Ozen|first4=Seza|last5=Frenkel|first5=Joost|last6=Simon|first6=Anna|last7=Neven|first7=Bénédicte|last8=Kuemmerle-Deschner|first8=Jasmin|last9=Ozgodan|first9=Huri|last10=Caorsi|first10=Roberta|last11=Federici|first11=Silvia|last12=Finetti|first12=Martina|last13=Trachana|first13=Maria|last14=Brunner|first14=Jurgen|last15=Bezrodnik|first15=Liliana|last16=Pinedo Gago|first16=Mari Carmen|last17=Maggio|first17=Maria Cristina|last18=Tsitsami|first18=Elena|last19=Al Suwairi|first19=Wafaa|last20=Espada|first20=Graciela|last21=Shcherbina|first21=Anna|last22=Aksu|first22=Guzide|last23=Ruperto|first23=Nicolino|last24=Martini|first24=Alberto|last25=Ceccherini|first25=Isabella|last26=Gattorno|first26=Marco|title=A web-based collection of genotype-phenotype associations in hereditary recurrent fevers from the Eurofever registry|journal=Orphanet Journal of Rare Diseases|volume=12|issue=1|year=2017|issn=1750-1172|doi=10.1186/s13023-017-0720-3}}</ref> | ||
* | ** Monogenic [[Periodic fever syndrome|periodic fever syndromes]], such as: | ||
***[[FMF]] | |||
***[[TNF receptor associated periodic syndrome|TNF Receptor associated periodic syndrome]] ([[TRAPS]]) | |||
***[[CAPS|Cryopyrin-associated periodic fever syndrome]] | |||
***[[Mevalonate kinase deficiency]] | |||
**[[Tuberculosis]] | |||
**[[Leprosy]] | |||
** Whipple Disease | |||
**[[Osteomyelitis]] | |||
**[[Chronic pyelonephritis]] | |||
**[[Subacute bacterial endocarditis]] | |||
** Chronic cutaneous ulcers | |||
**[[Conditions]] Predisposing to chronic [[infections]] including: | |||
***[[Cystic fibrosis]] | |||
***[[Bronchiectasis]] | |||
***[[Kartagener syndrome]] | |||
***[[Epidermolysis bullosa]] | |||
***Injected drug abuse | |||
***[[Jejuno-ileal bypass]] | |||
***[[Paraplegia]] | |||
***[[Sickle cell anemia]] | |||
***[[Immunodeficiency]] | |||
***[[Common variable immunodeficiency]] | |||
***[[Cyclic neutropenia]] | |||
***[[Hyperimmunoglobulin M syndrome]] | |||
***[[Hypogammaglobulinemia]] | |||
*** Sex-linked agammaglobulinemia | |||
***[[Human Immunodeficiency Virus|Human immunodeficiency virus]]/[[AIDS]] | |||
**[[Neoplasia]] | |||
**[[Adenocarcinoma]] | |||
**[[Basal cell carcinoma]] | |||
**[[Carcinoid tumors|Carcinoid tumor]] | |||
**[[Castleman disease]] | |||
**[[Gastrointestinal stromal tumor]] | |||
**[[Hairy cell leukemia]] | |||
**[[Hepatic adenoma]] | |||
**[[Hodgkin disease]] | |||
**[[Mesothelioma]] | |||
**[[Renal cell carcinoma]] | |||
**[[Sarcoma]] | |||
**Inflammatory Arthritis | |||
** Adult-onset Still disease | |||
**[[Ankylosing spondylitis]] | |||
**[[Juvenile idiopathic arthritis]] | |||
**[[Psoriatic arthropathy]] | |||
**[[Reiter's syndrome|Reiter syndrome]] | |||
**[[Rheumatoid arthritis]] | |||
**[[Gout]] | |||
** Systemic [[Vasculitis]] | |||
** Antineutrophil cytoplasmic antibody-associated vasculitis | |||
**[[Behcet disease]] | |||
**[[Giant cell arteritis]] | |||
**[[Polyarteritis nodosa]] | |||
**[[Polymyalgia rheumatica]] | |||
**[[Systemic lupus erythematosus]] | |||
**[[Takayasu arteritis]] | |||
**[[Inflammatory Bowel Disease]] | |||
**[[Ulcerative colitis]] | |||
**[[Crohn disease]] | |||
* Others include: | |||
**[[Atrial myxoma]] | |||
** Inflammatory abdominal aortic aneurism | |||
**[[Retroperitoneal fibrosis]] | |||
**[[SAPHO syndrome|SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis) syndrome]] | |||
**[[Sarcoidosis]] | |||
**[[Sinus histiocytosis with massive lymphadenopathy]] | |||
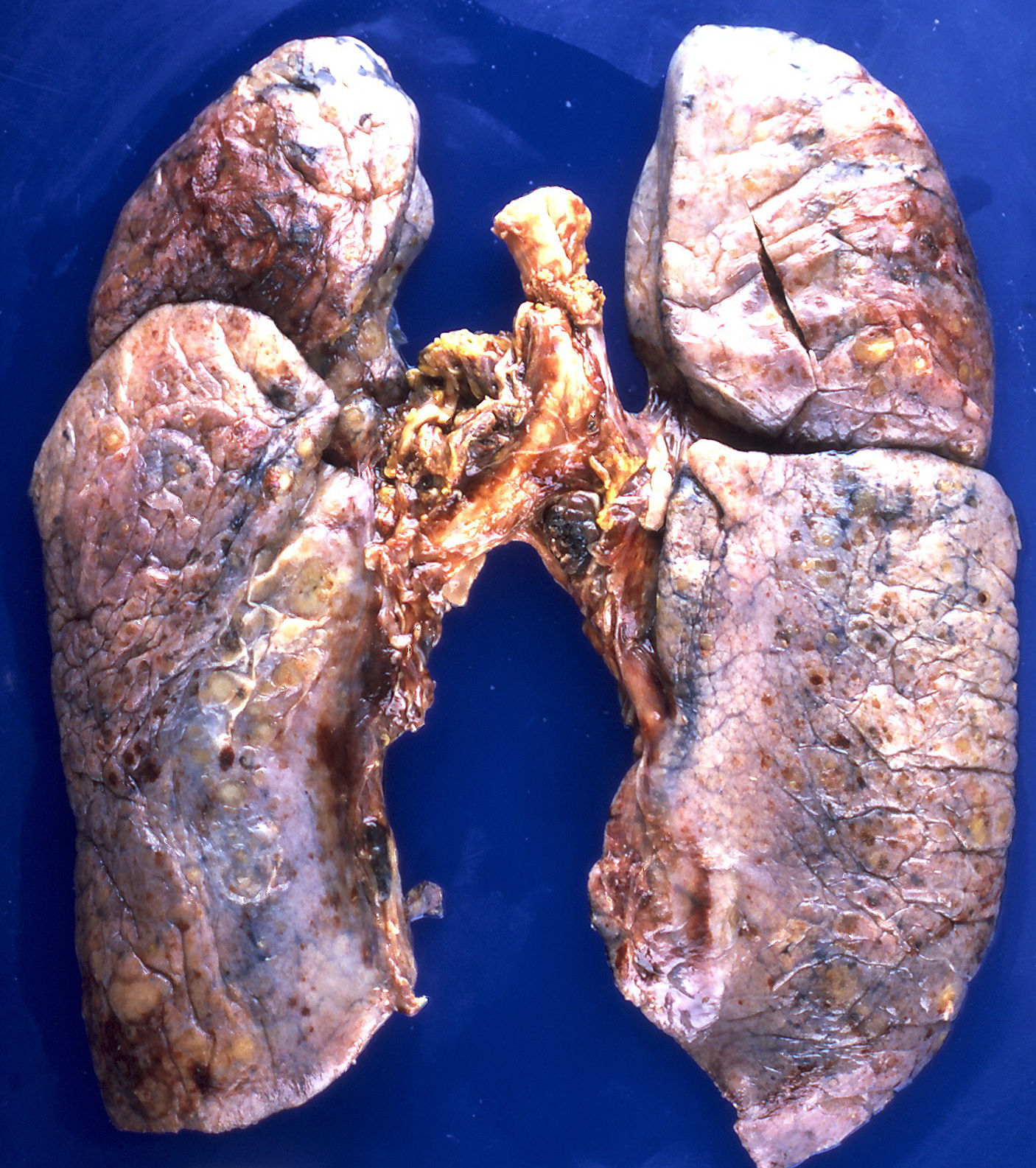
== Gross Pathology == | == Gross Pathology == | ||
On gross pathology, the organs affected by amyloidosis can be characterized by the following features: | On gross pathology, the organs affected by amyloidosis can be characterized by the following features: | ||
Revision as of 19:33, 31 October 2019
|
Secondary amyloidosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Secondary amyloidosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Secondary amyloidosis pathophysiology |
|
Risk calculators and risk factors for Secondary amyloidosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Shaghayegh Habibi, M.D.[2]Sabawoon Mirwais, M.B.B.S, M.D.[3]
Overview
Amyloid is an abnormal insoluble extracellular protein that deposits in the different tissues and causes organic dysfunction and a wide variety of clinical syndromes. In systemic amyloidosis, amyloid gradually accumulate and amyloid deposition is widespread in the viscera, blood vessel walls, and in the different connective tissues. Secondary amyloidosis is associated with chronic inflammation (such as tuberculosis or rheumatoid arthritis).
Pathophysiology
- Amyloid is an abnormal insoluble extracellular protein that deposits in the different tissues and causes organic dysfunction and a wide variety of clinical syndromes.[1]
- These abnormal amyloids are derived from misfolding and aggregation of normally soluble proteins.
- Amyloid deposition can disrupt tissue structure of involved organ and consequently leads to organ failure.[2]
Secondary Amyloidosis (AA)
- Secondary amyloidosis occurs as a reaction to an existing illness.
- Secondary amyloidosis is associated with chronic inflammation (such as tuberculosis or rheumatoid arthritis).[3]
- Secondary or reactive amyloidosis (AA) comprises approximately 45% of the systemic amyloidoses.
- Pathogenesis of secondary amyloidosis is multifactorial, including:
- Primary structure of the precursor protein
- Acute phase response
- Nonfibril proteins (amyloid P component, apo E, GAGs, proteoglycans and basement membrane proteins)
- Receptors
- Lipid metabolism
- Proteases
Associated Conditions
- Conditions associated with AA amyloidosis include:[4][5][6]
- Monogenic periodic fever syndromes, such as:
- Tuberculosis
- Leprosy
- Whipple Disease
- Osteomyelitis
- Chronic pyelonephritis
- Subacute bacterial endocarditis
- Chronic cutaneous ulcers
- Conditions Predisposing to chronic infections including:
- Cystic fibrosis
- Bronchiectasis
- Kartagener syndrome
- Epidermolysis bullosa
- Injected drug abuse
- Jejuno-ileal bypass
- Paraplegia
- Sickle cell anemia
- Immunodeficiency
- Common variable immunodeficiency
- Cyclic neutropenia
- Hyperimmunoglobulin M syndrome
- Hypogammaglobulinemia
- Sex-linked agammaglobulinemia
- Human immunodeficiency virus/AIDS
- Neoplasia
- Adenocarcinoma
- Basal cell carcinoma
- Carcinoid tumor
- Castleman disease
- Gastrointestinal stromal tumor
- Hairy cell leukemia
- Hepatic adenoma
- Hodgkin disease
- Mesothelioma
- Renal cell carcinoma
- Sarcoma
- Inflammatory Arthritis
- Adult-onset Still disease
- Ankylosing spondylitis
- Juvenile idiopathic arthritis
- Psoriatic arthropathy
- Reiter syndrome
- Rheumatoid arthritis
- Gout
- Systemic Vasculitis
- Antineutrophil cytoplasmic antibody-associated vasculitis
- Behcet disease
- Giant cell arteritis
- Polyarteritis nodosa
- Polymyalgia rheumatica
- Systemic lupus erythematosus
- Takayasu arteritis
- Inflammatory Bowel Disease
- Ulcerative colitis
- Crohn disease
- Others include:
- Atrial myxoma
- Inflammatory abdominal aortic aneurism
- Retroperitoneal fibrosis
- SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis) syndrome
- Sarcoidosis
- Sinus histiocytosis with massive lymphadenopathy
Gross Pathology
On gross pathology, the organs affected by amyloidosis can be characterized by the following features:
- Porcelain like or waxy appearance
- Enlargement
Images


Microscopic Pathology
On microscopic histopathological analysis, amyloidosis is characterized by:[3][10]
- Green birefringence under polarized light after Congo red staining (appears red under normal light)
- Linear non-branching fibrils (indefinite length with an approximately same diameter)
- Distinct X-ray diffraction pattern consistent with Pauling's model of a cross-beta fibril
Images



References
- ↑ Wechalekar AD, Gillmore JD, Hawkins PN (June 2016). "Systemic amyloidosis". Lancet. 387 (10038): 2641–2654. doi:10.1016/S0140-6736(15)01274-X. PMID 26719234.
- ↑ Wechalekar AD, Gillmore JD, Hawkins PN (June 2016). "Systemic amyloidosis". Lancet. 387 (10038): 2641–2654. doi:10.1016/S0140-6736(15)01274-X. PMID 26719234.
- ↑ 3.0 3.1 Khan MF, Falk RH (November 2001). "Amyloidosis". Postgrad Med J. 77 (913): 686–93. PMC 1742163. PMID 11677276.
- ↑ Blank, Norbert; Hegenbart, Ute; Dietrich, Sascha; Brune, Maik; Beimler, Jörg; Röcken, Christoph; Müller-Tidow, Carsten; Lorenz, Hanns-Martin; Schönland, Stefan O. (2018). "Obesity is a significant susceptibility factor for idiopathic AA amyloidosis". Amyloid. 25 (1): 37–45. doi:10.1080/13506129.2018.1429391. ISSN 1350-6129.
- ↑ van der Hilst, J. C. H.; Yamada, T.; Op den Camp, H. J. M.; van der Meer, J. W. M.; Drenth, J. P. H.; Simon, A. (2008). "Increased susceptibility of serum amyloid A 1.1 to degradation by MMP-1: potential explanation for higher risk of type AA amyloidosis". Rheumatology. 47 (11): 1651–1654. doi:10.1093/rheumatology/ken371. ISSN 1462-0324.
- ↑ Papa, Riccardo; Doglio, Matteo; Lachmann, Helen J.; Ozen, Seza; Frenkel, Joost; Simon, Anna; Neven, Bénédicte; Kuemmerle-Deschner, Jasmin; Ozgodan, Huri; Caorsi, Roberta; Federici, Silvia; Finetti, Martina; Trachana, Maria; Brunner, Jurgen; Bezrodnik, Liliana; Pinedo Gago, Mari Carmen; Maggio, Maria Cristina; Tsitsami, Elena; Al Suwairi, Wafaa; Espada, Graciela; Shcherbina, Anna; Aksu, Guzide; Ruperto, Nicolino; Martini, Alberto; Ceccherini, Isabella; Gattorno, Marco (2017). "A web-based collection of genotype-phenotype associations in hereditary recurrent fevers from the Eurofever registry". Orphanet Journal of Rare Diseases. 12 (1). doi:10.1186/s13023-017-0720-3. ISSN 1750-1172.
- ↑ By Yale Rosen from USA - Amyloidosis, CC BY-SA 2.0, https://commons.wikimedia.org/w/index.php?curid=31127928
- ↑ By Ed Uthman, MD - https://www.flickr.com/photos/euthman/377537238/, CC BY-SA 2.0, https://commons.wikimedia.org/w/index.php?curid=1629764
- ↑ By Ed Uthman, MD - https://www.flickr.com/photos/euthman/377538012/, CC BY-SA 2.0, https://commons.wikimedia.org/w/index.php?curid=1629740
- ↑ Röcken C, Shakespeare A (February 2002). "Pathology, diagnosis and pathogenesis of AA amyloidosis". Virchows Arch. 440 (2): 111–122. doi:10.1007/s00428-001-0582-9. PMID 11964039.
- ↑ By Michael Feldman, MD, PhDUniversity of Pennsylvania School of Medicine - http://www.healcentral.org/healapp/showMetadata?metadataId=38717, CC BY 2.0, https://commons.wikimedia.org/w/index.php?curid=870218
- ↑ By Ed Uthman, MD - https://www.flickr.com/photos/euthman/377559787/, CC BY-SA 2.0, https://commons.wikimedia.org/w/index.php?curid=1629716
- ↑ By Ed Uthman, MD - https://www.flickr.com/photos/euthman/377559955/, CC BY-SA 2.0, https://commons.wikimedia.org/w/index.php?curid=1629705