Second degree AV block
| Second degree AV block | |
| Second degree AV block. Mobitz Type II |
|
Second degree AV block Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Second degree AV block On the Web |
|
American Roentgen Ray Society Images of Second degree AV block |
|
Risk calculators and risk factors for Second degree AV block |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Electrocardiographic Findings
Type I Second Degree AV Block
- Also called the Wenckebach phenomenon or Mobitz type I block
- Intermittent failure of the supraventricular impulse to be conducted to the ventricles, not every P wave is followed by a QRS
- There is progressive prolongation of the PR interval until a P wave is blocked
- Progressive shortening of the RR interval until a P wave is blocked
- The RR interval containing the blocked P wave is shorter than the sum of 2 PP intervals
- The increase in the PR interval is longest in the second conducted beat after the pause
- These rules may not be followed because of fluctuation in vagal tone and secondary to sinus arrhythmia.
- In patients with normal QRS width, the block is usually located in the AV node
- there is progressive prolongation of the AH interval until the blocked P wave occurs
- When it is associated with bundle branch block, the block may occur in the AV node, His bundle or the contralateral bundle branch
- in 75% the block is in the AV node
- in 25% it is infranodal
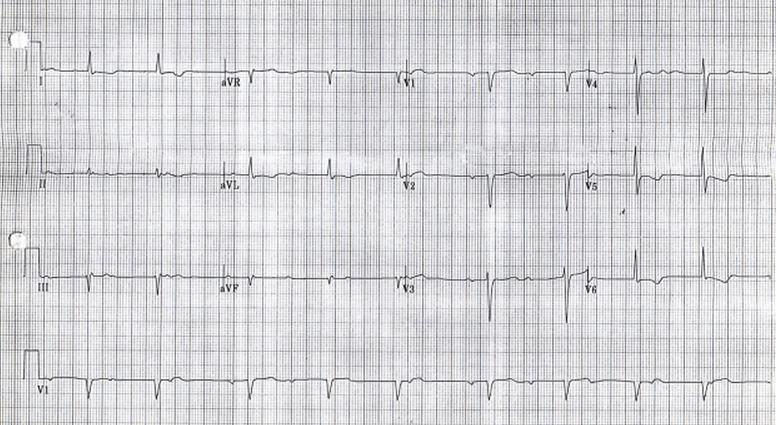
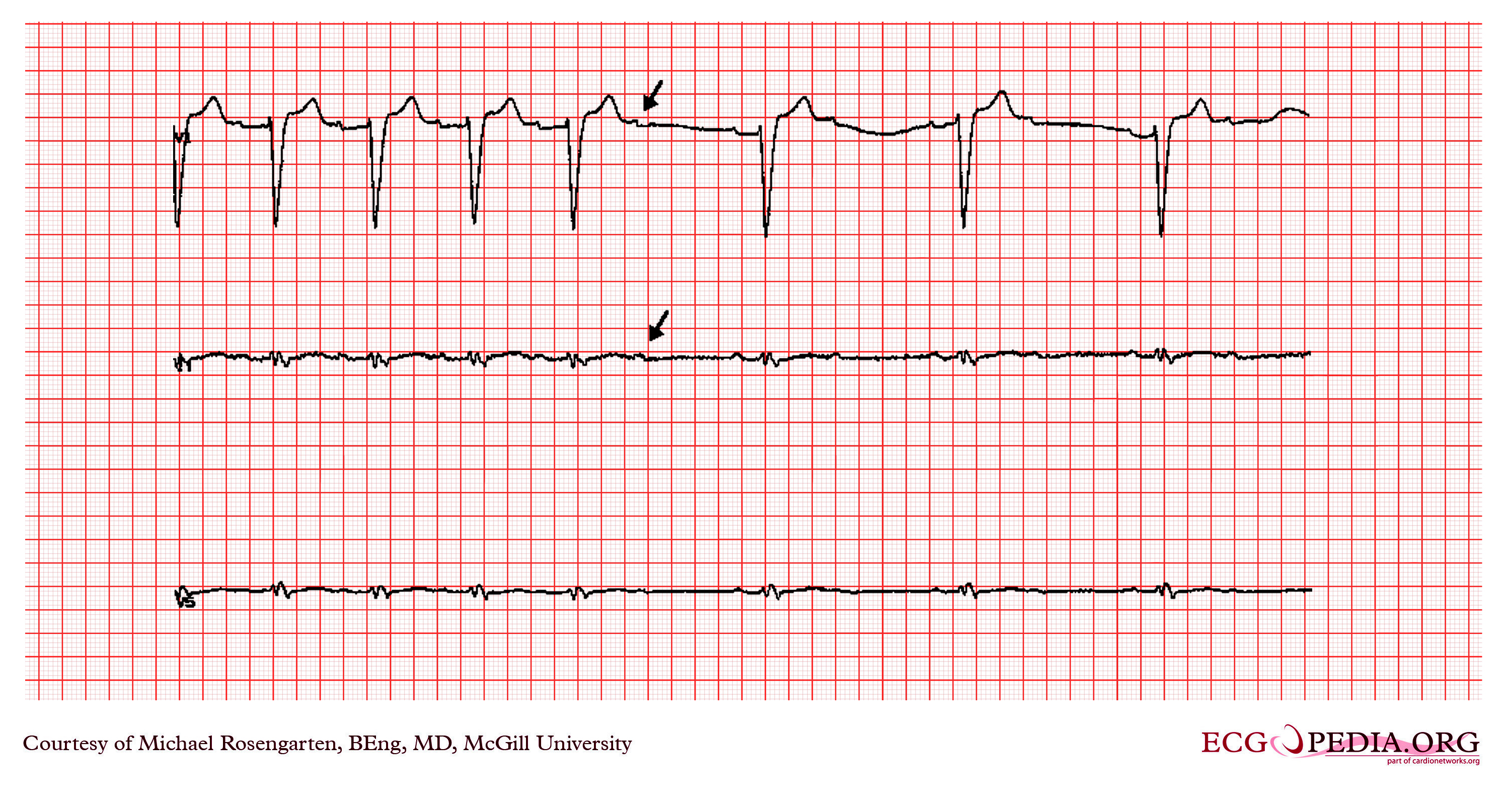
Shown below is a two lead rhythm strip from a patient in the emergency room. The rhythm is sinus with second degree A/V block. Note the progressive lengthening of the PR interval and that the interval that brackets the blocked P wave is less than twice that of the RR interval. This recording suggests a Mobitz I A/V block, but some care has to be taken as the QRS that ends the pause in at least one case looks like a nodal escape beat.
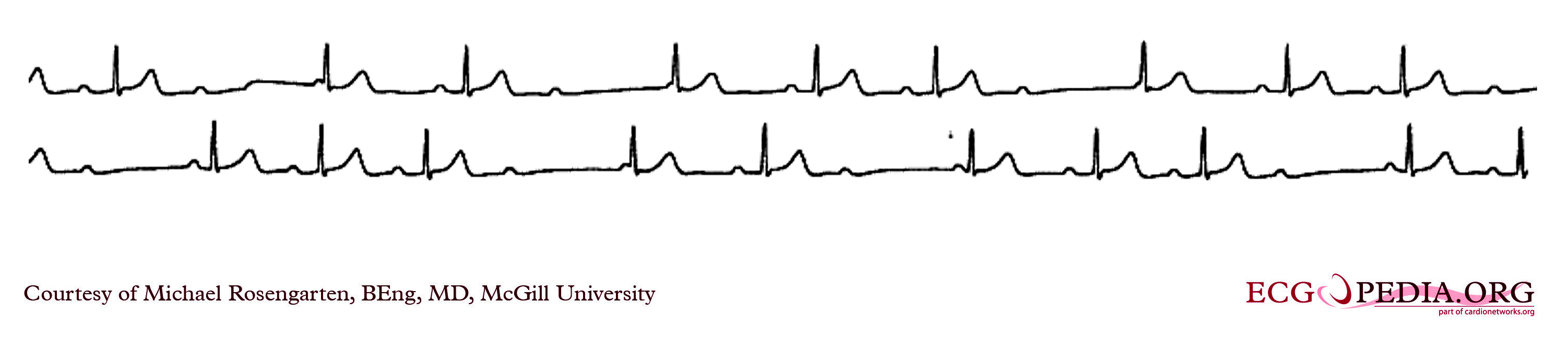
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an image of an electrocardiogram showing type I second degree AV block (Wenckebach).
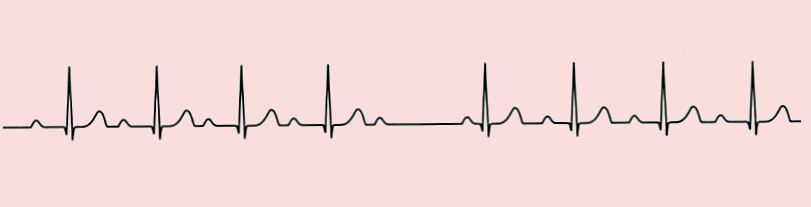
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram showing type I second degree AV block (Wenckebach).
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram showing type I second degree AV block (Wenckebach).
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram showing type I second degree AV block (Wenckebach).
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram showing a Mobitz I A/V block with a gradual increase in the PR interval before the dropped p wave
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/Main_Page
Type II Second-Degree AV Block: Mobitz Type II Block
- There are intermittent blocked P waves
- In the conducted beats, the PR intervals remain constant
- The PR is fairly constant except that slight shortening may occur in the first beat after the blocked cycle. This is the result of improved conduction following the block
- Most patients with type II second-degree AV block have associated bundle branch block.
- In these instances the block is usually located distal to the His bundle, in approximately 27 to 35% of patients however, the lesion is located in the His bundle itself, and a narrow complex may be inscribed.
- 2:1 AV Block:
- Impossible to determine whether the second-degree AV block is type I or type II.
- A long rhythm strip is helpful to document any change in the behavior of the conduction ratio
- When the atrial rate is increased by exercise or by atropine, the AV block in type I tends to decrease and that in type II tends to increase
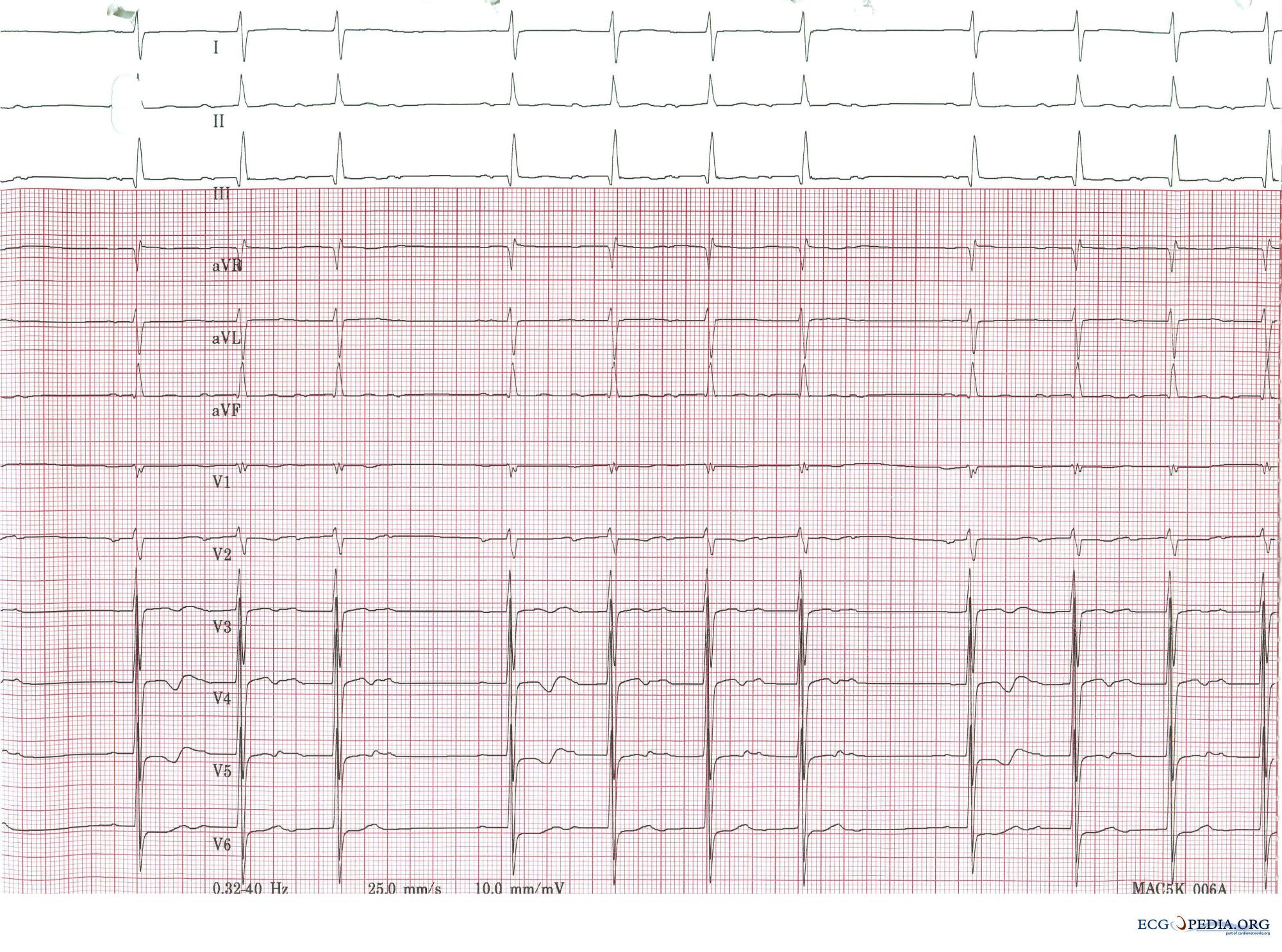
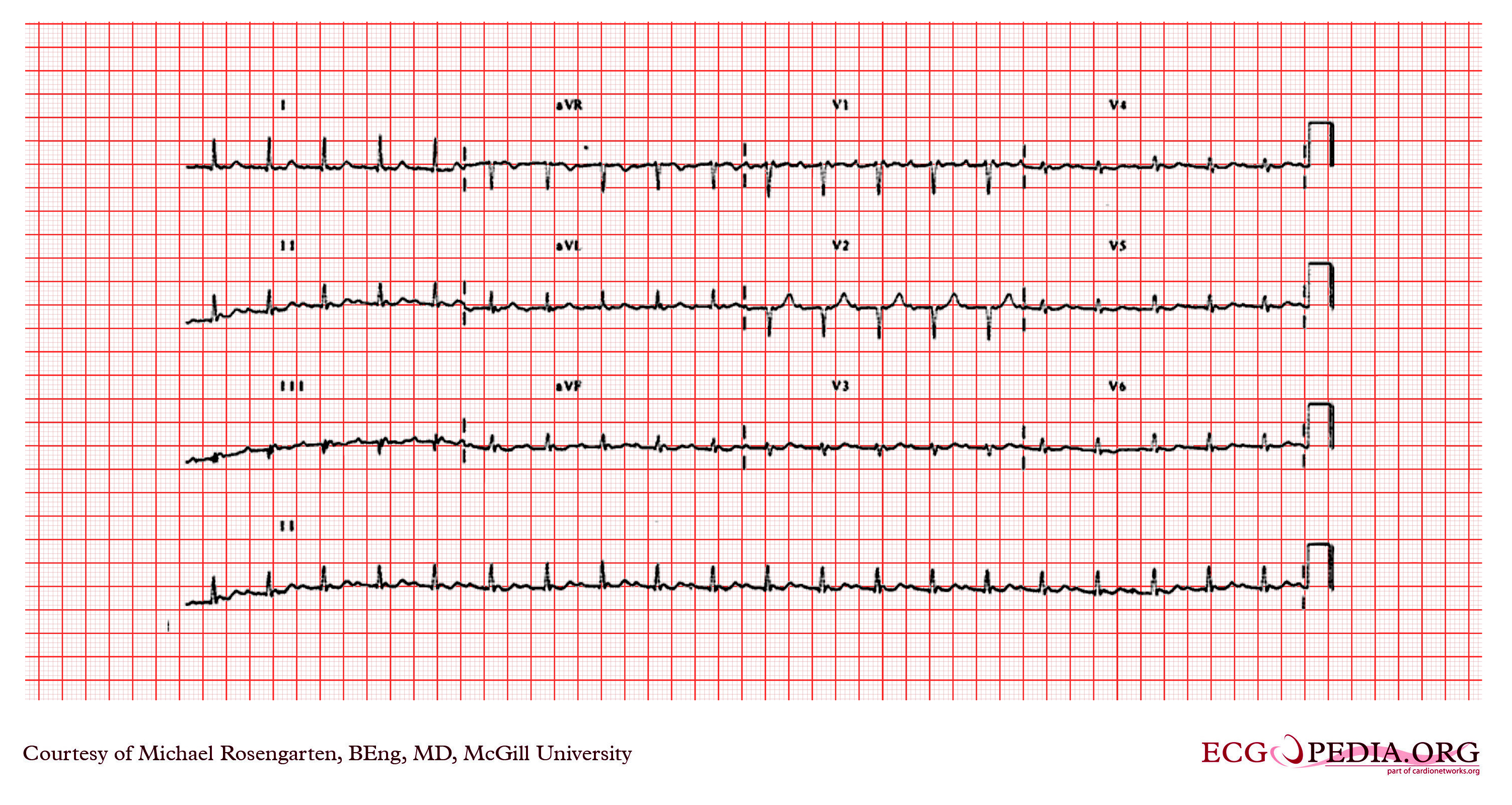
Shown below is an electrocardiogram of a 12 lead EKG with a 2:1 AV block.
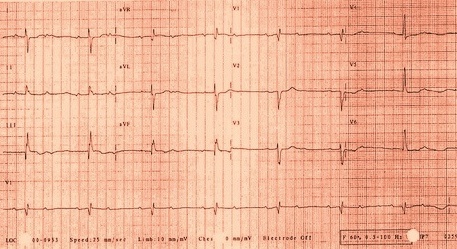
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
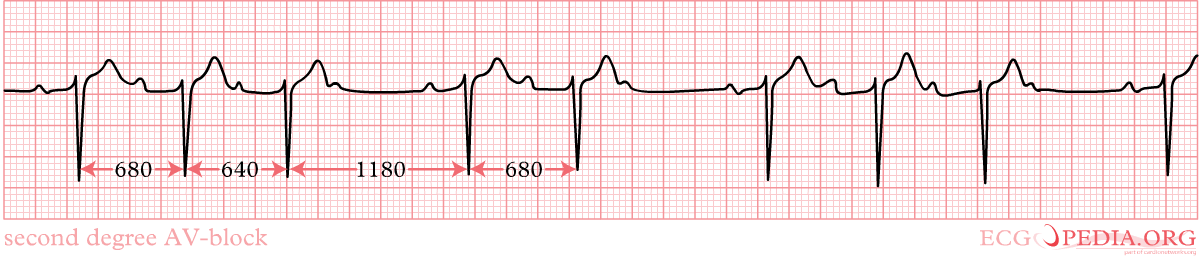
Shown below is an electrocardiogram of a type II second degree AV block (Mobitz type II).
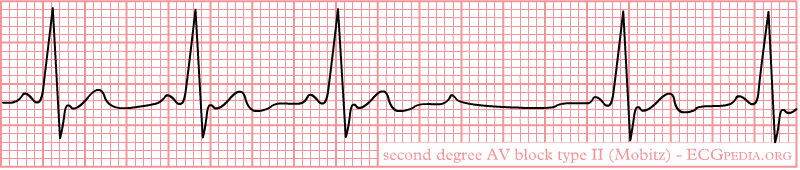
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram of a 3 channel recording with a 2:1 AV block in a 73 year old woman with dizziness. 2 to 1 AV block (every other P wave is conducted to the ventricles) 2 to 1 AV block starts after the 5th QRS in this 3 channel recording. The first non-conducted P wave is indicated with an arrow. Note the long PR interval of conducted P waves is constant and the left bundle branch block 2 to 1 AV block cannot be classified into Mobitz type I or II as we do not know if the 2nd P wave would be conducted with the same or longer PR interval.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an electrocardiogram of a 2:1 AV Block with atrial tachycardia.
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
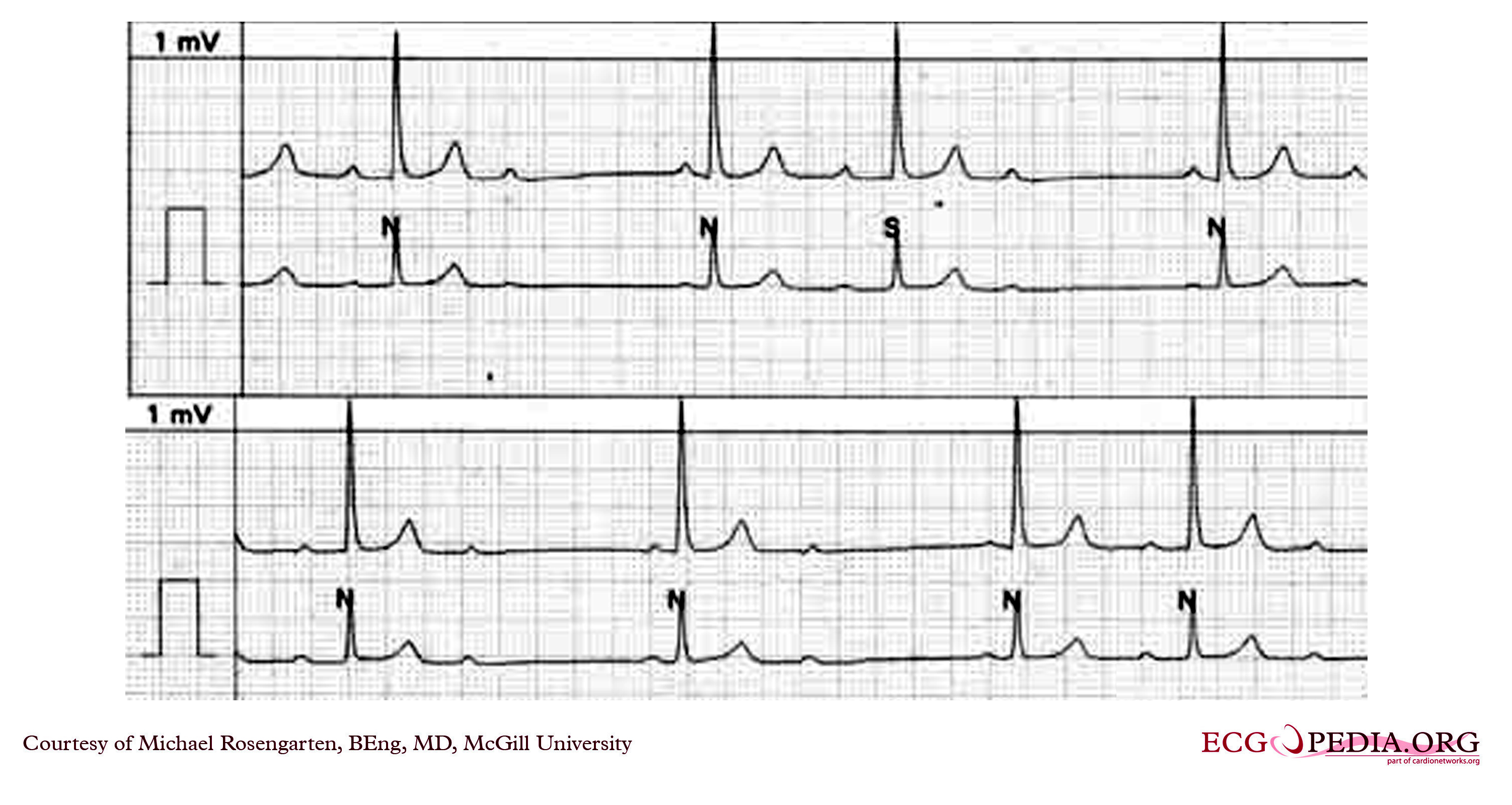
Shown below is an example of EKG showing two strips from the same patient with a 2:1 block on the top tracing and a Mobitz II A/V block on the lower one. Note that with 2:1 block you cannot tell if this is a Mobitz I or II. Mobitz II is seen below as the PR does not change before and after the non-conducted P wave.
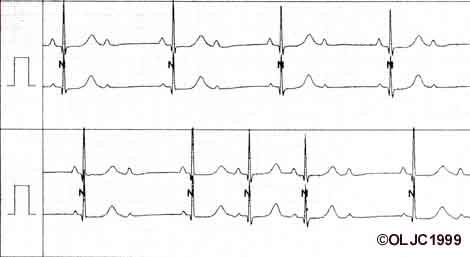
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Advanced AV Block or High Grade AV Block
- When the AV conduction ratio is 3:1 or higher
- In some cases only occasional ventricular captures are observed, and the dominant rhythm is maintained by a subsidiary pacemaker.
- You must compare the PR interval of the rare captured beats, a constant PR interval suggests type II block
Differential Diagnosis of AV Block
Differential Diagnosis of Second-Degree AV Block
- Second Degree AV Block may be simulated by blocked PACs. Must be very careful to assure that the P to P intervals are constant
- 2:1 conduction may simulate sinus bradycardia as the blocked P waves may fall on the preceding T waves
Differential Diagnosis of AV Block in General
Normal Variants
- PR prolongation can be found in 0.5% of healthy patients
- Second degree block type I may be seen in healthy patients during sleep
- Transient AV block can occur with vagal maneuvers
ST Elevation MI
- In acute ST elevation MI:
- First degree block occurs in 8% to 13%
- Second degree block in 3.5% to 10%
- Complete heart block in 2.5% to 8%
Inferior ST Elevation MI
- In 90% of patients the inferior wall is supplied by the RCA which gives off a branch to the AV node
- As a rule the AV block is transient and normal function returns within a week of the acute episode
Anterior ST Elevation MI
- Incidence of second degree AV block and third degree AV block is 5 to 7%
- Block is the result of damage to the interventricular septum supplied by the LAD
- There is damage to the bundle branches either in the form of bilateral bundle branch block or trifascicular block
- RBBB, RBBB + LAHB, RBBB + LPHB or LBBB often appear before the development of AV block
- The PR is normal or minimally prolonged before the onset of second degree AV block or third degree AV block
- Although the AV block is usually transient, there is a relatively high incidence of recurrence or high-degree AV block after the acute event
- In addition to ischemia, fibrosis and calcification of the summit of the ventricular septum that involve the branching part of the bundle branches, may play a role in the genesis of the conduction defect.
- It used to be thought that CAD was the most frequent cause of chronic complete AV block, but it actually causes only 15% of cases
Degenerative Diseases
- Sclerodegenerative disease of the bundle branches first described by Lenegre
- The pathologic process is called idiopathic bilateral bundle branch fibrosis and the heart block is called primary heart block
- This is the most common cause of chronic AV block (46%)
- Lev described similar degenerative lesions, which he referred to as sclerosis of the left side of the cardiac skeleton. There is progressive fibrosis and calcification of the mitral annulus, the central fibrous body, the pars membranacea, the base of the aorta, and the summit of the muscular ventricular septum. Various portions of the His bundle or the bundle branches may be involved, resulting in AV block.
Hypertension
- Chronic AV block in patients with HTN is thought to be due to CAD or sclerosis of the left side of the cardiac skeleton exacerbated by hypertension
Diseases of the Myocardium
- Acute rheumatic fever: PR prolongation is a common (25 to 95% of cases) sign in patients with acute rheumatic fever
- Type I second degree AV block may occur, but complete AV block is uncommon
- usually transient, disappears when the patient recovers
- Amyloidosis
- Ankylosing spondylitis
- Chagas disease
- Dermatomyositis
- Dilated cardiomyopathy results in various degrees of heart block are seen in 15% of patients
- Diphtheria
- HCM: 3% of patients with HCM will develop heart block
- Hemochromatosis
- Lyme disease
- Muscular dystrophy
- Myocarditis
- Sarcoid
- Scleroderma
- SLE
- Tumors, primary and secondary
Valvular Heart Disease
- Calcific aortic stenosis may be accompanied by chronic partial or complete AV block
- There is an extension of the calcification to involve the main bundle or its bifurcation, resulting in degeneration and necrosis of the conduction tissue
- May also occur in rheumatic mitral valve disease, but is less common
- Occasionally, massive calcification of the mitral annulus as an aging process may cause AV block
- May also be seen in bacterial endocarditis, especially of the aortic valve
Drugs
- When second degree AV block is induced, it is always of the Type I variety
- When complete block occurs, the QRS complexes are narrow because the block is of the AV node
- The ventricular response rate is more rapid than that due to organic lesions, and increased automaticity of the AV junctional pacemaker may be responsible.
- Quinidine and Procainamide may produce slight prolongation of the PR
- β blockers may cause AV block
- Diltiazem and verapamil may cause AV conduction delay and PR interval prolongation
Congenital
- Occurs in the absence of other evidence of organic heart disease
- Site is usually proximal to the bifurcation of the His bundle, most often in the AV node
- Narrow QRS with a rate > 40 beats per minute
- Frequently seen in those with corrected transposition of the great vessels, and occasionally in ASDs and Ebstein's anomaly
Trauma
- May be induced during open heart surgery in the area of AV conduction tissue
- Seen in patients operated on for the correction of VSD, tetralogy of Fallot, and endocardial cushion defect.
- May be due to edema, transient ischemia, or actual disruption of the conduction tissue. The block may therefore be permanent or transient.
- Also reported with both penetrating and non-penetrating trauma of the chest
History and Symptoms
Most people with Wenckebach (Type I Mobitz) do not show symptoms. However, those that do usually display one or more of the following:
Treatment
Mobitz I
- Patients are usually asymptomatic and doesn't require a pacemaker.
- Correction of reversible causes of the block such as ischemia, medications, and vagotonic conditions should be addressed.
Mobitz II
- Correction of reversible causes of the block such as ischemia, medications, and vagotonic conditions should be considered.
- Implantation of permanent pacemakers in both asymptomatic and symptomatic patients is usually done. Asymptomatic Mobitz II are prone to be converted to symptomatic or third degree heart AV block. Thus, they should be considered for a pacemaker even if asymptomatic.
- A dual chamber DDD pacemaker is preferred over a single chambered VVI pacemakers as it maintains physiologic AV synchrony.
- A dual-chamber artificial pacemaker is a type of device that typically listens for a pulse from the SA node and sends a pulse to the AV node at an appropriate interval, essentially completing the connection between the two nodes. Pacemakers in this role are usually programmed to enforce a minimum heart rate and to record instances of atrial flutter and atrial fibrillation
- Treatment may also include medicines to control blood pressure and atrial fibrillation, as well as lifestyle and dietary changes to reduce risk factors associated with heart attack and stroke.
- Treatment in emergency situations are atropine and an external pacer.
Related chapters
- Electrical conduction system of the heart
- Electrocardiogram (ECG or EKG)
- SA node
- AV node
- First degree AV block
- Third degree AV block
Sources
- Copyleft images obtained courtesy of ECGpedia, http://en.ecgpedia.org/index.php?title=Special:NewFiles&dir=prev&offset=20080806182927&limit=500
- Template:WhoNamedIt
- http://www.youtube.com/watch?v=GVxJJ2DBPiQ - AV Block Parody Video by the University of Alberta
- Emergency Cardiovascular Medicine - eMedicine article on 2nd Degree Heart Block