Sandbox:farnaz: Difference between revisions
Usama Talib (talk | contribs) |
No edit summary |
||
| (17 intermediate revisions by 2 users not shown) | |||
| Line 19: | Line 19: | ||
{{familytree | D001 | | D002 | | D003 | | | |D004 | | D005 | | D006 | | | | | |!| | | | | |D001=LV failure|D002=Dysrthmia|D003=LV hypertrophy and cardiomyopathy| D004=Volume Overload|D005=MI|D006=LV outflow obstruction| |}} | {{familytree | D001 | | D002 | | D003 | | | |D004 | | D005 | | D006 | | | | | |!| | | | | |D001=LV failure|D002=Dysrthmia|D003=LV hypertrophy and cardiomyopathy| D004=Volume Overload|D005=MI|D006=LV outflow obstruction| |}} | ||
{{familytree | | | | | | | | | | | | | | | | |,|-|-|-|-|-|-|-|-|-|-|-|-|-|+|-|-|-|-|-|-|-|-|-|-|-|-|-|.|}} | {{familytree | | | | | | | | | | | | | | | | |,|-|-|-|-|-|-|-|-|-|-|-|-|-|+|-|-|-|-|-|-|-|-|-|-|-|-|-|.|}} | ||
{{familytree | | | | | | | | | | | | | | | | E02 | | | | | | | | | | | | | | {{familytree | | | | | | | | | | | | | | | | E02 | | | | | | | | | | | |E03 | | | | | | | | | | | | E04 |E01=E01|E02=Direct injury to lung|E03=Hematogenous injury to lung|E04=Lung injury plus elevated hydrostatic pressure}} | ||
{{familytree | | | | | |,|-|-|-|v|-|-|-|v|-|-|^|-|-|v|-|-|-|v|-|-|-|.| | | | | {{familytree | | | | | |,|-|-|-|v|-|-|-|v|-|-|^|-|-|v|-|-|-|v|-|-|-|.| | |!| | | | | | | | | |,|-|-|-|+|-|-|-|.| }} | ||
{{familytree | | | | | F01 | | F02 | | F03 | | | | F04 | | F05 | | F06 | | | | {{familytree | | | | | F01 | | F02 | | F03 | | | | F04 | | F05 | | F06 | |!| | | | | | | | | F07 | | F08 | | F09 | | | | | |F01=Chest trauma,pulmonary contusion|F02=Aspiration|F03=Smoke inhalation|F04=Pneumonia|F05=Oxygen toxicity|F06=Pulmonary embolism,reperfusion|F07=High altitude pulmonary edema|F08=Neurogenic pulmonary edema|F09=Reexpansion pulmonary edema}} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.| | | | | | | | | }} | |||
{{familytree | | | | | | | | | | | | | | | | | | | | | | G01 | | G02 | | G03 | | G04 | | G05 | | | | | | | | | | | | | | |G01=Sepsis|G02=Pancreatitis|G03=Nonthoracic trauma|G04=Multiple transfusions|G05=Intravenous drug use. e.g. heroin|G06=Cardiopulmonary bypass}} | |||
{{familytree/end}} | {{familytree/end}} | ||
*Direct injury to lung: | |||
**Pulmonary contusion | |||
**[[Aspiration]] | |||
**Smoke inhalation | |||
**[[Pneumonia]] | |||
**Oxygen toxicity | |||
**[[Pulmonary embolism]],[[reperfusion]] | |||
*Hematogenous injury to lung: | |||
**[[Sepsis]] | |||
**[[Pancreatitis]] | |||
**Nonthoracic trauma | |||
**Multiple transfusions | |||
**Intravenous drug use | |||
**Cardiopulmonary bypass | |||
*Lung injury plus elevated hydrostatic pressure: | |||
**High altitude pulmonary edema | |||
**Neurogenic pulmonary edema | |||
**[[Reexpansion]] [[pulmonary edema]] | |||
96 patients (174 eyes, 70% females) were included with a mean age at presentation of 30 years | |||
{{Family tree/start}} | |||
{{Family tree || | | B01 | | | |B01= Pulmonary edema treatment based on classification}} | |||
{{Family tree | |,|-|-|^|-|-|.| | }} | |||
{{Family tree | | C01 | | | | C02 |C01= Cardiogenic pulmonary edema| C02= Noncardiogenic pulmonary edema}} | |||
{{familytree | | |!| | | | | |!| | | }} | |||
{{familytree | | D01 | | | | |!| | |D01= stabilize patient }} | |||
{{Family tree/end}} | |||
{| class="wikitable" | {| class="wikitable" | ||
| Line 58: | Line 80: | ||
==References== | ==References== | ||
__NOTOC__ | |||
{{CMG}}; {{AE}} {{EG}} | |||
<small>'''''Abbreviations:''''' '''ABG ('''[[arterial blood gas]]'''); ACE ('''[[Angiotensin-converting enzyme|angiotensin converting enzyme]]'''); BMI ('''[[body mass index]]'''); CBC ('''[[Complete blood counts|complete blood count]]'''); CSF ('''[[cerebrospinal fluid]]'''); CXR ('''[[chest X-ray]]'''); ECG ('''[[electrocardiogram]]'''); FEF ('''[[Spirometry|forced expiratory flow rate]]'''); FEV1 ('''[[forced expiratory volume]]'''); FVC ('''[[forced vital capacity]]'''); JVD ('''[[jugular vein distention]]''');''' '''MCV ('''[[mean corpuscular volume]]'''); Plt ('''[[platelet]]'''); RV ('''[[residual volume]]'''); SIADH ('''[[syndrome of inappropriate antidiuretic hormone]]'''); TSH ('''[[thyroid stimulating hormone]]'''); Vt ('''[[tidal volume]]''');''' '''WBC ('''[[White blood cells|white blood cell]]''');'''</small> | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! colspan="3" rowspan="3" |Organ system | |||
! rowspan="3" |Diseases | |||
! colspan="11" |Clinical manifestations | |||
! colspan="5" rowspan="2" |Diagnosis | |||
! rowspan="3" |Other features | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! colspan="6" |Symptoms | |||
! colspan="5" |Physical exam | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
!Loss of consciousness | |||
!Agitation | |||
!Weight loss | |||
!Fever | |||
!Chest pain | |||
!Cough | |||
!Cyanosis | |||
!Clubbing | |||
!JVD | |||
!Peripheral edema | |||
!Auscultation | |||
!CBC | |||
!ABG | |||
!Imaging | |||
!Spirometry | |||
!Gold standard | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| | |||
| | |||
| | |||
![[Pulmonary edema]]<ref name="MartindaleNoble2013">{{cite journal|last1=Martindale|first1=Jennifer L.|last2=Noble|first2=Vicki E.|last3=Liteplo|first3=Andrew|title=Diagnosing pulmonary edema|journal=European Journal of Emergency Medicine|volume=20|issue=5|year=2013|pages=356–360|issn=0969-9546|doi=10.1097/MEJ.0b013e32835c2b88}}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |Basal [[Crackles|crackle]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |[[Respiratory alkalosis]] | |||
! style="background: #F5F5F5; padding: 5px;" |Bat wing pattern, air bronchograms | |||
! style="background: #F5F5F5; padding: 5px;" |↓[[Tidal volume|Vt]], ↑[[Residual volume|RV]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Coronary catheterization|Cardiac Catheterization]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Tachypnea]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
! rowspan="4" |Acute Dyspnea | |||
! rowspan="4" |[[Respiratory system]] | |||
! rowspan="4" |[[Chest]] and [[Pleurae|Pleura]], | |||
Lower [[airway]] | |||
![[Bronchiolitis]]<ref name="pmid23562737">{{cite journal |vauthors=Holbro A, Lehmann T, Girsberger S, Stern M, Gambazzi F, Lardinois D, Heim D, Passweg JR, Tichelli A, Bubendorf L, Savic S, Hostettler K, Grendelmeier P, Halter JP, Tamm M |title=Lung histology predicts outcome of bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation |journal=Biol. Blood Marrow Transplant. |volume=19 |issue=6 |pages=973–80 |year=2013 |pmid=23562737 |doi=10.1016/j.bbmt.2013.03.017 |url=}}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Wheeze]] and [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |↑[[WBC]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |Bronchovascular markings | |||
! style="background: #F5F5F5; padding: 5px;" |↓[[Tidal volume|Vt]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Clinical]] assessment | |||
! style="background: #F5F5F5; padding: 5px;" |[[Respiratory syncytial virus|Respiratory syncytial virus (RSV)]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
![[COPD exacerbation resident survival guide|COPD exacerbation]]<ref name="pmid25177479">{{cite journal| author=Qureshi H, Sharafkhaneh A, Hanania NA| title=Chronic obstructive pulmonary disease exacerbations: latest evidence and clinical implications. | journal=Ther Adv Chronic Dis | year= 2014 | volume= 5 | issue= 5 | pages= 212-27 | pmid=25177479 | doi=10.1177/2040622314532862 | pmc=4131503 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25177479 }}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Wheeze]], [[Rhonchi]], and [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |↑[[WBC]], ↑[[RBC]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Respiratory alkalosis]] | |||
! style="background: #F5F5F5; padding: 5px;" |Hyperexpansion | |||
! style="background: #F5F5F5; padding: 5px;" |↓ [[FEV1]]/[[FVC]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Clinical]] assessment | |||
! style="background: #F5F5F5; padding: 5px;" |[[Chronic bronchitis|Acute '''exacerbations''' of chronic bronchitis (AECB)]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
![[Lung carcinoma]]<ref name="pmid22054876">{{cite journal| author=Dela Cruz CS, Tanoue LT, Matthay RA| title=Lung cancer: epidemiology, etiology, and prevention. | journal=Clin Chest Med | year= 2011 | volume= 32 | issue= 4 | pages= 605-44 | pmid=22054876 | doi=10.1016/j.ccm.2011.09.001 | pmc=3864624 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22054876 }}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Wheeze]] and [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |Mass lesion, [[hilar lymphadenopathy]] | |||
! style="background: #F5F5F5; padding: 5px;" |↓[[Tidal volume|Vt]], ↑[[Residual volume|RV]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Bronchoscopy]] | |||
! style="background: #F5F5F5; padding: 5px;" |Paraneoplastic syndromes, such as [[Syndrome of inappropriate antidiuretic hormone|SIADH]] and [[Lambert-Eaton myasthenic syndrome|lambert-Eaton]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
![[Pneumonia]]<ref name="pmid25165554">{{cite journal| author=Simonetti AF, Viasus D, Garcia-Vidal C, Carratalà J| title=Management of community-acquired pneumonia in older adults. | journal=Ther Adv Infect Dis | year= 2014 | volume= 2 | issue= 1 | pages= 3-16 | pmid=25165554 | doi=10.1177/2049936113518041 | pmc=4072047 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25165554 }}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Wheeze]], [[Rhonchi]], and [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |↑[[WBC]], [[neutrophilia]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |[[Consolidation (medicine)|Lobar consolidation]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |[[Chest X-ray]] and CT Scan | |||
! style="background: #F5F5F5; padding: 5px;" |[[productive cough]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
! rowspan="7" |Chronic Dyspnea | |||
! rowspan="6" |[[Respiratory system]] | |||
! rowspan="6" |[[Chest]] and [[Pleura]], | |||
Lower [[airway]] | |||
![[Bronchiectasis]]<ref name="CantinBankier2009">{{cite journal|last1=Cantin|first1=Luce|last2=Bankier|first2=Alexander A.|last3=Eisenberg|first3=Ronald L.|title=Bronchiectasis|journal=American Journal of Roentgenology|volume=193|issue=3|year=2009|pages=W158–W171|issn=0361-803X|doi=10.2214/AJR.09.3053}}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Rhonchi]], [[Wheezing]], [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |↑[[WBC]], [[neutrophilia]] | |||
! style="background: #F5F5F5; padding: 5px;" |↓[[Oxygen|O2]], ↑[[CO2]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Bronchiectasis chest x ray|Tram-track opacities]] | |||
! style="background: #F5F5F5; padding: 5px;" |↑ [[FEV1]]/[[FVC]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Computed tomography|High resolution computed tomography (HRCT)]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Productive cough|Chronic productive cough]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
![[Interstitial lung disease]]<ref name="pmid2060395">{{cite journal |vauthors=Baughman RP, Shipley RT, Loudon RG, Lower EE |title=Crackles in interstitial lung disease. Comparison of sarcoidosis and fibrosing alveolitis |journal=Chest |volume=100 |issue=1 |pages=96–101 |year=1991 |pmid=2060395 |doi= |url=}}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Rhonchi]], [[Wheezing]], [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |↓[[Oxygen|O2]], ↑[[CO2]] | |||
! style="background: #F5F5F5; padding: 5px;" |Peripheral [[pulmonary]] infiltrative opacification | |||
! style="background: #F5F5F5; padding: 5px;" |↑ [[FEV1]]/[[FVC]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Computed tomography|High resolution computed tomography (HRCT)]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Pneumoconiosis]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
![[Sarcoidosis]]<ref name="pmid14518232">{{cite journal |vauthors=Moher D, Cole CW, Hill GB |title=Epidemiology of abdominal aortic aneurysm: the effect of differing definitions |journal=Eur J Vasc Surg |volume=6 |issue=6 |pages=647–50 |date=November 1992 |pmid=1451823 |doi= |url= |author=}}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |↓[[Oxygen|O2]], ↑[[CO2]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Hilar lymphadenopathy|Hilar adenopathy]] | |||
! style="background: #F5F5F5; padding: 5px;" |↑ [[FEV1]]/[[FVC]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Computed tomography|High resolution computed tomography (HRCT)]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Hypercalcemia]], high [[Angiotensin-converting enzyme|ACE]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
![[Alveolitis]]<ref name="pmid15692967">{{cite journal |vauthors=Khanna D, Clements PJ, Furst DE, Chon Y, Elashoff R, Roth MD, Sterz MG, Chung J, FitzGerald JD, Seibold JR, Varga J, Theodore A, Wigley FM, Silver RM, Steen VD, Mayes MD, Connolly MK, Fessler BJ, Rothfield NF, Mubarak K, Molitor J, Tashkin DP |title=Correlation of the degree of dyspnea with health-related quality of life, functional abilities, and diffusing capacity for carbon monoxide in patients with systemic sclerosis and active alveolitis: results from the Scleroderma Lung Study |journal=Arthritis Rheum. |volume=52 |issue=2 |pages=592–600 |date=February 2005 |pmid=15692967 |doi=10.1002/art.20787 |url= |author=}}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |Basal [[Crackles|crackle]] | |||
! style="background: #F5F5F5; padding: 5px;" |↑[[WBC]], [[neutrophilia]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" | Basal reticulonodular opacification | |||
! style="background: #F5F5F5; padding: 5px;" |↑ [[FEV1]]/[[FVC]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Computed tomography|High resolution computed tomography (HRCT)]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Dry cough]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
![[Cystic fibrosis]]<ref name="ZieglerRovedder2009">{{cite journal|last1=Ziegler|first1=Bruna|last2=Rovedder|first2=Paula Maria Eidt|last3=Dalcin|first3=Paulo de Tarso Roth|last4=Menna-Barreto|first4=Sérgio Saldanha|title=Padrões ventilatórios na espirometria em pacientes adolescentes e adultos com fibrose cística|journal=Jornal Brasileiro de Pneumologia|volume=35|issue=9|year=2009|pages=854–859|issn=1806-3713|doi=10.1590/S1806-37132009000900006}}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Rhonchi]], [[Wheezing]], [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |Normal | |||
! style="background: #F5F5F5; padding: 5px;" |[[Metabolic alkalosis]] | |||
! style="background: #F5F5F5; padding: 5px;" |Thick-walled [[bronchiectasis]] | |||
! style="background: #F5F5F5; padding: 5px;" |↓ [[Forced expiratory volume|FEF<sub>75%</sub>]]/[[FVC]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Sweat test]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Congenital absence of the vas deferens|Absent vas deferens]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
![[Tuberculosis]]<ref name="pmid16709993">{{cite journal| author=Campbell IA, Bah-Sow O| title=Pulmonary tuberculosis: diagnosis and treatment. | journal=BMJ | year= 2006 | volume= 332 | issue= 7551 | pages= 1194-7 | pmid=16709993 | doi=10.1136/bmj.332.7551.1194 | pmc=1463969 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16709993 }}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Rhonchi]], [[Wheezing]], [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |↑[[WBC]] | |||
! style="background: #F5F5F5; padding: 5px;" |↓[[Oxygen|O2]], ↑[[CO2]] | |||
! style="background: #F5F5F5; padding: 5px;" |Patchy [[Consolidation (medicine)|consolidation]] or poorly defined linear and nodular [[Opacity|opacities]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Restrictive Lung Disease|Restrictive]], [[Obstructive lung disease|obstructive]], or mixed | |||
! style="background: #F5F5F5; padding: 5px;" |[[Interferon-γ release assays|IFN-γ release assay (IGRA)]] | |||
[[Acid fast|Acid-fast staining]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Night sweat]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
! colspan="2" |[[Autoimmune]] | |||
![[Wegener's granulomatosis]]<ref name="pmid23034218">{{cite journal| author=Cardenas-Garcia J, Farmakiotis D, Baldovino BP, Kim P| title=Wegener's granulomatosis in a middle-aged woman presenting with dyspnea, rash, hemoptysis and recurrent eye complaints: a case report. | journal=J Med Case Rep | year= 2012 | volume= 6 | issue= | pages= 335 | pmid=23034218 | doi=10.1186/1752-1947-6-335 | pmc=3492078 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23034218 }}</ref> | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+/- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |+ | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |- | |||
! style="background: #F5F5F5; padding: 5px;" |[[Wheezing]], [[Crackles]] | |||
! style="background: #F5F5F5; padding: 5px;" |↓ [[RBC]] | |||
! style="background: #F5F5F5; padding: 5px;" |↓[[Oxygen|O2]], ↑[[CO2]] | |||
! style="background: #F5F5F5; padding: 5px;" |Cavitate [[nodules]], ground-glass opacity | |||
! style="background: #F5F5F5; padding: 5px;" |↓ [[FEV1]]/[[FVC]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Biopsy]] demonstrating a [[granulomatous]] [[vasculitis]] | |||
! style="background: #F5F5F5; padding: 5px;" |[[Rhinosinusitis|Chronic rhinosinusitis]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
|} | |||
{{Family tree/start}} | |||
{{Family tree | | | A01 | | | | | | | | | | A01= <div style="float: left; text-align: left; width: 25em; padding:1em;">'''Prevention of pulmonary edema''' </div>}} | |||
{{Family tree | |,|-|^|-|.| | }} | |||
{{Family tree | B01 | | B02 | | B01= '''Non-cardiogenic pulmonary edema'''<br><div style="float: left; text-align: left; width: 25em; padding:1em;"> </div>| B02= '''Cardiogenic pulmonary edema''' <br> <div style="float: left; text-align: left; width: 25em; padding:1em;"></div>}} | |||
{{Family tree | |!| | | |!| | | | | }} | |||
{{Family tree | C01 | | C02 | | | | C01=<div style="float: left; text-align: left; width: 25em; padding:1em;"> | |||
❑ Encourage healthy lifestyle and exercise<br> | |||
❑ Precautions for pulmonary edema associated with high altitude<br> | |||
** | |||
❑ | |||
❑ (I-A) <br> | |||
❑ Control [[obesity]] (I-C) <br> | |||
❑ (I-C) <br> | |||
❑ Avoid tobacco (I-C) <br> | |||
❑ <br> | |||
❑ <br> </div> | |||
| C02=<div style="float: left; text-align: left; width: 25em; padding:1em;"> | |||
❑ Encourage healthy lifestyle and exercise <br> | |||
❑ Treat [[hypertension]] (I-A) <br> | |||
❑ Treat [[dyslipidemia]] (I-A) <br> | |||
❑ Control [[obesity]] (I-C) <br> | |||
❑ Treat [[DM]] (I-C) <br> | |||
❑ Avoid tobacco (I-C) <br> | |||
❑ Avoid cardiotoxic agents (I-C)</div>}} | |||
{{Family tree | | | | | |!| | | | | }} | |||
{{Family tree | | | | | D01 | | | | D01=<div style="float: left; text-align: left; width: 25em; padding:1em;"> | |||
'''Consider additional measures in selected patients:''' | |||
❑ Administer [[ACE-I]] if history of [[MI]] or [[ACS]] and reduced [[EF]] to prevent symptoms and reduce mortality (I-A), in all decreased [[EF]] to prevent symptoms (I-A) <br> | |||
❑ Administer [[beta-blocker]]s if history of [[MI]] or [[ACS]] and reduced [[EF]] to reduce mortality (I-B), in all reduced [[EF]] to prevent symptoms (I-C) <br> | |||
❑ Administer [[statin]]s if history of [[MI]] or [[ACS]] to prevent symptoms (I-A) <br> | |||
❑ Consider [[ICD]] placement to prevent sudden death if asymptomatic ischemic [[cardiomyopathy]], > 40 days post-MI, [[LVEF]] ≤30%, on adequate medical therapy, and good 1 year survival</div>}} | |||
{{Family tree/end}} | |||
{{familytree/start |summary=Sample 1}} | |||
{{familytree | | | | | | | | A01 |A01=A01}} | |||
{{familytree | | | | |,|-|-|-|^|-|-|-|-|.| | | }} | |||
{{familytree | | | B01 | | | | | | | | B02 | | |B01=B01|B02=B02}} | |||
{{familytree | | | | | | | | | | | | | |!| | | }} | |||
{{familytree | | | | | | | | | | | | | |!| | | }} | |||
{{familytree | |,|-|-|-|v|-|-|-|v|-|-|-|+|-|-|-|.| | }} | |||
{{familytree | |!| | | |!| | | |!| | | |!| | | |!| | | }} | |||
{{familytree | D01 | | D02 | | D03 | | D04 | | D05 |D01=D01|D02=D02|D03=D03|D04=D04|D05=D05}} | |||
{{familytree/end}} | |||
{{Family tree/start}} | |||
{{Family tree | | | | B01 | | | |B01= Pulmonary edema treatment based on classification}} | |||
{{Family tree | |,|-|-|^|-|-|-|-|.| }} | |||
{{Family tree | |C01| | | | |C02|C01= Cardiogenic pulmonary edema| C02= Noncardiogenic pulmonary edema}} | |||
{{familytree | |!| | | | ||| |!| | | }} | |||
{{familytree | |D01| | | | |D02| | |D01= ❑ First step is to stabilize the patient<br> by following the ABCs of [[resuscitation]],<br> that is, [[airway]], [[breathing]], and [[circulation]]<br> ❑ Any associated [[arrhythmia]]<br> or [[myocardial infarction]] should be treated appropriately<br>❑Following drugs are used:<br>❑ [[ACE-I]] or [[ARB]]<br> ❑[[Beta blocker]]s | |||
:❑ [[Bisoprolol]]<br> :❑[[Carvedilol]]<br>:❑Sustained release [[metoprolol succinate]]<br>PLUS ❑[[Loop diuretics]]<br> | |||
:❑ Starting dose:<br>:❑ [[Furosemide]] 20 to 40 mg, '''OR'''<br>:❑ [[Torsemide]] 10 to 20 mg, '''OR'''<br>:❑ [[Bumetanide]] 0.5 to 1 mg<br>❑ Monitor volume status and adjust dose<br>❑ No response: double oral diuretics dose rather than administer BID<br>❑No or minimal response despite maximal diuretic dose<br> then administer another[[diuretics]] BID or TID PLUS<br>❑[[Aldosterone antagonist]]<br>❑Vasopressin antagonists:<br>❑ [[Conivaptan]]<br>❑[[Tolvaptan]]<br>❑ Type III phosphodiesterease inhibitors<br>❑[[Milrinone]] and [[enoximone]]<br>|D02= ❑Treatment of the underlying cause is very important<br>❑ If the cause of pulmonary edema is overdose of | |||
opioid overdose<br>:❑ Naloxone is used for the reversal of symptoms<br>❑ Salicylate toxicity<br>:❑ Sodium bicarbonate is used for the treatment<br>❑ High altitude pulmonary edema treatment:<br> :❑ Oxygen therapy is the first line therapy<br> :❑ Nifedipine<br>:❑Tadalafil and Sildenafil<br>❑Anticoagulants are used for the treatment of pulmonary edema due to pulmonary embolism<br>❑Antibiotics are used to treat underlying infections }} | |||
{{Family tree/end}} | |||
==References== | |||
{{reflist|2}} | |||
<references /> | <references /> | ||
Latest revision as of 14:06, 16 March 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Farnaz Khalighinejad, MD [2]
Overview
This is my sandbox.
Image reference
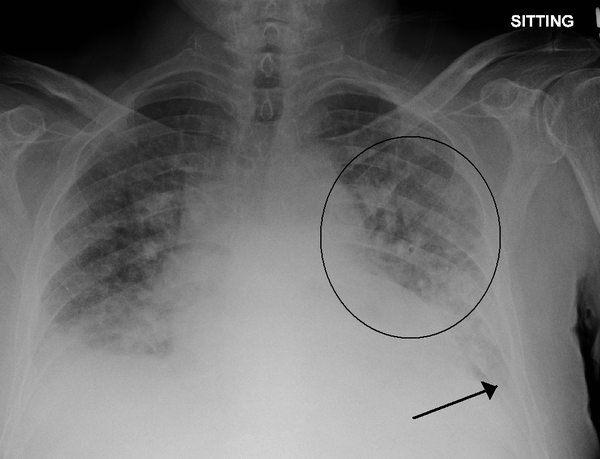
Source: Wikimedia commons
Type 1:
| Pulmonary edema | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Cardiogenic | Non-cardiogenic | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| LV failure | Dysrthmia | LV hypertrophy and cardiomyopathy | Volume Overload | MI | LV outflow obstruction | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Direct injury to lung | Hematogenous injury to lung | Lung injury plus elevated hydrostatic pressure | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Chest trauma,pulmonary contusion | Aspiration | Smoke inhalation | Pneumonia | Oxygen toxicity | Pulmonary embolism,reperfusion | High altitude pulmonary edema | Neurogenic pulmonary edema | Reexpansion pulmonary edema | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sepsis | Pancreatitis | Nonthoracic trauma | Multiple transfusions | Intravenous drug use. e.g. heroin | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
- Direct injury to lung:
- Pulmonary contusion
- Aspiration
- Smoke inhalation
- Pneumonia
- Oxygen toxicity
- Pulmonary embolism,reperfusion
- Hematogenous injury to lung:
- Sepsis
- Pancreatitis
- Nonthoracic trauma
- Multiple transfusions
- Intravenous drug use
- Cardiopulmonary bypass
- Lung injury plus elevated hydrostatic pressure:
- High altitude pulmonary edema
- Neurogenic pulmonary edema
- Reexpansion pulmonary edema
96 patients (174 eyes, 70% females) were included with a mean age at presentation of 30 years
| Pulmonary edema treatment based on classification | |||||||||||||||||||||||
| Cardiogenic pulmonary edema | Noncardiogenic pulmonary edema | ||||||||||||||||||||||
| stabilize patient | |||||||||||||||||||||||
| Cause | Symptom | Diagnosis | Treatment |
|---|---|---|---|
| 1 | |||
| 2 | |||
| 3 |
References
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: Eiman Ghaffarpasand, M.D. [4]
Abbreviations: ABG (arterial blood gas); ACE (angiotensin converting enzyme); BMI (body mass index); CBC (complete blood count); CSF (cerebrospinal fluid); CXR (chest X-ray); ECG (electrocardiogram); FEF (forced expiratory flow rate); FEV1 (forced expiratory volume); FVC (forced vital capacity); JVD (jugular vein distention); MCV (mean corpuscular volume); Plt (platelet); RV (residual volume); SIADH (syndrome of inappropriate antidiuretic hormone); TSH (thyroid stimulating hormone); Vt (tidal volume); WBC (white blood cell);
Prevention of pulmonary edema | |||||||||||||||||||||||||||
| Non-cardiogenic pulmonary edema | Cardiogenic pulmonary edema | ||||||||||||||||||||||||||
❑ Encourage healthy lifestyle and exercise ❑
❑ (I-A) | ❑ Encourage healthy lifestyle and exercise | ||||||||||||||||||||||||||
Consider additional measures in selected patients:
❑ Administer ACE-I if history of MI or ACS and reduced EF to prevent symptoms and reduce mortality (I-A), in all decreased EF to prevent symptoms (I-A) | |||||||||||||||||||||||||||
| A01 | |||||||||||||||||||||||||||||||||||||||||
| B01 | B02 | ||||||||||||||||||||||||||||||||||||||||
| D01 | D02 | D03 | D04 | D05 | |||||||||||||||||||||||||||||||||||||
| Pulmonary edema treatment based on classification | |||||||||||||||||||||||||
| Cardiogenic pulmonary edema | Noncardiogenic pulmonary edema | ||||||||||||||||||||||||
| ❑ First step is to stabilize the patient by following the ABCs of resuscitation, that is, airway, breathing, and circulation ❑ Any associated arrhythmia or myocardial infarction should be treated appropriately ❑Following drugs are used: ❑ ACE-I or ARB ❑Beta blockers
| ❑Treatment of the underlying cause is very important ❑ If the cause of pulmonary edema is overdose of opioid overdose :❑ Naloxone is used for the reversal of symptoms ❑ Salicylate toxicity :❑ Sodium bicarbonate is used for the treatment ❑ High altitude pulmonary edema treatment: :❑ Oxygen therapy is the first line therapy :❑ Nifedipine :❑Tadalafil and Sildenafil ❑Anticoagulants are used for the treatment of pulmonary edema due to pulmonary embolism ❑Antibiotics are used to treat underlying infections | ||||||||||||||||||||||||
References
- ↑ Martindale, Jennifer L.; Noble, Vicki E.; Liteplo, Andrew (2013). "Diagnosing pulmonary edema". European Journal of Emergency Medicine. 20 (5): 356–360. doi:10.1097/MEJ.0b013e32835c2b88. ISSN 0969-9546.
- ↑ Holbro A, Lehmann T, Girsberger S, Stern M, Gambazzi F, Lardinois D, Heim D, Passweg JR, Tichelli A, Bubendorf L, Savic S, Hostettler K, Grendelmeier P, Halter JP, Tamm M (2013). "Lung histology predicts outcome of bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation". Biol. Blood Marrow Transplant. 19 (6): 973–80. doi:10.1016/j.bbmt.2013.03.017. PMID 23562737.
- ↑ Qureshi H, Sharafkhaneh A, Hanania NA (2014). "Chronic obstructive pulmonary disease exacerbations: latest evidence and clinical implications". Ther Adv Chronic Dis. 5 (5): 212–27. doi:10.1177/2040622314532862. PMC 4131503. PMID 25177479.
- ↑ Dela Cruz CS, Tanoue LT, Matthay RA (2011). "Lung cancer: epidemiology, etiology, and prevention". Clin Chest Med. 32 (4): 605–44. doi:10.1016/j.ccm.2011.09.001. PMC 3864624. PMID 22054876.
- ↑ Simonetti AF, Viasus D, Garcia-Vidal C, Carratalà J (2014). "Management of community-acquired pneumonia in older adults". Ther Adv Infect Dis. 2 (1): 3–16. doi:10.1177/2049936113518041. PMC 4072047. PMID 25165554.
- ↑ Cantin, Luce; Bankier, Alexander A.; Eisenberg, Ronald L. (2009). "Bronchiectasis". American Journal of Roentgenology. 193 (3): W158–W171. doi:10.2214/AJR.09.3053. ISSN 0361-803X.
- ↑ Baughman RP, Shipley RT, Loudon RG, Lower EE (1991). "Crackles in interstitial lung disease. Comparison of sarcoidosis and fibrosing alveolitis". Chest. 100 (1): 96–101. PMID 2060395.
- ↑ Moher D, Cole CW, Hill GB (November 1992). "Epidemiology of abdominal aortic aneurysm: the effect of differing definitions". Eur J Vasc Surg. 6 (6): 647–50. PMID 1451823.
- ↑ Khanna D, Clements PJ, Furst DE, Chon Y, Elashoff R, Roth MD, Sterz MG, Chung J, FitzGerald JD, Seibold JR, Varga J, Theodore A, Wigley FM, Silver RM, Steen VD, Mayes MD, Connolly MK, Fessler BJ, Rothfield NF, Mubarak K, Molitor J, Tashkin DP (February 2005). "Correlation of the degree of dyspnea with health-related quality of life, functional abilities, and diffusing capacity for carbon monoxide in patients with systemic sclerosis and active alveolitis: results from the Scleroderma Lung Study". Arthritis Rheum. 52 (2): 592–600. doi:10.1002/art.20787. PMID 15692967.
- ↑ Ziegler, Bruna; Rovedder, Paula Maria Eidt; Dalcin, Paulo de Tarso Roth; Menna-Barreto, Sérgio Saldanha (2009). "Padrões ventilatórios na espirometria em pacientes adolescentes e adultos com fibrose cística". Jornal Brasileiro de Pneumologia. 35 (9): 854–859. doi:10.1590/S1806-37132009000900006. ISSN 1806-3713.
- ↑ Campbell IA, Bah-Sow O (2006). "Pulmonary tuberculosis: diagnosis and treatment". BMJ. 332 (7551): 1194–7. doi:10.1136/bmj.332.7551.1194. PMC 1463969. PMID 16709993.
- ↑ Cardenas-Garcia J, Farmakiotis D, Baldovino BP, Kim P (2012). "Wegener's granulomatosis in a middle-aged woman presenting with dyspnea, rash, hemoptysis and recurrent eye complaints: a case report". J Med Case Rep. 6: 335. doi:10.1186/1752-1947-6-335. PMC 3492078. PMID 23034218.