Spirometry

|
WikiDoc Resources for Spirometry |
|
Articles |
|---|
|
Most recent articles on Spirometry |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Spirometry at Clinical Trials.gov Clinical Trials on Spirometry at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Spirometry
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Spirometry Discussion groups on Spirometry Patient Handouts on Spirometry Directions to Hospitals Treating Spirometry Risk calculators and risk factors for Spirometry
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Spirometry |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Spirometry (meaning the measuring of breath) is the most common of the Pulmonary Function Tests (PFTs), measuring lung function, specifically the measurement of the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is an important tool used for generating pneumotachograph to assessing conditions such as asthma, pulmonary fibrosis, and COPD.
Indications
- Spirometry with and without bronchodilators is used to evaluate all patients with ongoing respiratory illnesses.
- It measures the forced vital capacity (FVC), the forced exhaled volume in 1 second (FEV1), total lung capacity, and residual volume.
- In the presence of airflow limitation, the patient exhales air slowly, while the total volume of air exhaled is generally not affected. Thus airflow obstruction is diagnosed by a reduced FEV1/FVC ratio.
- The American Thoracic Society suggests a ratio of <70% as defining obstruction.
Obstructive lung patterns
- Improvement of FEV1 post bronchodilator therapy indicates an obstructive pattern.
- Bronchodilators can be administered after obtaining baseline spirometry.
- Improvement in airflow obstruction after bronchodilation is shown as an increase in the FEV1.
- Significant reversibility is defined by an increase of ≥ 12% and 200mL in FEV1 from baseline measure after inhalation of a short-acting bronchodilator.
- Sometimes patients will not demonstrate reversibility immediately with bronchodilators, but will after a short course of oral corticosteroids (2 to 3 weeks) is administered to improve control.
Severity of obstruction based on spirometry
- Mild obstruction - > 70%
- Moderate obstruction - 50-70%
- Severe obstruction - < 50%
Spirometry findings in obstructive pattern
- FEV1/FVC - < 70%
- FVC - Normal or decreased
- Total lung capacity - Normal or increased
- Residual volume - Normal or increased
Restrictive lung patterns
- Reduced FVC
- Diseases such as bronchiolitis obliterans with organizing pneumonia, interstitial lung disease,or neuromuscular limitation, present with restrictive patterns on spirometry.
- Other tests used for restrictive lung patterns along with spirometry are helium lung volumes and diffusing capacity of carbon monoxide.
- A total lung capacity < 90% of the predicted values, confirms the presence of a restrictive ventilatory defect.
- A reduction in the FVC < 80%suggests a restrictive ventilatory defect.
Spirometry findings in restrictive pattern
- FEV1/FVC - Normal or increased
- FVC - Decreased
- Total lung capacity - Decreased
- Residual volume - Normal or decreased
Combined restrictive and obstructive defects
- Combination of a reduced FVC (<80%) and a FEV1/FVC <70% may suggest a mixed obstructive and restrictive pattern.
Spirometry testing
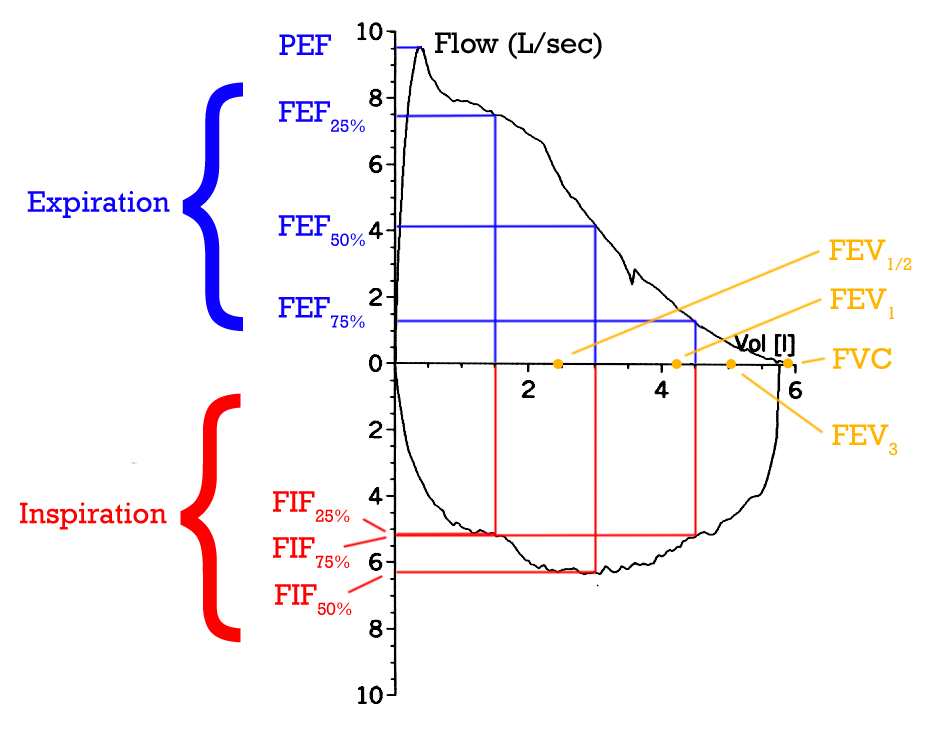
The spirometry test is performed using a device called a spirometer, which comes in several different varieties. Most spirometers display the following graphs:
- a volume-time curve, showing volume (liters) along the Y-axis and time (seconds) along the X-axis
- a flow-volume loop, which graphically depicts the rate of airflow on the Y-axis and the total volume inspired or expired on the X-axis
The most commonly used guidelines for spirometric testing and interpretation are set by the American Thoracic Society (ATS) and the European Respiratory Society (ERS).
Procedure
The basic FVC test varies slightly depending on the equipment used.
Generally, the patient is asked to take the deepest breath they can, and then exhale into the sensor as hard as possible, for as long as possible. It is sometimes directly followed by a rapid inhalation (inspiration), in particular when assessing possible upper airway obstruction. Sometimes, the test will be preceded by a period of quiet breathing in and out from the sensor (tidal volume), or the rapid breath in (forced inspiratory part) will come before the forced exhalation.
During the test, soft nose clips may be used to prevent air escaping through the nose. Filter mouthpieces may be used to prevent the spread of microorganisms, particularly for inspiratory maneuvers.
Limitations of test
The maneuver is highly dependent on patient cooperation and effort, and is normally repeated at least three times to ensure reproducibility. Since results are dependent on patient cooperation, FEV1 and FVC can only be underestimated, never overestimated.
Due to the patient cooperation required, spirometry can only be used on children old enough to comprehend and follow the instructions given (typically about 4-5 years old), and only on patients who are able to understand and follow instructions - thus, this test is not suitable for patients who are unconscious, heavily sedated, or have limitations that would interfere with vigorous respiratory efforts. Other types of lung function tests are available for infants and unconscious persons.
Related tests
Spirometry can also be part of a bronchial challenge test, used to determine bronchial hyperresponsiveness to either rigorous exercise, inhalation of cold/dry air, or with a pharmaceutical agent such as methacholine or histamine.
Sometimes, to assess the reversibility of a particular condition, a bronchodilator is administered before performing another round of tests for comparison. This is commonly referred to as a reversibility test, or a post bronchodilator test (Post BD), and is an important part in diagnosing asthma versus COPD.
Explanation of common test values in FVC tests
| Abbreviation | Name | Description |
|---|---|---|
| FVC | Forced Vital Capacity | This is the total amount of air that can forcibly be blown out after full inspiration, measured in liters. |
| FEV1 | Forced Expiratory Volume in 1 Second | This is the amount of air that you can forcibly blow out in one second, measured in litres. Along with FVC it is considered one of the primary indicators of lung function. |
| FEV1 / FVC | FEV1% | This is the ratio of FEV 1 to FVC. In healthy adults this should be approximately 75 - 80%. |
| PEF | Peak Expiratory Flow | This is the speed of the air moving out of your lungs at the beginning of the expiration, measured in liters per second. |
| FEF 25-75% or 25-50% | Forced Expiratory Flow 25-75% or 25-50% | This is the average flow (or speed) of air coming out of the lung during the middle portion of the expiration (also sometimes referred to as the MMEF, for maximal mid-expiratory flow). |
| FIF 25-75% or 25-50% | Forced Inspiratory Flow 25%-75% or 25%-50% | This is similar to FEF 25%-75% or 25%-50% except the measurement is taken during inspiration. |
| FET | Forced Expiratory Time | This measures the length of the expiration in seconds. |
| SVC | Slow Vital capacity | |
| TV | Tidal Volume | During the respiratory cycle, a specific volume of air is drawn into and then expired out of the lungs. This volume is tidal volume. |
| MVV | Maximum Voluntary Ventilation | a measure of the maximum amount of air that can be inhaled and exhaled in one minute, measured in liters/minute. |
Note that functional residual capacity (FRC) cannot be measured via spirometry, but it can be measured with a plethysmograph.
Results are usually given in both raw data (liters, liters per second) and percent predicted - the test result as a percent of the "predicted values" for the patients of similar characteristics (height, age, sex, and sometimes race and weight). The interpretation of the results can vary depending on the physician and the source of the predicted values. Generally speaking, results nearest to 100% predicted are the most normal, and results over 80% are often considered normal. However, review by a doctor is necessary for accurate diagnosis of any individual situation.
Technologies used in spirometers
- Volumetric Spirometers
- Water bell
- Bellows wedge
- Flow measuring Spirometers
- Fleisch-pneumotach
- Lilly (screen) pneumotach
- Turbine(actually a rotating vane, this spins, the revolutions are counted as they break a light beam)
- Pitot tube
- Hot-wire anemometer
- Ultrasound