STEMI resident survival guide: Difference between revisions
No edit summary |
|||
| (16 intermediate revisions by 2 users not shown) | |||
| Line 26: | Line 26: | ||
==Pre-Hospital Care== | ==Pre-Hospital Care== | ||
Pre-hospital care can begin in the ambulance by [[Emergency Medical Services]] (EMS) personnel and it can decrease the delay in the management of [[STEMI]] patients. In the United States, volunteers and fire fighters are permitted to initiate emergency care prior to the arrival of highly trained paramedics by beginning [[CPR]] and if adequately trained, can defibrillate the patient using an [[Defibrillation|automatic external defibrillator]]. Early access to EMS is promoted by a 9-1-1 system. | Pre-hospital care can begin in the ambulance by [[Emergency Medical Services]] (EMS) personnel and it can decrease the delay in the management of [[STEMI]] patients. In the United States, volunteers and fire fighters are permitted to initiate emergency care prior to the arrival of highly trained [[paramedics]] by beginning [[CPR]] and if adequately trained, can defibrillate the patient using an [[Defibrillation|automatic external defibrillator]]. Early access to [[EMS]] is promoted by a 9-1-1 system. | ||
{{Family tree/start}} | {{Family tree/start}} | ||
| Line 37: | Line 37: | ||
:❑ [[Aspirin|Non-enteric coated aspirin]] | :❑ [[Aspirin|Non-enteric coated aspirin]] | ||
:❑ [[Nitroglycerin|Sublingual nitroglycerin]] if an [[RV infarct]] and / or [[hypotension]] are not present | :❑ [[Nitroglycerin|Sublingual nitroglycerin]] if an [[RV infarct]] and / or [[hypotension]] are not present | ||
:❑ In so far as the risk of emergency coronary bypass surgery is <u><</u>1%, a thienopyridine such as [[Prasugrel]], [[Ticagrelor]] or [[Clopidogrel]] can be administered | :❑ In so far as the risk of emergency [[CABG|coronary artery bypass surgery]] is <u><</u>1%, a [[thienopyridine]] such as [[Prasugrel]], [[Ticagrelor]] or [[Clopidogrel]] can be administered | ||
:❑ [[Unfractionated heparin]] | :❑ [[Unfractionated heparin]] | ||
:❑ [[Glycoprotein IIb IIIa inhibitors]] | :❑ [[Glycoprotein IIb IIIa inhibitors]] | ||
| Line 49: | Line 49: | ||
==FIRE: Focused Initial Rapid Evaluation== | ==FIRE: Focused Initial Rapid Evaluation== | ||
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.<ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref> | A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.<ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref> | ||
<span style="font-size:85%"> '''Abbreviations:''' | <span style="font-size:85%"> '''Abbreviations:''' | ||
| Line 73: | Line 72: | ||
:❑ New [[LBBB|<span style="color:white;">LBBB</span>]]<br> | :❑ New [[LBBB|<span style="color:white;">LBBB</span>]]<br> | ||
''Click [[STEMI resident survival guide#Gallery|<span style="color:white;">here </span>]] for the gallery of ECG examples below.'' | ''Click [[STEMI resident survival guide#Gallery|<span style="color:white;">here </span>]] for the gallery of ECG examples below.'' | ||
❑ '''Increase in [[troponin|<span style="color:white;">troponin</span>]] and / or CK MB'''</div>}} | ❑ '''Increase in [[troponin|<span style="color:white;">troponin</span>]] and / or [[CKMB|<span style="color:white;">CK MB </span>]]'''</div>}} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G02 | G02= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Rule out life threatening alternative diagnoses:'''<br> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G02 | G02= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Rule out life threatening alternative diagnoses:'''<br> | ||
❑ [[Aortic dissection|<span style="color:white;">Aortic dissection</span>]] <br> (suggestive findings: [[back pain|<span style="color:white;">back pain</span>]], interscapular pain, [[aortic regurgitation|<span style="color:white;">aortic regurgitation</span>]], [[pulsus paradoxus|<span style="color:white;">pulsus paradoxus</span>]], [[blood pressure|<span style="color:white;">blood pressure</span>]] discrepancy between the arms) <br> | ❑ [[Aortic dissection|<span style="color:white;">Aortic dissection</span>]] <br> (suggestive findings: [[back pain|<span style="color:white;">back pain</span>]], [[interscapular pain|<span style="color:white;">interscapular pain</span>]], [[aortic regurgitation|<span style="color:white;">aortic regurgitation</span>]], [[pulsus paradoxus|<span style="color:white;">pulsus paradoxus</span>]], [[blood pressure|<span style="color:white;">blood pressure</span>]] discrepancy between the arms) <br> | ||
❑ [[Pulmonary embolism|<span style="color:white;">Pulmonary embolism</span>]] <br> (suggestive findings: acute onset of [[dyspnea|<span style="color:white;">dyspnea</span>]], [[tachypnea|<span style="color:white;">tachypnea</span>]], [[hemoptysis|<span style="color:white;">hemoptysis</span>]], previous [[DVT|<span style="color:white;">DVT</span>]]) <br> | ❑ [[Pulmonary embolism|<span style="color:white;">Pulmonary embolism</span>]] <br> (suggestive findings: acute onset of [[dyspnea|<span style="color:white;">dyspnea</span>]], [[tachypnea|<span style="color:white;">tachypnea</span>]], [[hemoptysis|<span style="color:white;">hemoptysis</span>]], previous [[DVT|<span style="color:white;">DVT</span>]]) <br> | ||
❑ [[Cardiac tamponade|<span style="color:white;">Cardiac tamponade</span>]] <br> (suggestive findings: [[hypotension|<span style="color:white;">hypotension</span>]], [[jugular venous distention|<span style="color:white;">jugular venous distention</span>]], [[muffled heart sounds|<span style="color:white;">muffled heart sounds</span>]])<br> | ❑ [[Cardiac tamponade|<span style="color:white;">Cardiac tamponade</span>]] <br> (suggestive findings: [[hypotension|<span style="color:white;">hypotension</span>]], [[jugular venous distention|<span style="color:white;">jugular venous distention</span>]], [[muffled heart sounds|<span style="color:white;">muffled heart sounds</span>]], [[pulsus paradoxus|<span style="color:white;">pulsus paradoxus</span>]])<br> | ||
❑ [[Tension pneumothorax|<span style="color:white;">Tension pneumothorax</span>]] <br> (suggestive findings: sudden [[dyspnea|<span style="color:white;">dyspnea</span>]], [[tachycardia|<span style="color:white;">tachycardia</span>]], [[trauma|<span style="color:white;">chest trauma</span>]], unilateral absence of breath sounds)<br> | ❑ [[Tension pneumothorax|<span style="color:white;">Tension pneumothorax</span>]] <br> (suggestive findings: sudden [[dyspnea|<span style="color:white;">dyspnea</span>]], [[tachycardia|<span style="color:white;">tachycardia</span>]], [[trauma|<span style="color:white;">chest trauma</span>]], unilateral absence of [[breath sounds|<span style="color:white;">breath sound</span>]])<br> | ||
❑ [[Esophageal rupture|<span style="color:white;">Esophageal rupture</span>]] <br> (suggestive findings: [[vomiting|<span style="color:white;">vomiting</span>]], [[subcutaneous emphysema|<span style="color:white;">subcutaneous emphysema</span>]])</div>}} | ❑ [[Esophageal rupture|<span style="color:white;">Esophageal rupture</span>]] <br> (suggestive findings: [[vomiting|<span style="color:white;">vomiting</span>]], [[subcutaneous emphysema|<span style="color:white;">subcutaneous emphysema</span>]])</div>}} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G01 | G01= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Assess appropriateness of patients for perfusion therapy:''' | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G01 | G01= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Assess appropriateness of patients for perfusion therapy:''' | ||
❑ Contraindications to fibrinolytics [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">(click here for the complete list)</span>]] <br> | ❑ [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">Contraindications to fibrinolytics</span>]] [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">(click here for the complete list shown below)</span>]] <br> | ||
❑ Assess the [[femoral pulse|<span style="color:white;">femoral pulses</span>]] (strength, bruit) <br> | ❑ Assess the [[femoral pulse|<span style="color:white;">femoral pulses</span>]] (strength, [[bruit|<span style="color:white;">bruit</span>]]) <br> | ||
❑ [[Pericarditis|<span style="color:white;">Pericarditis</span>]] (suggestive finding: [[ | ❑ [[Pericarditis resident survival guide|<span style="color:white;">Pericarditis</span>]] (suggestive finding: [[Pericarditis resident survival guide|<span style="color:white;">pericardial friction rub</span>]])<br> </div> }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G01 | G01= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Consider right ventricular MI in case of:''' | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G01 | G01= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Consider [[RVMI|<span style="color:white;">right ventricular MI</span>]] in case of:''' | ||
❑ [[Hypotension|<span style="color:white;">Hypotension</span>]]<br> | ❑ [[Hypotension|<span style="color:white;">Hypotension</span>]]<br> | ||
❑ Elevated [[jugular venous pressure|<span style="color:white;">jugular venous pressure</span>]]<br> | ❑ Elevated [[jugular venous pressure|<span style="color:white;">jugular venous pressure</span>]]<br> | ||
| Line 101: | Line 100: | ||
'''[[Right ventricular myocardial infarction resident survival guide|<span style="color:white;">Click here for right ventricular myocardial infarction resident survival guide</span>]]'''</div>}} | '''[[Right ventricular myocardial infarction resident survival guide|<span style="color:white;">Click here for right ventricular myocardial infarction resident survival guide</span>]]'''</div>}} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | I01 | | | I01= <div style="float: left; text-align: left; width: 35em; padding:1em;">'''Check for hypoperfusion and left ventricular failure:'''<br> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | I01 | | | I01= <div style="float: left; text-align: left; width: 35em; padding:1em;">'''Check for hypoperfusion and [[left ventricular failure|<span style="color:white;">left ventricular failure </span>]]:'''<br> | ||
❑ [[Hypotension|<span style="color:white;">Hypotension</span>]] <br> | ❑ [[Hypotension|<span style="color:white;">Hypotension</span>]] <br> | ||
❑ [[Tachycardia|<span style="color:white;">Tachycardia</span>]] <br> | ❑ [[Tachycardia|<span style="color:white;">Tachycardia</span>]] <br> | ||
❑ [[Cyanosis|<span style="color:white;">Cyanotic skin and nail bed</span>]] <br> | ❑ [[Cyanosis|<span style="color:white;">Cyanotic skin and nail bed</span>]] <br> | ||
❑ [[ | ❑ [[Clammy skin|<span style="color:white;">Cold skin</span>]] <br> | ||
❑ [[Skin mottling|<span style="color:white;">Skin mottling</span>]] <br> | ❑ [[Skin mottling|<span style="color:white;">Skin mottling</span>]] <br> | ||
❑ Patient lies still <br> | ❑ Patient lies still <br> | ||
| Line 118: | Line 117: | ||
:❑ Caution in [[COPD|<span style="color:white;">COPD</span>]] patients: maintain an oxygen saturation between 88% and 92% | :❑ Caution in [[COPD|<span style="color:white;">COPD</span>]] patients: maintain an oxygen saturation between 88% and 92% | ||
❑ Administer [[beta-blockers|<span style="color:white;">beta-blockers</span>]] (unless contraindicated) and titrate to the [[heart rate|<span style="color:white;">heart rate</span>]] and [[blood pressure|<span style="color:white;">blood pressure </span>]]<br> | ❑ Administer [[beta-blockers|<span style="color:white;">beta-blockers</span>]] (unless contraindicated) and titrate to the [[heart rate|<span style="color:white;">heart rate</span>]] and [[blood pressure|<span style="color:white;">blood pressure </span>]]<br> | ||
<span style="font-size:85%;">Contraindicated in heart failure, prolonged or high degree AV block, reactive airway disease, high risk of cardiogenic shock and low cardiac output state</span> <br> | <span style="font-size:85%;">Contraindicated in [[heart failure|<span style="color:white;">heart failure </span>]], [[AV block |<span style="color:white;">prolonged or high degree AV block </span>]], [[reactive airway disease|<span style="color:white;">reactive airway disease </span>]], high risk of [[cardiogenic shock|<span style="color:white;">cardiogenic shock </span>]] and low [[cardiac output|<span style="color:white;">cardiac output</span>]] state</span> <br> | ||
:❑ [[Metoprolol|<span style="color:white;">Metoprolol</span>]] IV, 5 mg every 5 min, up to 3 doses | :❑ [[Metoprolol|<span style="color:white;">Metoprolol</span>]] IV, 5 mg every 5 min, up to 3 doses | ||
:❑ [[Carvedilol|<span style="color:white;">Carvedilol</span>]] IV, 25 mg, two times a day | :❑ [[Carvedilol|<span style="color:white;">Carvedilol</span>]] IV, 25 mg, two times a day | ||
❑ Administer sublingual [[nitroglycerin|<span style="color:white;">nitroglycerin</span>]] 0.4 mg every 5 minutes for a total of 3 doses<br> | ❑ Administer sublingual [[nitroglycerin|<span style="color:white;">nitroglycerin</span>]] 0.4 mg every 5 minutes for a total of 3 doses<br> | ||
<span style="font-size:85%;">Contraindicated in suspected right ventricular MI, recent use of phosphodiesterase inhibitors, decreased blood pressure 30 mmHg below baseline</span> <br> | <span style="font-size:85%;">Contraindicated in suspected [[RVMI|<span style="color:white;">right ventricular MI </span>]], recent use of [[phosphodiesterase inhibitors|<span style="color:white;">phosphodiesterase inhibitors </span>]], decreased [[blood pressure|<span style="color:white;">blood pressure </span>]] 30 mmHg below baseline</span> <br> | ||
❑ Administer IV [[morphine|<span style="color:white;">morphine</span>]] if needed | ❑ Administer IV [[morphine|<span style="color:white;">morphine</span>]] if needed | ||
:❑ Initial dose 4-8 mg | :❑ Initial dose 4-8 mg | ||
| Line 138: | Line 137: | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | C03 | | C04 | C03= '''NO''' | C04= '''YES'''}} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | C03 | | C04 | C03= '''NO''' | C04= '''YES'''}} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| | | |!| | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| | | |!| | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | D01 | | D02 | | D03 | |D01=<div style="float: left; text-align: center; width: 25em; padding:1em;">❑ '''Primary PCI within 90 minutes''' <br></div> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | D01 | | D02 | | D03 | |D01=<div style="float: left; text-align: center; width: 25em; padding:1em;">❑ '''[[Primary PCI|<span style="color:white;">Primary PCI</span>]] within 90 minutes''' <br></div> | ||
| D02= <div style="float: left; text-align: center; width: 25em; padding:1em;">❑ '''Fibrinolytic therapy within 30 min''' </div> | | D02= <div style="float: left; text-align: center; width: 25em; padding:1em;">❑ '''[[Fibrinolytic therapy|<span style="color:white;">Fibrinolytic therapy</span>]] within 30 min''' </div> | ||
| D03= <div style="float: left; text-align: center; width: 15em; padding:1em;">❑ '''Transfer for primary PCI''' </div> | | D03= <div style="float: left; text-align: center; width: 15em; padding:1em;">❑ '''Transfer for [[primary PCI|<span style="color:white;">primary PCI </span>]]''' </div> | ||
}} | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| | | | | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| | | | | }} | ||
| Line 152: | Line 151: | ||
:❑ Symptoms of [[ischemia|<span style="color:white;">ischemia</span>]] <12 hours ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence A</span>]]) <br> | :❑ Symptoms of [[ischemia|<span style="color:white;">ischemia</span>]] <12 hours ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence A</span>]]) <br> | ||
:❑ Ongoing [[ischemia|<span style="color:white;">ischemia</span>]] 12-24 hours following onset ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence C</span>]])<br> | :❑ Ongoing [[ischemia|<span style="color:white;">ischemia</span>]] 12-24 hours following onset ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence C</span>]])<br> | ||
❑ '''Confirm that the patient has no [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">contraindications to fibrinolytics</span>]]''' | ❑ '''Confirm that the patient has no [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">contraindications to fibrinolytics</span>]] [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">(click here for the complete list shown below)</span>]] <br>''' | ||
</div>}} | </div>}} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| }} | ||
| Line 186: | Line 185: | ||
::❑ 0.75-mg/kg IV bolus, then 1.75–mg/kg/h infusion | ::❑ 0.75-mg/kg IV bolus, then 1.75–mg/kg/h infusion | ||
::❑ Additional bolus of 0.3 mg/kg if needed | ::❑ Additional bolus of 0.3 mg/kg if needed | ||
::❑ Decrease infusion to 1 mg/kg/h when creatinine clearance <30 mL/min | ::❑ Decrease infusion to 1 mg/kg/h when [[creatinine|<span style="color:white;">creatinine</span>]] clearance <30 mL/min | ||
</div> | </div> | ||
| F03=<div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Administer ONE of the following [[fibrinolytic therapy|<span style="color:white;">fibrinolytic therapy</span>]]:''' <br> | | F03=<div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Administer ONE of the following [[fibrinolytic therapy|<span style="color:white;">fibrinolytic therapy</span>]]:''' <br> | ||
| Line 194: | Line 193: | ||
:❑ 40 mg for weight 70-79 kg | :❑ 40 mg for weight 70-79 kg | ||
:❑ 45 mg for weight 80-89 kg | :❑ 45 mg for weight 80-89 kg | ||
:❑ 50 mg for weight ≥90 kg | :❑ 50 mg for weight ≥90 kg<ref name="pmid11136484">{{cite journal| author=Wang-Clow F, Fox NL, Cannon CP, Gibson CM, Berioli S, Bluhmki E et al.| title=Determination of a weight-adjusted dose of TNK-tissue plasminogen activator. | journal=Am Heart J | year= 2001 | volume= 141 | issue= 1 | pages= 33-40 | pmid=11136484 | doi=10.1067/mhj.2001.112092 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11136484 }} </ref> | ||
❑ [[Reteplase|<span style="color:white;">Reteplase</span>]] 10 units IV boluses every 30 min <br> | ❑ [[Reteplase|<span style="color:white;">Reteplase</span>]] 10 units IV boluses every 30 min <br> | ||
❑ [[Alteplase|<span style="color:white;">Alteplase</span>]] | ❑ [[Alteplase|<span style="color:white;">Alteplase</span>]] | ||
| Line 235: | Line 234: | ||
❑ Other high risk features | ❑ Other high risk features | ||
</div> | </div> | ||
|G02= <div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Transfer to a PCI- | |G02= <div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Transfer to a PCI-capable hospital for non primary PCI, if there is:''' <br> | ||
❑ [[Cardiogenic shock|<span style="color:white;">Cardiogenic shock</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]]) <br> | ❑ [[Cardiogenic shock|<span style="color:white;">Cardiogenic shock</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]]) <br> | ||
❑ Acute severe [[heart failure|<span style="color:white;">heart failure</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]]) <br> | ❑ Acute severe [[heart failure|<span style="color:white;">heart failure</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]]) <br> | ||
❑ Spontaneous or easily provoked myocardial ischemia ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence C</span>]]) <br> | ❑ Spontaneous or easily provoked myocardial ischemia ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence C</span>]]) <br> | ||
❑ Failed reperfusion after [[fibrinolytic therapy|<span style="color:white;">fibrinolytics</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) <br> | ❑ Failed reperfusion after [[fibrinolytic therapy|<span style="color:white;">fibrinolytics</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) <br> | ||
❑ Reocclusion after fibrinolytics ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) <br> | ❑ Reocclusion after [[fibrinolytic therapy|<span style="color:white;">fibrinolytics</span>]]([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) <br> | ||
❑ Successful fibrinolytic reperfusion, between 3 and 24 hours ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) | ❑ Successful fibrinolytic reperfusion, between 3 and 24 hours ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) | ||
</div> }} | </div> }} | ||
| Line 256: | Line 255: | ||
❑ [[Ischemic stroke]] within the last 3 months (unless within 4.5 hours)<br> | ❑ [[Ischemic stroke]] within the last 3 months (unless within 4.5 hours)<br> | ||
❑ Structural cerebral vascular lesion<br> | ❑ Structural cerebral vascular lesion<br> | ||
❑ Primary | ❑ Primary or [[metastasis|metastatic]] intracranial [[malignancy]] <br> | ||
❑ Suspicion of [[aortic dissection]]<br> | ❑ Suspicion of [[aortic dissection]]<br> | ||
❑ Increased bleeding tendency or active [[bleeding]] <br> | ❑ Increased bleeding tendency or active [[bleeding]] <br> | ||
| Line 264: | Line 263: | ||
❑ Previous treatment with [[streptokinase]] within the last 6 months | ❑ Previous treatment with [[streptokinase]] within the last 6 months | ||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ❑ [[Oral anticoagulation therapy]] <br> | | style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ❑ [[Oral anticoagulation therapy]] <br> | ||
❑ Pregnancy <br> | ❑ [[Pregnancy]] <br> | ||
❑ Active [[peptic ulcer]] <br> | ❑ Active [[peptic ulcer]] <br> | ||
❑ Previous history of chronic severe [[hypertension]] that is poorly controlled<br> | ❑ Previous history of chronic severe [[hypertension]] that is poorly controlled<br> | ||
| Line 346: | Line 345: | ||
❑ [[Femoral artery|Femoral pulse]] (if a patient is to undergo [[PCI]])<br> | ❑ [[Femoral artery|Femoral pulse]] (if a patient is to undergo [[PCI]])<br> | ||
:❑ Strength | :❑ Strength | ||
:❑ Bruits | :❑ [[Bruits]] | ||
'''Skin''' <br> | '''Skin''' <br> | ||
| Line 431: | Line 430: | ||
---- | ---- | ||
'''Assess the patient for ischemia:'''<br> | '''Assess the patient for ischemia:'''<br> | ||
❑ Perform non invasive testing before discharge for the evaluation of ischemia among patients who did not undergo [[coronary angiography]] and in whom | ❑ Perform non invasive testing before discharge for the evaluation of ischemia among patients who did not undergo [[coronary angiography]] and in whom [[coronary angiography]] is not warranted due to the absence of high risk features ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]) <br> | ||
❑ Assess the [[LVEF]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]) | ❑ Assess the [[LVEF]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]) | ||
</div>}} | </div>}} | ||
| Line 443: | Line 442: | ||
:❑ [[Aspirin]] 81-325 mg (indefinitely) | :❑ [[Aspirin]] 81-325 mg (indefinitely) | ||
:❑ [[Antiplatelet drug|Antiplatelet therapy]] | :❑ [[Antiplatelet drug|Antiplatelet therapy]] | ||
:❑ Consider oral factor Xa inhibition with [[Rivaroxaban]] outside the US based upon EMA approval (Note [[Rivaroxaban]] is not FDA approved for use in ACS in the US) | |||
:❑ [[Beta blockers]] | :❑ [[Beta blockers]] | ||
:❑ [[ACE inhibitors]] or [[ARB]] (in case of [[anterior MI]], [[ejection fraction]] ≤ 40% or [[heart failure]]) | :❑ [[ACE inhibitors]] or [[ARB]] (in case of [[anterior MI]], [[ejection fraction]] ≤ 40% or [[heart failure]]) | ||
| Line 461: | Line 461: | ||
==Do's== | ==Do's== | ||
* | * A pre-hospital [[ECG]] is recommended. If [[STEMI]] is diagnosed the [[PCI]] team should be activated while the patient is en route to the hospital. | ||
* Administer reperfusion therapy for all patients presenting with [[STEMI]] within 12 hours of the beginning of the symptoms ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]). | * Administer reperfusion therapy for all patients presenting with [[STEMI]] within 12 hours of the beginning of the symptoms ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]). | ||
| Line 506: | Line 506: | ||
==Don'ts== | ==Don'ts== | ||
* Do not administer IV [[beta-blockers]] among patients with elevated risk for cardiogenic shock, signs of [[heart failure]], low ouput state, prolonged [[PR interval]] more than 0.24 seconds, second or third degree block or [[asthma]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]). | * Do not administer IV [[beta-blockers]] among patients with elevated risk for cardiogenic shock, signs of [[heart failure]], low ouput state, prolonged [[PR interval]] more than 0.24 seconds, [[second degree AV block|second]] or [[third degree block]] or [[asthma]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]). | ||
* Do not administer IV [[GP IIb/IIIa inhibitors]] to patients with low risk of ischemic events or at high risk of bleeding and who are already on aspirin and P2Y12 receptor inhibitors therapy. | * Do not administer IV [[GP IIb/IIIa inhibitors]] to patients with low risk of ischemic events or at high risk of bleeding and who are already on aspirin and P2Y12 receptor inhibitors therapy. | ||
* Do not administer [[nitroglycerine]] to patients with systolic | * Do not administer [[nitroglycerine]] to patients with [[systolic blood pressure]] < 90 mm Hg or ≥ to 30 mm Hg below baseline, severe [[bradycardia]] (< 50 bpm), [[tachycardia]] (> 100 bpm), or suspected [[RVMI|right ventricular myocardial infarction]]. | ||
* Do not delay the time for reperfusion. | * Do not delay the time for reperfusion. | ||
| Line 518: | Line 518: | ||
** Active pathological bleeding | ** Active pathological bleeding | ||
** Age ≥75 years of age, (except in high-risk patients such as diabetes or prior MI, where its use may be considered) | ** Age ≥75 years of age, (except in high-risk patients such as diabetes or prior MI, where its use may be considered) | ||
** Urgent coronary artery bypass graft surgery (CABG) is likely | ** Urgent [[coronary artery bypass graft]] surgery ([[CABG]]) is likely | ||
** Presence of additional risk factors for bleeding such as body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of bleeding<ref name="dailymed.nlm.nih.gov">{{Cite web | last = | first = | title = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6 | url = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6 | publisher = | date = | accessdate = 6 February 2014 }}</ref> | ** Presence of additional risk factors for [[bleeding]] such as body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of [[bleeding]]<ref name="dailymed.nlm.nih.gov">{{Cite web | last = | first = | title = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6 | url = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6 | publisher = | date = | accessdate = 6 February 2014 }}</ref> | ||
* Do not administer [[fibrinolytic therapy]] to patients with known [[cerebral arteriovenous malformation]] or to patients with suspected [[aortic dissection]]. | * Do not administer [[fibrinolytic therapy]] to patients with known history of [[intracranial hemorrhage]], [[cerebral arteriovenous malformation]] or to patients with suspected [[aortic dissection]]. | ||
* Do not withhold [[aspirin]] among patients who are planned to undergo urgent [[CABG]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]).<ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref> | * Do not withhold [[aspirin]] among patients who are planned to undergo urgent [[CABG]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]).<ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref> | ||
| Line 551: | Line 551: | ||
[[Category:Resident survival guide]] | [[Category:Resident survival guide]] | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
</div> | </div> | ||
Latest revision as of 15:26, 8 August 2014
| STEMI Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Pre-Hospital Care |
| FIRE |
| Complete Diagnosis |
| Pre-Discharge Care |
| Long Term Management |
| Do's |
| Don'ts |
| Gallery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]; Rim Halaby, M.D. [3]
Overview
ST elevation myocardial infarction (STEMI) is a syndrome characterized by the presence of symptoms of myocardial ischemia associated with persistent ST elevation on electrocardiogram and elevated cardiac enzymes. The management of STEMI should be initiated without delay and the following timelines should be minimized (the 4 D's):
Door to Data
If a patient presents with chest discomfort, an electrocardiogram must be obtained immediately and no later than 5-10 minutes after arrival. In the patient with chest discomfort, an electrocardiogram should be obtained prior to obtaining insurance / payment information.
Data to Decision
If the electrocardiogram shows ST segment elevation, ST segment depression consistent with posterior MI, or a new left bundle branch block, a decision must be made within 5 to 10 minutes as to whether to administer a fibrinolytic agent or to proceed to primary angioplasty.
Decision to Drug or Device
Once a decision is made to administer a fibrinolytic agent or to proceed to primary angioplasty this should be carried out within 30 minutes.
Causes
Life Threatening Causes
STEMI is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Plaque rupture
- Takotsubo cardiomyopathy (also known as broken heart syndrome or stress cardiomyopathy)
- Aortic dissection with propagation to the right coronary artery
- Cocaine
Pre-Hospital Care
Pre-hospital care can begin in the ambulance by Emergency Medical Services (EMS) personnel and it can decrease the delay in the management of STEMI patients. In the United States, volunteers and fire fighters are permitted to initiate emergency care prior to the arrival of highly trained paramedics by beginning CPR and if adequately trained, can defibrillate the patient using an automatic external defibrillator. Early access to EMS is promoted by a 9-1-1 system.
Prehospital Care ❑ Check the vital signs
❑ Activate the cardiac cath team in the hospital | |||||||||
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.[1]
Abbreviations: LBBB: left bundle branch block; CABG: coronary artery bypass graft; COPD: chronic obstructive pulmonary disease; DVT: deep vein thrombosis; ECG: electrocardiography; GP IIb IIIa: glycoprotein IIb IIIa; LAD: left anterior descending; MI: myocardial infarction; PCI: percutaneous coronary intervention; SC: subcutaneous injection; STEMI: ST elevation myocardial infarction
Boxes in red signify that an urgent management is needed.
Identify cardinal findings of STEMI: ❑ Chest pain or chest discomfort
❑ Characteristic ECG changes consistent with STEMI
Click here for the gallery of ECG examples below. ❑ Increase in troponin and / or CK MB | |||||||||||||||||||||||
Rule out life threatening alternative diagnoses: ❑ Aortic dissection (suggestive findings: vomiting, subcutaneous emphysema) | |||||||||||||||||||||||
Assess appropriateness of patients for perfusion therapy:
❑ Contraindications to fibrinolytics (click here for the complete list shown below) | |||||||||||||||||||||||
Consider right ventricular MI in case of:
❑ Hypotension
| |||||||||||||||||||||||
Order a right sided ECG in all patients with ST elevation in leads II, III and aVF: ❑ Clearly label the ECG as right sided | |||||||||||||||||||||||
Check for hypoperfusion and left ventricular failure : ❑ Hypotension | |||||||||||||||||||||||
Begin initial treatment: ❑ Administer 162 - 325 mg of non enteric aspirin
❑ Administer 2-4 L/min oxygen via nasal cannula when saturation <90%
❑ Administer beta-blockers (unless contraindicated) and titrate to the heart rate and blood pressure
❑ Administer sublingual nitroglycerin 0.4 mg every 5 minutes for a total of 3 doses
❑ Administer 80 mg atorvastatin | |||||||||||||||||||||||
Is PCI available? | |||||||||||||||||||||||
YES | NO | ||||||||||||||||||||||
| Is first medical contact to device ≤ 120 min? | |||||||||||||||||||||||
| NO | YES | ||||||||||||||||||||||
❑ Primary PCI within 90 minutes | ❑ Fibrinolytic therapy within 30 min | ❑ Transfer for primary PCI | |||||||||||||||||||||
Confirm that the patient has one of the following indications: ❑ Symptoms of ischemia <12 hours (Class I, level of evidence A) | ❑ Confirm that the patient has one of the following indications:
❑ Confirm that the patient has no contraindications to fibrinolytics (click here for the complete list shown below) | ||||||||||||||||||||||
Administer ONE of the following antiplatelet agents (before or at the time of PCI):
Prasugrel is contraindicated in case of prior history of strokes or TIAs, active pathological bleeding, age ≥75 years, when urgent coronary artery bypass graft surgery (CABG) is likely, body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of bleeding
Administer ONE of the following anticoagulant therapy:
| Administer ONE of the following fibrinolytic therapy: ❑ Tenecteplase single IV bolus
❑ Reteplase 10 units IV boluses every 30 min
❑ Streptokinase 1.5 million units IV administered over 30-60 min Administer a P2Y12 inhibitor:
Administer ONE of the following anticoagulant therapy:
❑ Enoxaparin (for up to 8 days or until revascularization)
| ||||||||||||||||||||||
Consider urgent CABG if the coronary anatomy is not amenable to PCI and one of the following: ❑ Ongoing and recurrent ischemia | Transfer to a PCI-capable hospital for non primary PCI, if there is: ❑ Cardiogenic shock (Class I, level of evidence B) | ||||||||||||||||||||||
Contraindications to Fibrinolytic Therapy
Shown below is a table summarizing the absolute and relative contraindications to fibrinolytic therapy among STEMI patients.
| Absolute contraindications | Relative contraindications |
| ❑ Prior intracranial hemorrhage ❑ Ischemic stroke within the last 3 months (unless within 4.5 hours) |
❑ Oral anticoagulation therapy ❑ Pregnancy |
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[1]
Abbreviations: CABG: coronary artery bypass graft; ECG: electrocardiogram; LAD: left anterior descending; LBBB: left bundle branch block; MI: myocardial infarction; PCI: percutaneous coronary intervention; S3: third heart sound; S4: fourth heart sound; VSD: ventricular septal defect
Characterize the symptoms: ❑ Chest pain or chest discomfort
❑ Dyspnea | |||||||||
Obtain a detailed history: ❑ Age
❑ List of medications Identify possible triggers: | |||||||||
Examine the patient: Vital signs
Pulses
Skin Heart
❑ Murmurs
❑ Pericardial friction rub (suggestive of pericarditis) Signs of right ventricular MI: Lungs | |||||||||
Pre-Discharge Care
Abbreviations: ACE: angiotensin converting enzyme; LVEF: left ventricular ejection fraction; MI: myocardial infarction; PCI: percutaneous coronary intervention; PO: per os; STEMI: ST elevation myocardial infarction; VF: ventricular fibrillation; VT: ventricular tachycardia
Administer the following medications in patients without contraindications: ❑ Aspirin 81-325 mg (indefinitely)
❑ ACE inhibitor in case of anterior MI, ejection fraction ≤ 40% or heart failure
❑ Valsartan (in case of intolerance to ACE inhibitors)
❑ Atorvastatin 80 mg daily Administer antiplatelet therapy For patients who underwent PCI, for one year Manage complications of STEMI
❑ Temporary pacing for symptomatic bradycardia refractory to medical therapy (Class I, level of evidence C)
Assess the patient for ischemia: | |||||||||
Long Term Management
Abbreviations: ACE: angiotensin converting enzyme; ARB: angiotensin receptor blocker; MI: myocardial infarction
❑ Prepare a list of all the home medications and educate the patient about compliance
❑ Encourage lifestyle modification
❑ Ensure the initiation of the management of comorbidities
❑ Educate the patient about the early recognition of symptoms of MI | |||||||
Do's
- A pre-hospital ECG is recommended. If STEMI is diagnosed the PCI team should be activated while the patient is en route to the hospital.
- Administer reperfusion therapy for all patients presenting with STEMI within 12 hours of the beginning of the symptoms (Class I, level of evidence A).
- Administer a loading dose followed by a maintenance dose of clopidogrel, ticagrelor or prasugrel (if PCI is planned) as initial treatment instead of aspirin among patients with gastrointestinal intolerance or hypersensitivity reaction to aspirin.
- Administer sublingual nitroglycerin in patients with ischemic chest pain; however, administer IV nitroglycerin among patients with persistent chest pain after three sublingual nitroglycerins.[4]
- Discontinue non-steroidal anti-inflamatory drugs immediately.[5][6]
- Rule out any contraindications for fibrinolytic therapy before its administration. If contraindications to fibrinolytics are present, the patient should be transferred to another hospital where PCI is available.
- Initiate therapeutic hypothermia among comatose patients with STEMI (Class I, level of evidence B).
- Perform immediate angiography and PCI among STEMI patients who underwent resuscitation for cardiac arrest (Class I, level of evidence B).
- Consider bare-metal stent among STEMI patients with any of the following (Class I, level of evidence C):
- High bleeding risk
- Lack of compliance for a one year regimen of dual antiplatelet therapy
- Surgery or invasive procedure within the next year
- Achieve the following therapeutic activated clotting time when administering UFH:
- 200 to 250 seconds with the concomitant administration of GPIIbIIIa receptor inhibitor
- 250 to 300 seconds (HemoTec device) without the concomitant administration of a GPIIbIIIa receptor inhibitor
- 300 to 350 seconds (Hemochron device) without the concomitant administration of a GPIIbIIIa receptor inhibitor
- Make sure the dose of P2Y12 receptor inhibitors is appropriate among patients undergoing PCI after fibrinolytic therapy:
- Patients who already received a loading dose of clopidogrel: No loading dose, clopidogrel daily
- Patients who did not receive a loading dose of clopidogrel and PCI is performed ≤ 24 hours after fibrinolytic therapy: loading dose of 300 mg clopidogrel
- Patients who did not receive a loading dose of clopidogrel and PCI is performed > 24 hours after fibrinolytic therapy: loading dose of 600 mg clopidogrel
- Patients who did not receive a loading dose of clopidogrel and PCI is performed >24 hours after therapy with fibrin specific agent, or >48 hours after therapy with a non-fibrin-specific agent: prasugrel 60 mg
- Prepare the patient for urgent CABG when indicated by discontinuing the following:
- Clopidogrel or ticagrelor at least 24 hours prior to CABG
- Eptifibatide or tirofiban at least 2 to 4 hours prior to CABG
- Abciximab 12 hours prior to CABG
- Consider using a mechanical circulatory support among hemodynamically unstable patients with STEMI requiring an urgent CABG (Class IIa, level of evidence C).
- Recommend a long term maintenance dose of 81 mg of aspirin when the patient is administered ticagrelor.
- Include aldosterone antagonist in the discharge medication list among patients who are already on ACE inhibitors and beta-blockers with a left ventricular ejection fraction <40% or diabetes or heart failure.[1]
Don'ts
- Do not administer IV beta-blockers among patients with elevated risk for cardiogenic shock, signs of heart failure, low ouput state, prolonged PR interval more than 0.24 seconds, second or third degree block or asthma (Class I, level of evidence B).
- Do not administer IV GP IIb/IIIa inhibitors to patients with low risk of ischemic events or at high risk of bleeding and who are already on aspirin and P2Y12 receptor inhibitors therapy.
- Do not administer nitroglycerine to patients with systolic blood pressure < 90 mm Hg or ≥ to 30 mm Hg below baseline, severe bradycardia (< 50 bpm), tachycardia (> 100 bpm), or suspected right ventricular myocardial infarction.
- Do not delay the time for reperfusion.
- Do not administer prasugrel among patients with any of the following:
- Prior history of strokes or TIAs (Class III, Level of evidence B)
- Active pathological bleeding
- Age ≥75 years of age, (except in high-risk patients such as diabetes or prior MI, where its use may be considered)
- Urgent coronary artery bypass graft surgery (CABG) is likely
- Presence of additional risk factors for bleeding such as body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of bleeding[7]
- Do not administer fibrinolytic therapy to patients with known history of intracranial hemorrhage, cerebral arteriovenous malformation or to patients with suspected aortic dissection.
- Do not withhold aspirin among patients who are planned to undergo urgent CABG (Class I, level of evidence C).[1]
Gallery
Shown below is an EKG demonstrating the evolution of an infarct on the EKG. ST elevation, Q wave formation, T wave inversion, normalization with a persistent Q wave suggest STEMI.

Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/File:AMI_evolutie.png
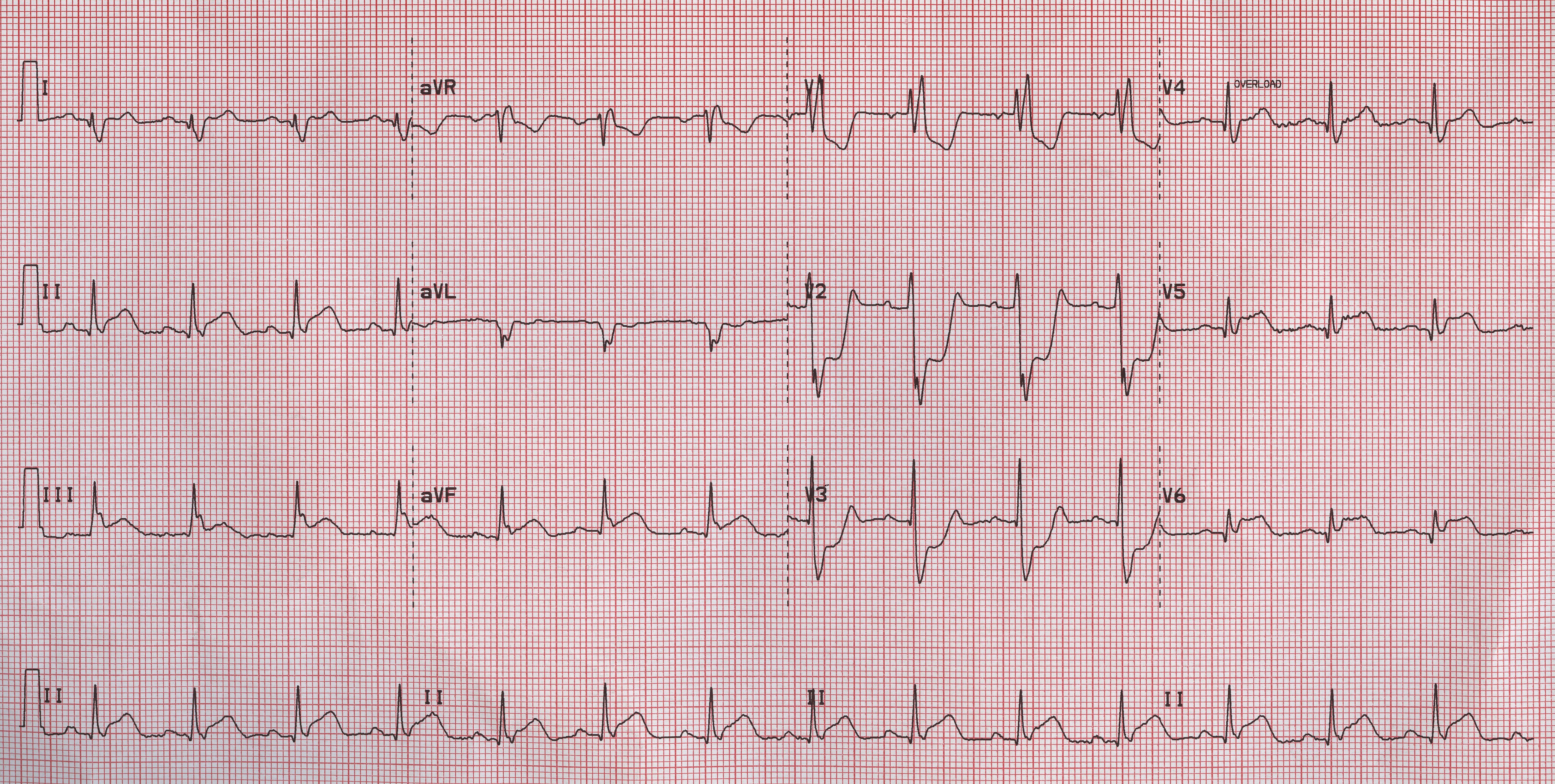
Shown below is an EKG demonstrating loss of R waves throughout the anterior wall (V1-V6). QS complexes in V3-V5. ST elevation in V1-V5 with terminal negative T waves.

Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG demonstrating ST elevation in leads II, III and aVF and ST depression in leads V1, V2 and V3 depicting a posterior MI.
Shown below is an EKG demonstrating acute MI in a patient with LBBB

Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
References
- ↑ 1.0 1.1 1.2 1.3 O'Gara, Patrick T.; Kushner, Frederick G.; Ascheim, Deborah D.; Casey, Donald E.; Chung, Mina K.; de Lemos, James A.; Ettinger, Steven M.; Fang, James C.; Fesmire, Francis M.; Franklin, Barry A.; Granger, Christopher B.; Krumholz, Harlan M.; Linderbaum, Jane A.; Morrow, David A.; Newby, L. Kristin; Ornato, Joseph P.; Ou, Narith; Radford, Martha J.; Tamis-Holland, Jacqueline E.; Tommaso, Carl L.; Tracy, Cynthia M.; Woo, Y. Joseph; Zhao, David X. (2013). "2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction". Journal of the American College of Cardiology. 61 (4): e78–e140. doi:10.1016/j.jacc.2012.11.019. ISSN 0735-1097.
- ↑ Wang-Clow F, Fox NL, Cannon CP, Gibson CM, Berioli S, Bluhmki E; et al. (2001). "Determination of a weight-adjusted dose of TNK-tissue plasminogen activator". Am Heart J. 141 (1): 33–40. doi:10.1067/mhj.2001.112092. PMID 11136484.
- ↑ Epstein AE, Dimarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS; et al. (2008). "ACC/AHA/HRS 2008 guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: executive summary". Heart Rhythm. 5 (6): 934–55. doi:10.1016/j.hrthm.2008.04.015. PMID 18534377.
- ↑ Kaplan K, Davison R, Parker M, Przybylek J, Teagarden JR, Lesch M (1983). "Intravenous nitroglycerin for the treatment of angina at rest unresponsive to standard nitrate therapy". Am J Cardiol. 51 (5): 694–8. PMID 6402912.
- ↑ Trelle S, Reichenbach S, Wandel S, Hildebrand P, Tschannen B, Villiger PM; et al. (2011). "Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis". BMJ. 342: c7086. doi:10.1136/bmj.c7086. PMC 3019238. PMID 21224324. Review in: Evid Based Med. 2011 Oct;16(5):142-3
- ↑ Coxib and traditional NSAID Trialists' (CNT) Collaboration. Bhala N, Emberson J, Merhi A, Abramson S, Arber N; et al. (2013). "Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials". Lancet. 382 (9894): 769–79. doi:10.1016/S0140-6736(13)60900-9. PMC 3778977. PMID 23726390. Review in: Ann Intern Med. 2013 Oct 15;159(8):JC12
- ↑ "http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6". Retrieved 6 February 2014. External link in
|title=(help)