Retinoblastoma differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 19: | Line 19: | ||
*[[Retinal dysplasia]] | *[[Retinal dysplasia]] | ||
*[[Medulloepithelioma]] | *[[Medulloepithelioma]] | ||
Differential diagnosis of leukocoria | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 800px;" align=center | |||
|valign=top| | |||
|+ | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Disease/Condition}} | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Clinical presentation }} | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Demographics/History}} | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Diagnosis }} | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Other notes }} | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Retinoblastoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Coats'disease (exudative retinitis or retinal telangiectasis) | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | PHPV/Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous) | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Astrocytic hamartoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Retinopathy of prematurity (ROP) | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Fundus examination: reveals gliotic-appearing retina, which is different from the retinal detachment associated with retinoblastoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Ocular toxocariasis | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Generally causes vitreoretinal traction and ocular inflammation not seen in retinoblastoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Fundus examination reveals the characteristic signs | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Hereditary retinal syndrome | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Generally causes vitreoretinal traction and ocular inflammation not seen in retinoblastoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Fundus examination reveals the characteristic signs | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* | |||
|} | |||
Differentiating features of some common and less common differential diagnosis are: | Differentiating features of some common and less common differential diagnosis are: | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 800px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 800px;" align=center | ||
| Line 27: | Line 95: | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Risk factors }} | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Risk factors }} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Unilateral/bilateral }} | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Unilateral/bilateral }} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Differentiating Signs/Symptoms }} | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Differentiating Signs/Symptoms }} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Axial length }} | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Axial length }} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Imaging findings }} | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Imaging findings }} | ||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Retinoblastoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*< 3 years of age in 90% | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Family history | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Unilateral/bilateral | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Leukocoria | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Normal | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*USG:Intraretinal/subretinal mass with calcification | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Congenital Cataract | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Congenital Cataract | ||
| Line 128: | Line 208: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Ophthalmology]] | [[Category:Ophthalmology]] | ||
Revision as of 14:47, 7 May 2019

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]: Associate Editor(s)-in-Chief: Simrat Sarai, M.D. [2]
Overview
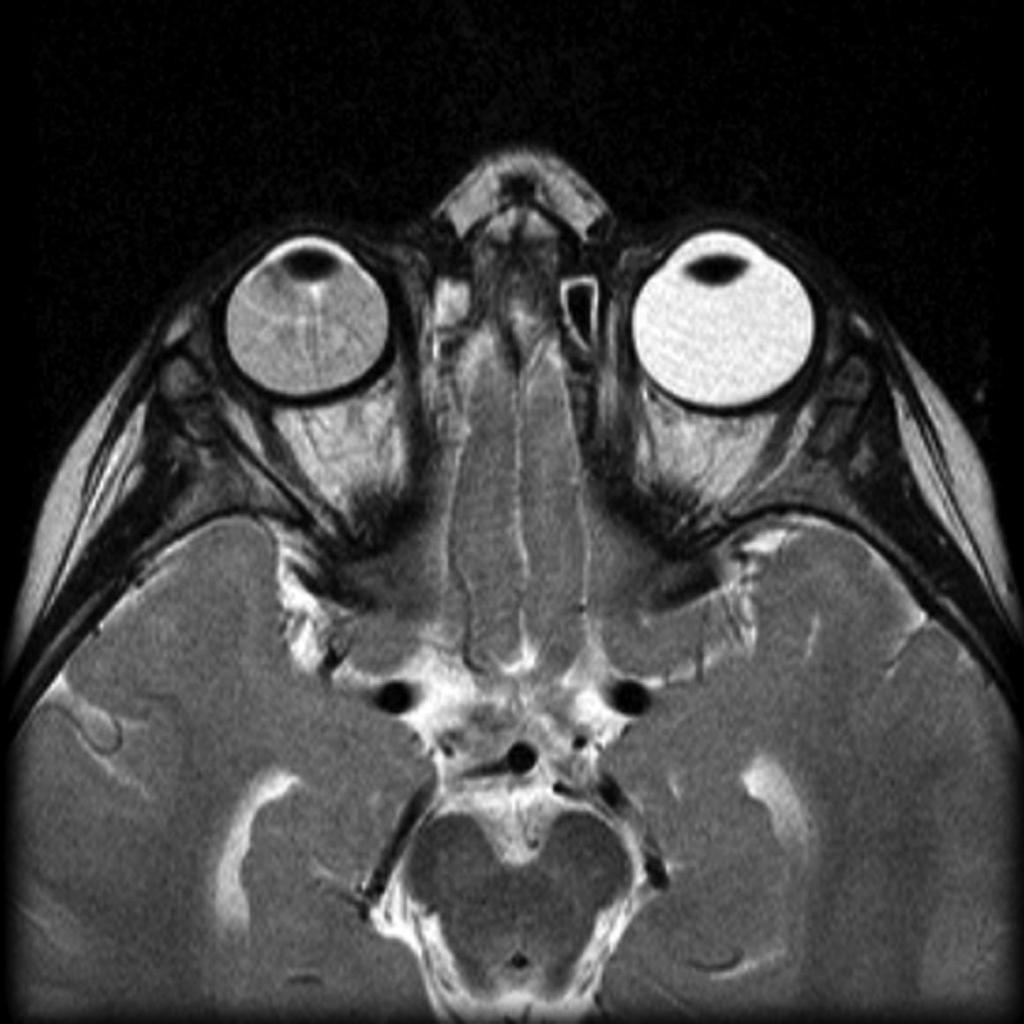
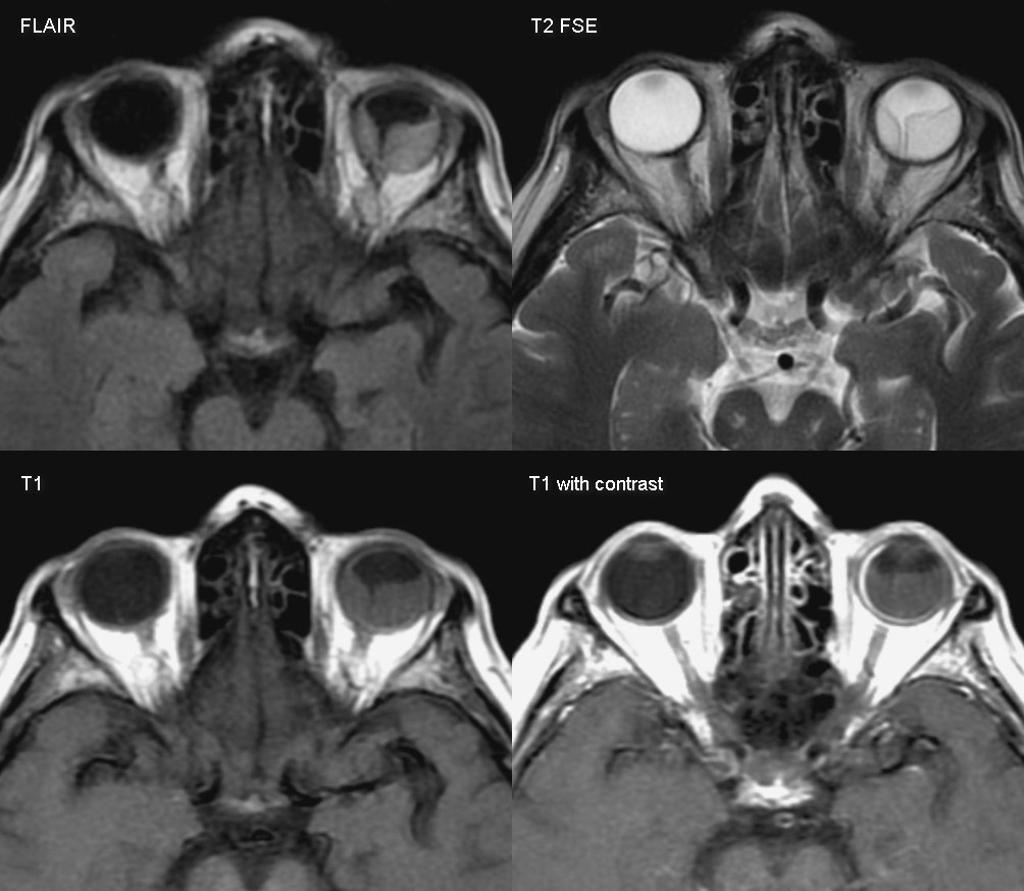
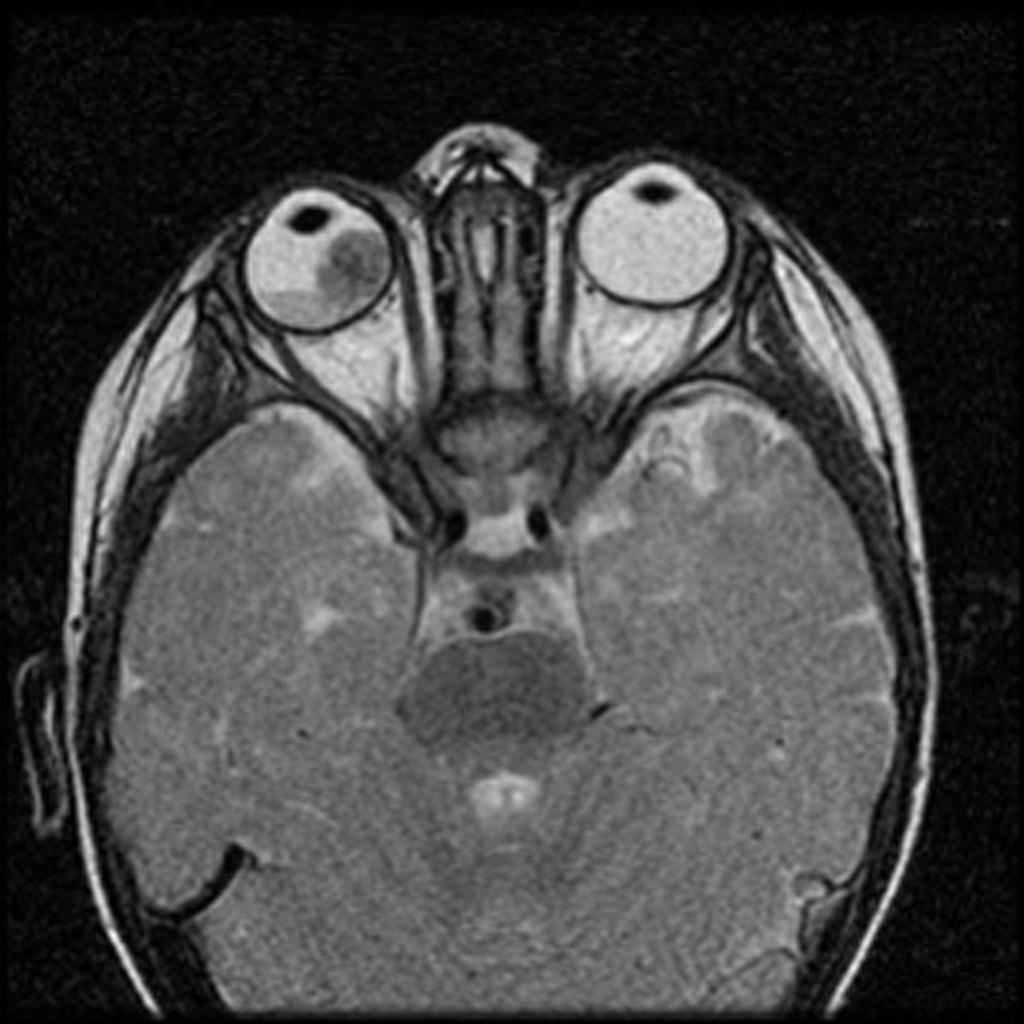
Retinoblastoma must be differentiated from other diseases that cause leukocoria such as congenital cataract, persistent fetal vasculature, Coats disease, coloboma of choroid or optic disc, toxocariasis, astrocytic hamartoma, retinopathy of prematurity, vitreous hemorrhage, uveitis, retinal dysplasia, and medulloepithelioma.[1]
Differential diagnosis
Retinoblastoma must be differentiated from other diseases that cause leukocoria. The common causes of leukocoria in children include:[1]
- Congenital cataract
- Persistent fetal vasculature
- Coats disease
Less common causes of leukocoria include:
- Coloboma of choroid or optic disc
- Toxocariasis
- Astrocytic hamartoma
- Retinopathy of prematurity (stage 4, 5)
- Vitreous hemorrhage
- Uveitis
- Retinal dysplasia
- Medulloepithelioma
Differential diagnosis of leukocoria
| Disease/Condition | Clinical presentation | Demographics/History | Diagnosis | Other notes |
|---|---|---|---|---|
| Retinoblastoma |
|
|
| |
| Coats'disease (exudative retinitis or retinal telangiectasis) |
|
|
| |
| PHPV/Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous) |
|
|
| |
| Astrocytic hamartoma |
|
|
| |
| Retinopathy of prematurity (ROP) |
|
|
| |
| Ocular toxocariasis |
|
|
|
|
| Hereditary retinal syndrome |
|
|
|
Differentiating features of some common and less common differential diagnosis are:
| Disease/Condition | Age of presentation | Risk factors | Unilateral/bilateral | Differentiating Signs/Symptoms | Axial length | Imaging findings |
|---|---|---|---|---|---|---|
| Retinoblastoma |
|
|
|
|
|
|
| Congenital Cataract |
|
| ||||
| Coats disease (exudative retinitis or retinal telangiectasis) |
|
| ||||
| Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous) |
|
| ||||
| Retinopathy of prematurity (ROP) |
|
| ||||
| Ocular toxocariasis |
|
|
| Disease | Prominent clinical feature | Radiological findings |
|---|---|---|
| Ocular cysticercosis |
|
|
| Retinal detachment |
|
|
| Hyperthyroid Ophthalmopathy |
|
|
| Retinoblastoma |
|
|
 |
 |
 |
 |
|---|
References
- ↑ 1.0 1.1 Retinoblastoma. Wikipedia(2015) https://en.wikipedia.org/wiki/Retinoblastoma#cite_note-30 Accessed on October 2, 2015
- ↑ 2.0 2.1 "How to Diagnose and Manage Coats' Disease".
- ↑ 3.0 3.1 "Management of retinal detachment: a guide for non-ophthalmologists".
- ↑ 4.0 4.1 "Thyroid Ophthalmopathy - EyeWiki".
- ↑ 5.0 5.1 "c.ymcdn.com".