Retinoblastoma differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
m (Bot: Removing from Primary care) |
||
| (14 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
[[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Retinoblastoma]] | [[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Retinoblastoma]] | ||
{{CMG}}; {{AE}} {{ | {{CMG}}; {{AE}} {{Sahar}} {{Simrat}} | ||
==Overview== | ==Overview== | ||
Retinoblastoma must be differentiated from other [[diseases]] that cause [[leukocoria]]. [[leukocoria]] may occur in several [[ocular]] [[conditions]] including [[tumors]], [[vascular]] [[disease]], [[inflammatory]] [[disorders]], and also due to [[trauma]]. | |||
== | ==Differentiating Retinoblastoma from Other Diseases== | ||
Retinoblastoma must be differentiated from other diseases that cause [[leukocoria]]. Differential diagnosis of leukocoria in children include: | Retinoblastoma must be differentiated from other [[diseases]] that cause [[leukocoria]]. [[Differential diagnosis]] of [[leukocoria]] in [[Child|children]] include: | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | | | A01 | | | | | |A01=[[Leukocoria]]}} | {{familytree | | | | | | | | | | | | | A01 | | | | | |A01=[[Leukocoria]]}} | ||
| Line 13: | Line 13: | ||
{{familytree | D01 | | | | D02 | | | | D03 | | | | D04 | | | | D05 | |D01=[[Tumors]]|D02=[[Congenital malformations]]|D03=[[Vascular]] [[diseases]]|D04=[[Inflammatory]] [[diseases]]|D05=[[Trauma]]}} | {{familytree | D01 | | | | D02 | | | | D03 | | | | D04 | | | | D05 | |D01=[[Tumors]]|D02=[[Congenital malformations]]|D03=[[Vascular]] [[diseases]]|D04=[[Inflammatory]] [[diseases]]|D05=[[Trauma]]}} | ||
{{familytree | |!| | | | | |!| | | | | |!| | | | | |!| | | | | |!| | }} | {{familytree | |!| | | | | |!| | | | | |!| | | | | |!| | | | | |!| | }} | ||
{{familytree | E01 | | | | E02 | | | | E03 | | | | E04 | | | | E05 | |E01=[[Retinoblastoma]]<br>[[Medulloepithelioma]]<br>[[Leukemia]]<br>Combined retinal [[hamartoma]]<br>[[ | {{familytree | E01 | | | | E02 | | | | E03 | | | | E04 | | | | E05 | |E01=[[Retinoblastoma]]<br>[[Medulloepithelioma]]<br>[[Leukemia]]<br>Combined retinal [[hamartoma]]<br>Astrocytic [[hamartoma]] (Bourneville’s tuberous sclerosis)|E02=[[Persistent fetal vasculature]] (PFV)<br>Posterior [[coloboma]]<br>[[Retinal fold]]<br>Myelinated nerve fibers<br>Morning glory syndrome<br>[[Retinal dysplasia]]<br>[[Norrie’s disease]]<br>Incontinentia pigmenti<br>[[Cataract]]|E03=[[Retinopathy of prematurity]] (ROP)<br>[[Coats’ disease]]<br>Familial exudative vitreoretinopathy (FEVR)|E04=[[Ocular toxocariasis]]<br>[[Congenital toxoplasmosis]]<br>Congenital [[cytomegalovirus]] [[retinitis]]<br>[[Herpes simplex]] [[retinitis]]<br>Other types of fetal iridochoroiditis<br>[[Endophthalmitis]]|E05=Intraocular [[foreign body]]<br>[[Vitreous hemorrhage]]<br>[[Retinal detachment]]}} | ||
{| | {| | ||
! colspan="2" style="background:#DCDCDC;" align="center" + |The above | ! colspan="2" style="background:#DCDCDC;" align="center" + |The above algorithm is adopted from Clinical Ophthalmic Oncology book <ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref> | ||
|- | |- | ||
|} | |} | ||
Retinoblastoma should be differentiated from the following conditions that cause [[leukocoria]]: | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 800px;" align="center" | {| style="border: 0px; font-size: 90%; margin: 3px; width: 800px;" align="center" | ||
| valign="top" | | | valign="top" | | ||
| Line 31: | Line 31: | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*[[Retinal]] [[mass]] | *[[Retinal]] [[mass]] | ||
*[[ | *[[Gross examination]] reveals a whitish [[tumor]] with prominent [[Vascular|vascularity]] | ||
*[[Vitreous]] seeding in endophytic [[tumors]] | *[[Vitreous]] seeding in endophytic [[tumors]] | ||
*[[exudative]] [[retinal detachment]] in exophytic [[tumor]] | *[[exudative]] [[retinal detachment]] in exophytic [[tumor]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Sporadic in 90% of the cases | *Sporadic in 90% of the cases | ||
*The median age of [[diagnosis]] is 18 months | *The [[median]] age of [[diagnosis]] is 18 months | ||
*[[Bilateral]] in 70% of the cases | *[[Bilateral]] in 70% of the cases | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*P/E:[[leukocoria]] | *[[Physical examination|P/E]]: [[leukocoria]] | ||
*[[Ultrasound imaging| | *[[Ultrasound imaging|Ultrasound imaging]]: | ||
** | **A dome or placoid-shaped [[Ocular|intraocular]] mass | ||
**+/-intralesional [[calcification]] | **+/- [[Lesion|intralesional]] [[calcification]] | ||
*[[CT scan|CT imaging]]: | *[[CT scan|CT imaging]]: Presence of [[calcification]] within the [[tumor]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Associated with [[13q deletion syndrome]] | *Associated with [[13q deletion syndrome]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Coats'disease<ref name="pmid22165951">{{cite journal |vauthors=Silva RA, Dubovy SR, Fernandes CE, Hess DJ, Murray TG |title=Retinoblastoma with Coats' response |journal=Ophthalmic Surg Lasers Imaging |volume=42 Online |issue= |pages=e139–43 |date=December 2011 |pmid=22165951 |doi=10.3928/15428877-20111208-04 |url=}}</ref><ref name="pmid19645389">{{cite journal |vauthors=Gupta N, Beri S, D'souza P |title=Cholesterolosis Bulbi of the Anterior Chamber in Coats Disease |journal=J Pediatr Ophthalmol Strabismus |volume= |issue= |pages= |date=June 2009 |pmid=19645389 |doi=10.3928/01913913-20090616-04 |url=}}</ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Coats disease|Coats'disease]]<ref name="pmid22165951">{{cite journal |vauthors=Silva RA, Dubovy SR, Fernandes CE, Hess DJ, Murray TG |title=Retinoblastoma with Coats' response |journal=Ophthalmic Surg Lasers Imaging |volume=42 Online |issue= |pages=e139–43 |date=December 2011 |pmid=22165951 |doi=10.3928/15428877-20111208-04 |url=}}</ref><ref name="pmid19645389">{{cite journal |vauthors=Gupta N, Beri S, D'souza P |title=Cholesterolosis Bulbi of the Anterior Chamber in Coats Disease |journal=J Pediatr Ophthalmol Strabismus |volume= |issue= |pages= |date=June 2009 |pmid=19645389 |doi=10.3928/01913913-20090616-04 |url=}}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* Yellowish appearance of [[leukocoria]] | * Yellowish appearance of [[leukocoria]] | ||
*P/E: | *[[Physical examination|P/E]]: [[Exudate|Exudative]] [[retinal detachment]] with [[vascular]] tortuosity and [[telangiectasia]] | ||
*+/- neurovascular glaucoma | *+/- neurovascular [[glaucoma]] | ||
*Absence of calcification | *Absence of [[calcification]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Sporadic in 100% of the cases | *Sporadic in 100% of the cases | ||
*Almost always unilateral | *Almost always unilateral | ||
*More common among boys | *More common among boys | ||
*The median age of diagnosis 5 to 9 years | *The [[median]] age of [[diagnosis]] 5 to 9 years | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*P/E is diagnostic in most of the cases | *[[Physical Examination|P/E]] is [[Diagnosis|diagnostic]] in most of the cases | ||
*Ultrasound | *[[Ultrasound imaging]]: | ||
**Complete retinal detachment | **Complete [[retinal detachment]] | ||
**Absence of calcification | **Absence of [[calcification]] | ||
**Exudative, mobile lipid material under retina | **[[Exudate|Exudative]], mobile [[lipid]] material under [[retina]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Fluorescein | *[[Fluorescein angiography]] reveals characteristic [[telangiectasias]] of small to medium-sized [[retinal]] [[Blood vessel|vessels]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous)<ref name="pmid19645389">{{cite journal |vauthors=Gupta N, Beri S, D'souza P |title=Cholesterolosis Bulbi of the Anterior Chamber in Coats Disease |journal=J Pediatr Ophthalmol Strabismus |volume= |issue= |pages= |date=June 2009 |pmid=19645389 |doi=10.3928/01913913-20090616-04 |url=}}</ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous)<ref name="pmid19645389">{{cite journal |vauthors=Gupta N, Beri S, D'souza P |title=Cholesterolosis Bulbi of the Anterior Chamber in Coats Disease |journal=J Pediatr Ophthalmol Strabismus |volume= |issue= |pages= |date=June 2009 |pmid=19645389 |doi=10.3928/01913913-20090616-04 |url=}}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Presence of leukocoria in infancy which commonly accompanied | *Presence of [[leukocoria]] in [[infancy]] which is commonly accompanied by [[microphthalmia]] | ||
* | *Presence of retrolental fibrovascular [[Tissue (biology)|tissue]] | ||
*+/- secondary cataract | *+/- secondary [[cataract]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Sporadic in the majority of cases | *Sporadic in the majority of cases | ||
*Always congenital (present at birth) | *Always [[congenital]] (present at birth) | ||
*Rarely bilateral | *Rarely [[bilateral]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*P/E:microphthalmia and intraocular pressure | *[[Physical examination|P/E]]: [[microphthalmia]] and increased[[intraocular pressure]] | ||
* | *Presence of elongated [[ciliary processes]] contracting into the retrolental mass | ||
*Ultrasound imaging: | *[[Ultrasound imaging]]: | ||
**Vitreous band from lens to optic nerve | **[[Vitreous]] band from [[Lens (anatomy)|lens]] to [[optic nerve]] | ||
**Short axial length of eyes | **Short axial length of [[Eye|eyes]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Bilateral cases has been accompanied | *[[Bilateral]] cases has been accompanied by[[protein C deficiency]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Astrocytic hamartoma<ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Astrocytic [[hamartoma]]<ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Presence of gray-yellow or translucent tumors involving the posterior pole near optic nerve | *Presence of gray-yellow or translucent [[tumors]] involving the [[Anatomical terms of location|posterior]] pole near [[optic nerve]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Presents at any age | *Presents at any age | ||
*Some has been associated with neurofibromatosis type 1/tuberous sclerosis | *Some has been associated with [[neurofibromatosis type 1]]/[[tuberous sclerosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*P/E: | *[[Physical Examination|P/E]]: A sessile shape [[tumor]] arising from the inner aspect of the [[Sensory system|sensory]] [[retina]] | ||
*Presence of small areas of calcification/complete calcification in older patients | *Presence of small areas of [[calcification]]/complete [[calcification]] in older [[Patient|patients]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Reticular pattern of fine blood vessels | *Reticular pattern of fine [[Blood vessel|blood vessels]] on [[fluorescein angiography]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Retinopathy of prematurity (ROP)<ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | [[Retinopathy of prematurity|Retinopathy of prematurity (ROP)]]<ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Absence of calcification | *Absence of [[calcification]] | ||
*Presence of retinal contraction in one or both eyes | *Presence of [[retinal]] contraction in one or both [[Eye|eyes]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*History of: | *History of: | ||
**Prematurity (<32 weeks gestation) | **[[Prematurity]] (< 32 weeks [[gestation]]) | ||
**Low birth weight (<1.5 kg) | **[[Low birth weight]] (< 1.5 kg/3.3 lbs) | ||
**Oxygen supplementation | **[[Oxygen]] supplementation | ||
*Leukocoria is | *[[Leukocoria]] is a late presentation of the [[disease]] | ||
*Always bilateral | *Always [[bilateral]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*P/E:Bilateral retinal avascularity and | *[[Physical Examination|P/E]]: [[Bilateral]] [[retinal]] [[Vascularity|avascularity]] and non-[[perfusion]] in [[temporal]] peripheral [[retina]] with fibrovascular proliferation in advanced cases | ||
*Ultrasound imaging: | *[[Ultrasound imaging|Ultrasound imaging:]] | ||
**Retinal detachment with retinal bands | **[[Retinal detachment]] with [[retinal]] bands | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Short axial length of eyes | *Short axial length of [[Eye|eyes]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Ocular toxocariasis <ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | [[Toxocariasis|Ocular toxocariasis]] <ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Presence of retinal and/or vitreous traction in approximately all the cases | *Presence of [[retinal]] and/or [[vitreous]] traction in approximately all of the cases | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Presents at any age | *Presents at any age | ||
*Mostly unilateral | *Mostly unilateral | ||
*Ingestion of larvae leads to the infection | *[[Ingestion]] of larvae leads to the [[infection]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*P/E: | *[[Physical Examination|P/E]]: Presence of [[granuloma]] and [[retinal]] traction | ||
*Ultrasound imaging: | *[[Ultrasound imaging]]: | ||
**Peripheral mass | **Peripheral [[mass]] | ||
**Vitreoretinal band | **Vitreoretinal band | ||
**Traction retinal detachment | **Traction [[retinal detachment]] | ||
*Presence of eosinophils in the anterior chamber tap | *Presence of [[eosinophils]] in the [[anterior chamber]] tap | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Classified into three | *[[Classification|Classified]] into three sub-types: | ||
**Macular granuloma | **[[Macular]] [[granuloma]] | ||
**Peripheral granuloma | **Peripheral [[granuloma]] | ||
**Endophthalmitis | **[[Endophthalmitis]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Familial Exudative Vitreoretinopathy (FEVR)<ref>{{cite book | last = Gerstenblith | first = Adam | title = The Wills eye manual : office and emergency room diagnosis and treatment of eye disease | publisher = Wolters Kluwer/Lippincott Williams & Wilkins | location = Philadelphia | year = 2012 | isbn = 978-1451109382 }}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *Presents at birth | ||
*The majority are [[asymptomatic]] | |||
* | *May present with [[leukocoria]], [[strabismus]], and [[vision loss]] | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *[[Autosomal dominant]] pattern of [[Heredity|inheritance]] | ||
*May occur sporadically | |||
*Findings include asymmetry of both [[Eye|eyes]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *[[Physical examination|P/E]]: [[Vascularity|Avascularity]] of the [[temporal]] [[retina]] with peripheral fibrovascular proliferation | ||
*[[Fluorescein angiography]]: Peripheral non-[[perfusion]] of the [[fundus]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *[[Fundus]] findings are similar to [[retinopathy of prematurity]] except for the history of [[prematurity]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | [[Norrie disease|Norrie’s Disease]]<ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref><ref name="pmid5897773">{{cite journal |vauthors=Howard GM, Ellsworth RM |title=Differential diagnosis of retinoblastoma. A statistical survey of 500 children. I. Relative frequency of the lesions which simulate retinoblastoma |journal=Am. J. Ophthalmol. |volume=60 |issue=4 |pages=610–8 |date=October 1965 |pmid=5897773 |doi= |url=}}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Presents | *Presents with [[microcephaly]], congenital [[blindness]], [[deafness]], and progressive [[neuropsychiatric]] illness | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *[[X-linked|X-linked disorder]] | ||
*More common in [[Male|males]] | |||
|- | |||
| | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *[[Physical exam|P/E]]: [[bilateral]] [[retinal]] [[dysplasia]], sometimes with [[Anatomical terms of location|anterior]] segment abnormalities and [[microphthalmia]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
- | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | [[Coloboma]]<ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *Presents at [[birth]] | ||
*Failure of the [[embryonic]] fissure to close completely results in an absence of normal [[retina]] and [[choroid]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *The majority are sporadic | ||
* | *[[Congenital disorder]] that affects [[male]] and [[female]] equally | ||
*May be unilateral or [[bilateral]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *[[Physical exam|P/E]]: Whitish depressed [[lesion]] of [[retina]] which is typically inferonasal and its margins may encompass the [[macula]] or [[optic nerve]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | *It may be accompanied by [[CHARGE syndrome]] | ||
|} | |} | ||
{| class="wikitable" | {| class="wikitable" | ||
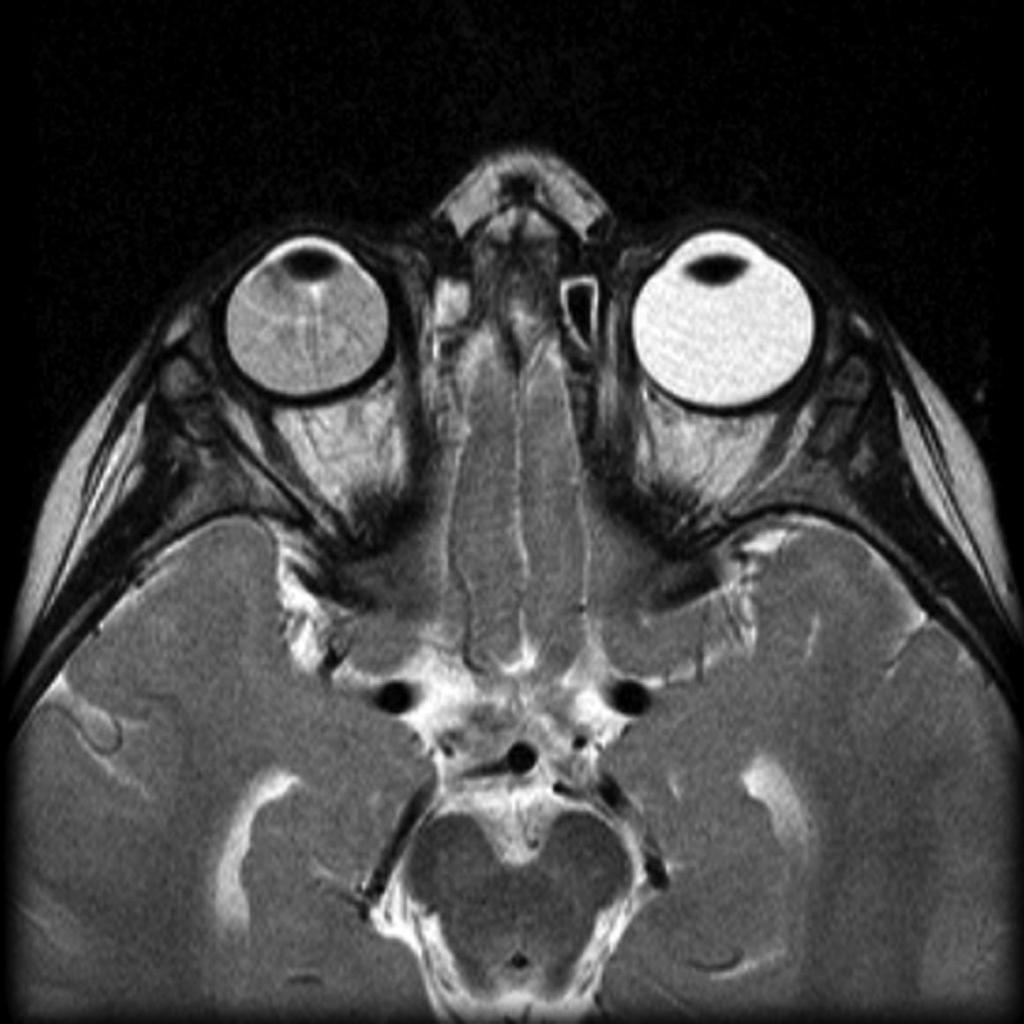
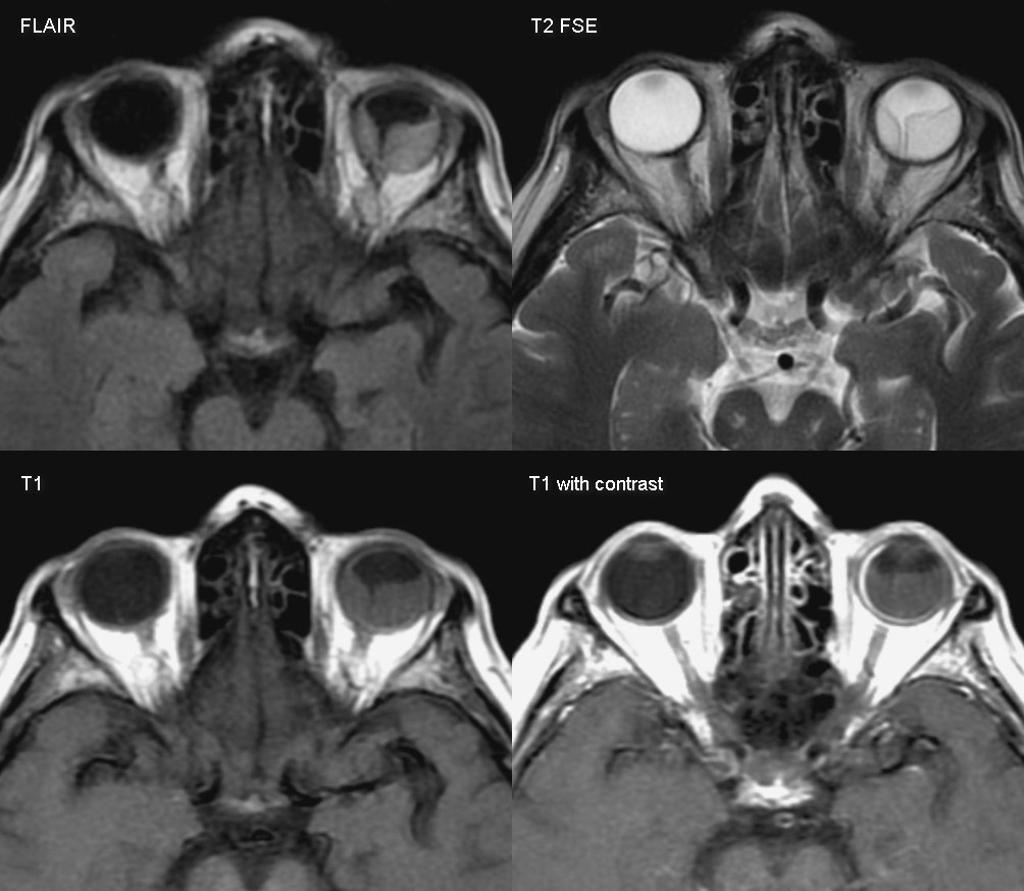
![[Image:Coats-disease-of-the-eye.jpg|center|300px|thumb|[[Magnetic resonance imaging|MRI]] of the [[Orbit (anatomy)|orbit]] showing [[Coats disease]] - Case courtesy of Dr Michael Sargent, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/6089]] | |||
! | |||
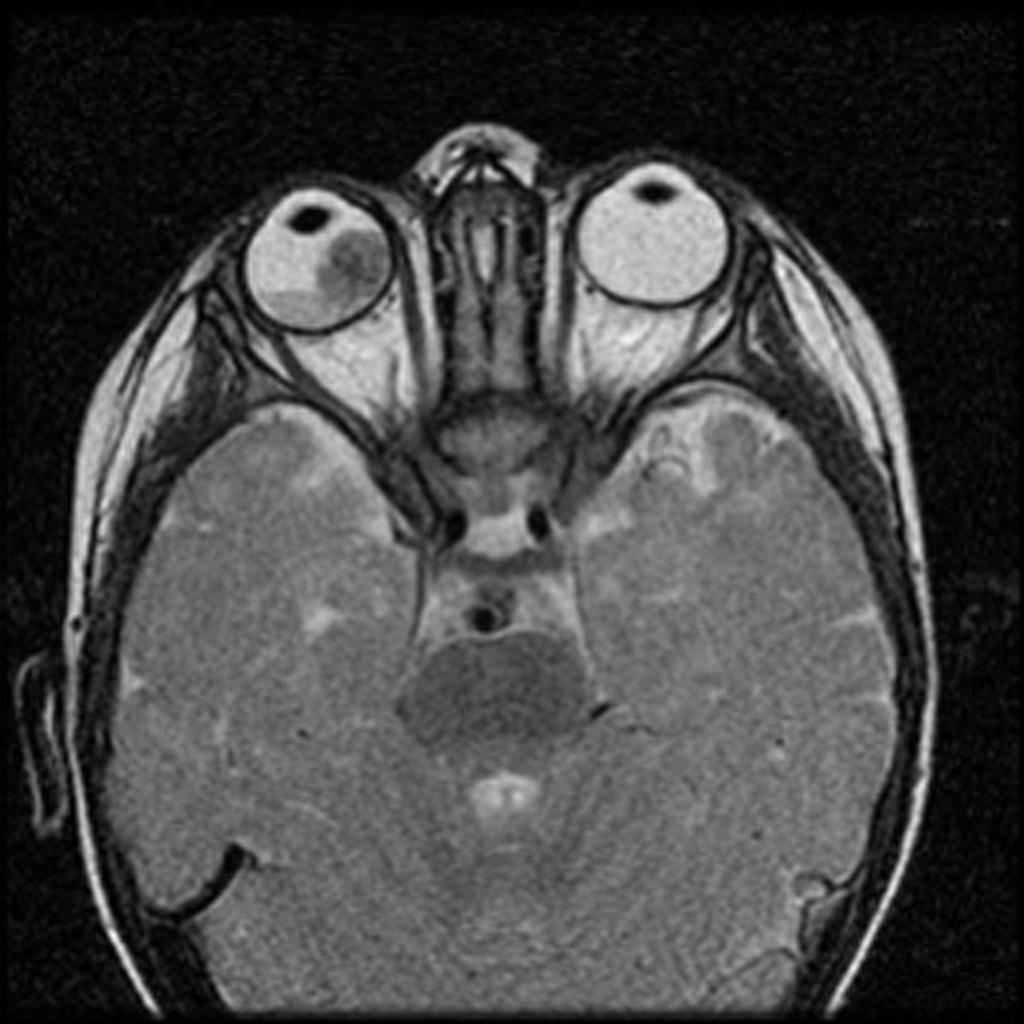
![[Image:Retinal-detachment-1.jpg|center|300px|thumb|MRI of the orbit showing retinal detachment - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/3134]] | ![[Image:Retinal-detachment-1.jpg|center|300px|thumb|MRI of the orbit showing retinal detachment - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/3134]] | ||
| Line 264: | Line 188: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
| |||
[[Category:Medicine]] | |||
[[Category:Oncology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Surgery]] | |||
Latest revision as of 23:59, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sahar Memar Montazerin, M.D.[2] Simrat Sarai, M.D. [3]
Overview
Retinoblastoma must be differentiated from other diseases that cause leukocoria. leukocoria may occur in several ocular conditions including tumors, vascular disease, inflammatory disorders, and also due to trauma.
Differentiating Retinoblastoma from Other Diseases
Retinoblastoma must be differentiated from other diseases that cause leukocoria. Differential diagnosis of leukocoria in children include:
| Leukocoria | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Tumors | Congenital malformations | Vascular diseases | Inflammatory diseases | Trauma | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Retinoblastoma Medulloepithelioma Leukemia Combined retinal hamartoma Astrocytic hamartoma (Bourneville’s tuberous sclerosis) | Persistent fetal vasculature (PFV) Posterior coloboma Retinal fold Myelinated nerve fibers Morning glory syndrome Retinal dysplasia Norrie’s disease Incontinentia pigmenti Cataract | Retinopathy of prematurity (ROP) Coats’ disease Familial exudative vitreoretinopathy (FEVR) | Ocular toxocariasis Congenital toxoplasmosis Congenital cytomegalovirus retinitis Herpes simplex retinitis Other types of fetal iridochoroiditis Endophthalmitis | Intraocular foreign body Vitreous hemorrhage Retinal detachment | |||||||||||||||||||||||||||||||||||||||||||||||||||
| The above algorithm is adopted from Clinical Ophthalmic Oncology book [1] |
|---|
Retinoblastoma should be differentiated from the following conditions that cause leukocoria:
| Disease/Condition | Clinical presentation | Demographics/History | Diagnosis | Other notes |
|---|---|---|---|---|
| Retinoblastoma[2][3] |
|
|
| |
| Coats'disease[4][5] |
|
|
| |
| Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous)[5] |
|
|
|
|
| Astrocytic hamartoma[1] |
|
|
|
|
| Retinopathy of prematurity (ROP)[1] |
|
|
|
|
| Ocular toxocariasis [1] |
|
| ||
| Familial Exudative Vitreoretinopathy (FEVR)[6] |
|
|
|
|
| Norrie’s Disease[1][7] |
|
|
- | |
| Coloboma[1] |
|
|
|
 |
 |
 |
 |
|---|
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Singh, Arun (2015). Clinical ophthalmic oncology : retinoblastoma. Heidelberg: Springer. ISBN 978-3-662-43451-2.
- ↑ Butros LJ, Abramson DH, Dunkel IJ (March 2002). "Delayed diagnosis of retinoblastoma: analysis of degree, cause, and potential consequences". Pediatrics. 109 (3): E45. PMID 11875173.
- ↑ Sachdeva R, Schoenfield L, Marcotty A, Singh AD (June 2011). "Retinoblastoma with autoinfarction presenting as orbital cellulitis". J AAPOS. 15 (3): 302–4. doi:10.1016/j.jaapos.2011.02.013. PMID 21680213.
- ↑ Silva RA, Dubovy SR, Fernandes CE, Hess DJ, Murray TG (December 2011). "Retinoblastoma with Coats' response". Ophthalmic Surg Lasers Imaging. 42 Online: e139–43. doi:10.3928/15428877-20111208-04. PMID 22165951.
- ↑ 5.0 5.1 Gupta N, Beri S, D'souza P (June 2009). "Cholesterolosis Bulbi of the Anterior Chamber in Coats Disease". J Pediatr Ophthalmol Strabismus. doi:10.3928/01913913-20090616-04. PMID 19645389.
- ↑ Gerstenblith, Adam (2012). The Wills eye manual : office and emergency room diagnosis and treatment of eye disease. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. ISBN 978-1451109382.
- ↑ Howard GM, Ellsworth RM (October 1965). "Differential diagnosis of retinoblastoma. A statistical survey of 500 children. I. Relative frequency of the lesions which simulate retinoblastoma". Am. J. Ophthalmol. 60 (4): 610–8. PMID 5897773.