PCI complications: access site complications: Difference between revisions
(→Venous) |
No edit summary |
||
| Line 26: | Line 26: | ||
*[[Subclavian]] | *[[Subclavian]] | ||
==Patients at High Risk for Access Site Complications== | ===Patients at High Risk for Access Site Complications=== | ||
*[[Obesity]] | *[[Obesity]] | ||
| Line 35: | Line 35: | ||
*Patients who undergone prior puncture | *Patients who undergone prior puncture | ||
*Patients with advanced peripheral [[arteriosclerosis]] | *Patients with advanced peripheral [[arteriosclerosis]] | ||
*Patients who suffer from coagulopathy or those taking [[anticoagulant]] or antiplatelet agents | *Patients who suffer from [[coagulopathy]] or those taking [[anticoagulant]] or [[antiplatelet]] agents | ||
*Patients with excessive [[edema]] | *Patients with excessive [[edema]] | ||
==Possible Complications== | ===Possible Complications=== | ||
*Local [[tissue]] trauma or damage (e.g., [[bleeding]] into surrounding tissues, [[nerve injury]]) | |||
*Local tissue trauma or damage (e.g., bleeding into surrounding tissues, nerve injury) | *[[Vascular]] damage (e.g., perforation, [[dissection]]) | ||
*Vascular damage (e.g., perforation, [[dissection]]) | *[[AV fistula]]: If the [[femoral artery]] and the [[vein]] are both used, [[artery|arterial]] sheath should be removed first and then the [[venous]] one to decrease risk of [[arteriovenous fistula]] formation. | ||
*AV fistula: If the [[femoral artery]] and the vein are both used, arterial sheath should be removed first and then the venous one to decrease risk of [[arteriovenous fistula]] formation. | *[[Infection]] and [[sepsis]]: After [[hemostasis]] is obtained the access area should be cleaned with [[antiseptic]] solution. | ||
*[[Infection]] and [[sepsis]]: After [[hemostasis]] is obtained the access area should be cleaned with antiseptic solution. | |||
*Aberrant catheter placement | *Aberrant catheter placement | ||
<br> | <br> | ||
Revision as of 19:28, 10 January 2013
|
Percutaneous coronary intervention Microchapters |
|
PCI Complications |
|---|
|
PCI in Specific Patients |
|
PCI in Specific Lesion Types |
|
PCI complications: access site complications On the Web |
|
American Roentgen Ray Society Images of PCI complications: access site complications |
|
Directions to Hospitals Treating Percutaneous coronary intervention |
|
Risk calculators and risk factors for PCI complications: access site complications |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Vascular access site complications are common during cardiac catheterization and PCI, and local bleeding (a local hematoma formation) is the most common one. A thoughtful and systematic approach to the catheterization procedure decreases problems of access.
Access Site Complications
An old cathlab saying Take time to evaluate and do it right the first time should always be remembered.
Complications for vascular access can be divided into acute (during the insertion period or shortly after) or long term. Operators should have a thorough knowledge of the anatomy and of the potential complications from the procedure to identify and quickly treat any complications that may arise. Access through synthetic peripheral vascular grafts should be avoided if possible.
The femoral artery approach is the most frequent site of vascular access during invasive cardiac procedures. Possible vascular access routes are as follow:
Arterial
- Axillary
- Brachial
- Femoral
- Radial (rarely used for cardiac catheterization, more common for diagnostic angiographies and percutaneous interventions)
- Subclavian (not used for cardiac catheterization)
- Translumbar (not used for cardiac catheterization)
Venous
Patients at High Risk for Access Site Complications
- Obesity
- Patients with high blood pressure
- Elderly
- Female gender
- Patients with aortic insufficiency
- Patients who undergone prior puncture
- Patients with advanced peripheral arteriosclerosis
- Patients who suffer from coagulopathy or those taking anticoagulant or antiplatelet agents
- Patients with excessive edema
Possible Complications
- Local tissue trauma or damage (e.g., bleeding into surrounding tissues, nerve injury)
- Vascular damage (e.g., perforation, dissection)
- AV fistula: If the femoral artery and the vein are both used, arterial sheath should be removed first and then the venous one to decrease risk of arteriovenous fistula formation.
- Infection and sepsis: After hemostasis is obtained the access area should be cleaned with antiseptic solution.
- Aberrant catheter placement
-
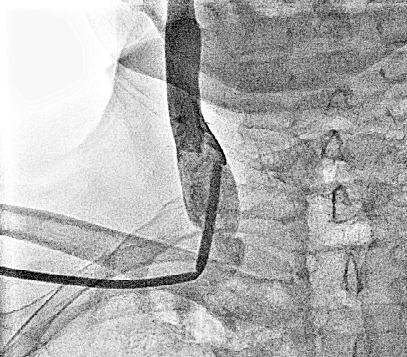
Complication during subclavian vein cannulation. Image courtesy of C. Michael Gibson and copylefted.
-
Normal anatomic position of subclavian vein
-
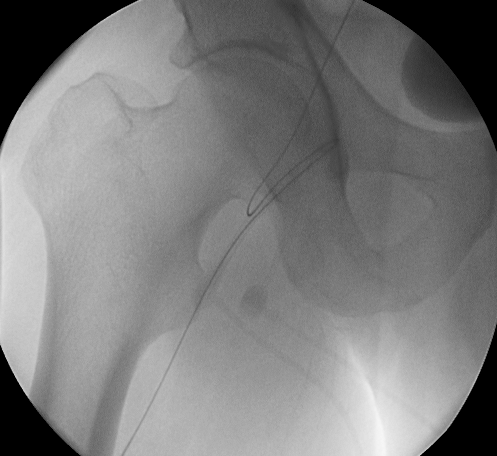
Complication during right femoral artery puncture. Image courtesy of C. Michael Gibson and copylefted.
-
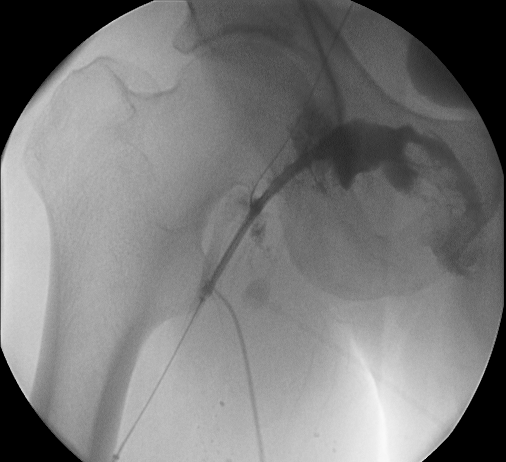
Complication during right femoral artery puncture. Image courtesy of C. Michael Gibson and copylefted.
-
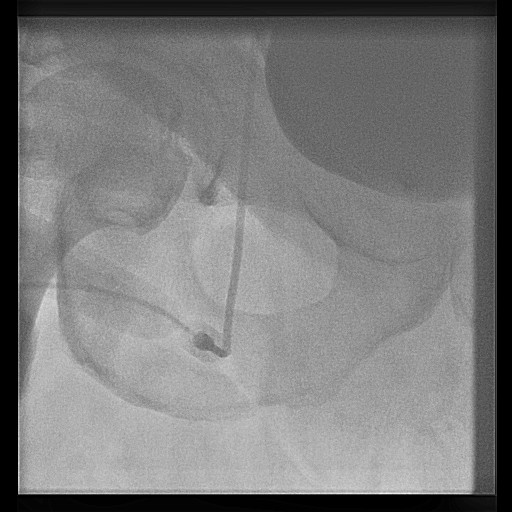
Complication of pulling out when there was resistance in a stent graft system. Part of right iliac and femoral arteries stripped with stent graft system from right femoral artery puncture site. Image courtesy of C. Michael Gibson and copylefted.
-
Higher Level Puncture of Femoral Artery and Cannula Kinking. Image courtesy of C. Michael Gibson and copylefted.