Ovarian cancer pathophysiology
|
Ovarian cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ovarian cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Ovarian cancer pathophysiology |
|
Risk calculators and risk factors for Ovarian cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Ovarian cancer is often diagnosed late resulting in a poor overall outcome for the patient. Pathological findings, therefore, often only occur in advanced symptomatic onset and tend to present more as severe pathologic outcomes.
Pathophysiology
Clear Cell Tumor
- Clear cell tumors are part of the surface epithelial-stromal tumor group of Ovarian cancers, accounting for 6% of all neoplastic cases. Clear cell tumors are also associated with the pancreas and salivary glands.
- Benign and borderline variants of this neoplasm are rare, and most cases are malignant.
- Typically, they are cystic neoplasms with polypoid masses that protrude into the cyst.
Endometrioid Tumor
Endometrioid tumors are part of the surface epithelial tumor group of ovarian neoplasms (10-20% of which are the endometrioid type). Benign and borderline variants are rare, as the majority are malignant. There is an association with endometriosis and concurrent primary endometrial carcinoma (endometrial cancer).
Gross Patholgy
| Ovarian Carcinomas Subtype | Features on Gross Pathology |
| ovarian serous cystadenocarcinoma |
Typically solid with multiple cystic areas. Often >10 cm. |
| ovarian mucinous cystadenocarcinoma |
|
| Endometrioid carcinoma of the ovary |
|
Microscopic Pathology
Histologic subtypes of epithelial ovarian tumor include:[1][2][3][4]
- Surface epithelial stromal ovarian tumor (60-70%)
- ovarian serous tumor
- ovarian serous cystadenoma: ~60% of serous tumor
- ovarian borderline serous cystadenoma: ~15% of serous tumor
- ovarian serous cystadenocarcinoma: ~25% of serous tumor; commonest malignant ovarian tumour
- ovarian mucinous tumor: ~20% of all ovarian tumor
- ovarian mucinous cystadenoma: ~80% of mucinous tumor
- ovarian bordeline mucinous cystadenoma: 10-15% of mucinous tumor
- ovarian mucinous cystadenocarcinoma: 5-10% of mucinous tumor
- ovarian endometrioid tumour: 8-15% of all ovarian tumor
- clear cell ovarian carcinoma: ~5% of ovarian cancer
- Brenner tumour: ~2.5% of ovarian epithelial neoplasms
- squamous cell carcinoma of the ovary
- ovarian cystadenofibroma / ovarian adenofibroma: can be serous, mucinous, endometrioid, clear cell or mixed
- ovarian cystadenocarcinofibroma: extremely rare
- undifferentiated carcinoma of the ovary: ~4% of all ovarian tumor
| Vulvar Carcinomas Subtype | Features on Histopathological Microscopic Analysis | Image |
| Ovarian serous cystadenocarcinoma |
|
|
| Ovarian mucinous cystadenocarcinoma |
|
|
| Endometrioid carcinoma of the ovary |
|
Clear cell tumor
Clear cell tumors can be either clear cell adenocarcinomas or clear cell sarcomas.On microscopic pathological examination, they are composed of cells with clear cytoplasm (that contains glycogen) and hob nail cells (from which the glycogen has been secreted).The pattern may be glandular, papillary or solid.
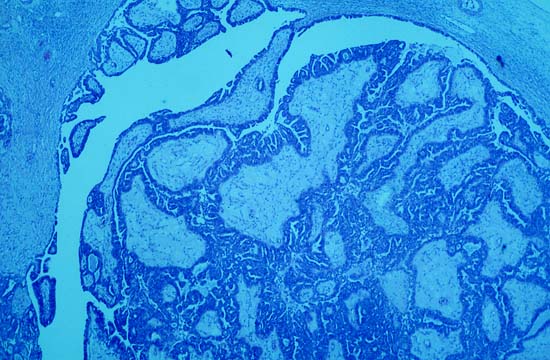
Shown below is an image of Overian clear cell adenocarcinoma.(H&E stain,very high mag)
-
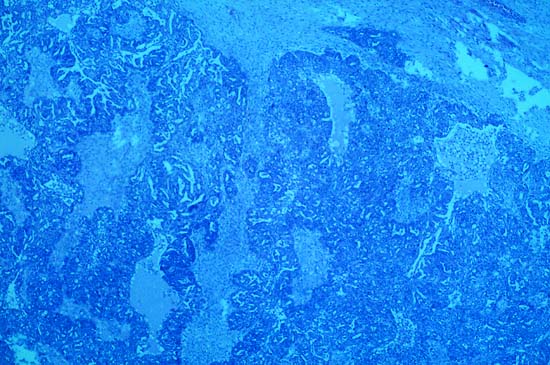
Photomicrograph is from the solid / papillary right ovarian tumor. As shown in this photo, much of the tumor had a papillary pattern with exuberant epithelial proliferation but no obvious stromal invasion. Other areas, such as the one depicted in the second photo, show extensive stromal invasion, the criterion upon which rests the diagnosis of frank malignancy.
-
Extensive stromal invasion, the criterion upon which rests the diagnosis of frank malignancy
-
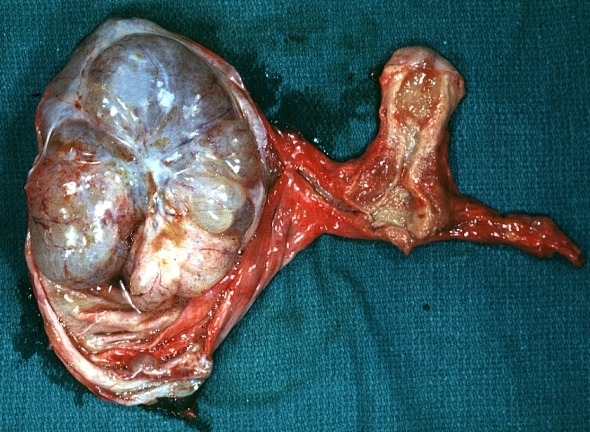
In this TAH-BSO specimen, the right ovary (on the left of the image) has been replaced by a solid serous carcinoma. The contralateral ovarian tumor is grossly cystic and could be termed a "cystadenocarcinoma." The patient had omental metastases and positive peritoneal fluid cytology. This cancer, which was discovered at exploratory laparotomy, apparently developed very rapidly; the patient had a normal pelvic ultrasound exam only 2 months before. (Courtesy of Ed Uthman, MD)
-
Ovary: Mucinous cystadenocarcinoma: Gross, an excellent image of uterus is in picture and thus illustrates the very large size of the ovarian tumor.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
Ovary: Clear cell carcinoma]
Video
Shown below is a video of clear cell adenocarcinoma of the vagina.
{{#ev:youtube|qO2w8VLf690}}
References
- ↑ Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. ISBN 9780071716727.
- ↑ Malignant melanoma. Libre pathology. http://librepathology.org/wiki/index.php/Malignant_melanoma. URL Accessed on September 30, 2015
- ↑ Basal cell carcinoma . Libre pathology. http://librepathology.org/wiki/index.php/Basal_cell_carcinoma. URL Accessed on September 30, 2015
- ↑ Squamous cell carcinoma. Libre pathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma. URL Accessed on September 30, 2015

![Ovary: Clear cell carcinoma]](/images/3/34/800px-Ovarian_clear_cell_carcinoma_-_very_high_mag.jpg)