Ovarian cancer pathophysiology: Difference between revisions
No edit summary |
|||
| (35 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{ovarian cancer}} | ||
{{CMG}} | {{CMG}}; {{AE}} {{Hudakarman}} | ||
==Overview== | ==Overview== | ||
Ovarian cancer is | [[Ovarian cancer]] is usually [[Diagnosis|diagnosed]] late resulting in a poor overall outcome for the [[patient]]. [[Pathological]] findings, therefore, often only occur in [[advanced]] symptomatic onset and tend to present more as severe pathologic outcomes. | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Clear Cell Tumor=== | |||
* Clear cell [[tumor]]s are part of the [[surface epithelial-stromal tumor]] group of [[ovarian cancer]]s, accounting for 6% of all neoplastic cases. Clear cell tumors are also associated with the [[pancreas]] and [[salivary glands]]. | |||
* [[Benign]] and borderline variants of this [[neoplasm]] are rare, and most cases are [[malignant]]. | |||
* Typically, they are [[cystic]] [[neoplasms]] with polypoid [[masses]] that protrude into the [[cyst]]. | |||
===Endometrioid Tumor=== | |||
[[Endometrioid tumor|Endometrioid tumors]] are part of the [[surface epithelial-stromal tumor|surface epithelial]] [[tumor]] group of [[Ovarian cancer|ovarian neoplasm]]s (10-20% of which are the [[Endometrium|endometrioid]] type). [[Benign]] and borderline variants are rare, as the majority are [[malignant]]. There is an association with [[endometriosis]] and concurrent primary [[endometrial carcinoma]] ([[endometrial cancer]]). | |||
===Gross Patholgy=== | |||
{| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Ovarian Carcinomas Subtype'''}} | |||
==Gross Patholgy== | |||
{| {{table}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Gross Pathology'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Gross Pathology'''}} | ||
|- | |- | ||
| | |[[Ovarian]] [[serous]] cystadenocarcinoma|| | ||
* Ovarian mass. | *[[Ovarian mass]]. | ||
* Typically solid with multiple cystic areas. | |||
* Often >10 cm. | |||
|- | |- | ||
| | |[[Ovarian]] [[mucinous cystadenocarcinoma]]|| | ||
*Multiloculated. | *Multiloculated. | ||
* Sticky, gelatinous fluid (glycoprotein). | * Sticky, gelatinous fluid (glycoprotein). | ||
* +/-Necrosis. | * +/- [[Necrosis]]. | ||
* Typically unilateral. | * Typically unilateral. | ||
| | |- | ||
|[[Endometrial cancer|Endometrioid]] [[carcinoma]] of the [[ovary]]|| | |||
* | * Usually solid and [[Cyst|cystic]], bilateral | ||
|- | |- | ||
|} | |} | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
Histologic subtypes of epithelial ovarian tumor | [[Histologic]] subtypes of [[epithelial ovarian tumor]] include:<ref>{{cite book | last = Hoffman | first = Barbara | title = Williams gynecology | publisher = McGraw-Hill Medical | location = New York | year = 2012 | isbn = 9780071716727 }}</ref><ref>Malignant melanoma. Libre pathology. http://librepathology.org/wiki/index.php/Malignant_melanoma. URL Accessed on September 30, 2015</ref><ref>Basal cell carcinoma | ||
. Libre pathology. http://librepathology.org/wiki/index.php/Basal_cell_carcinoma. URL Accessed on September 30, 2015</ref><ref>Squamous cell carcinoma. Libre pathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma. URL Accessed on September 30, 2015</ref> | |||
. Libre pathology. http://librepathology.org/wiki/index.php/Basal_cell_carcinoma. URL Accessed on September 30, 2015</ref><ref> Squamous cell carcinoma. Libre pathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma. URL Accessed on September 30, 2015</ref> | |||
* '''Surface epithelial stromal ovarian tumor''' (60-70%) | * '''Surface epithelial stromal ovarian tumor''' (60-70%) | ||
:* | |||
::* | :*'''Ovarian serous tumor''' | ||
::* | ::* Ovarian serous cystadenoma: ~60% of serous tumor | ||
::* | ::* Ovarian borderline serous cystadenoma: ~15% of serous tumor | ||
:* | ::* Ovarian serous cystadenocarcinoma: ~25% of serous tumor. Commonest malignant ovarian tumor | ||
::* | :*'''Ovarian mucinous tumor''': ~20% of all ovarian tumor | ||
::* | ::* Ovarian mucinous cystadenoma: ~80% of mucinous tumor | ||
::* | ::* Ovarian bordeline mucinous cystadenoma: 10-15% of mucinous tumor | ||
:* | ::* Ovarian mucinous cystadenocarcinoma: 5-10% of mucinous tumor | ||
:* | :*'''Ovarian endometrioid tumour''': 8-15% of all ovarian tumor | ||
:* Clear cell ovarian carcinoma: ~5% of ovarian cancer | |||
:* Brenner tumour: ~2.5% of ovarian epithelial neoplasms | :* Brenner tumour: ~2.5% of ovarian epithelial neoplasms | ||
:* | :* Squamous cell carcinoma of the ovary | ||
:* | :* Ovarian cystadenofibroma / ovarian adenofibroma: can be serous, mucinous, endometrioid, clear cell or mixed | ||
:* | :* Ovarian cystadenocarcinofibroma: extremely rare | ||
:* | :* Undifferentiated carcinoma of the ovary: ~4% of all ovarian tumor | ||
{| {{table}} | {| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Vulvar Carcinomas Subtype'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Vulvar Carcinomas Subtype'''}} | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Histopathological Microscopic Analysis'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Histopathological Microscopic Analysis'''}} | ||
| Line 69: | Line 63: | ||
|- | |- | ||
|- | |- | ||
| | | Ovarian serous cystadenocarcinoma|| | ||
* | *[[Nuclear]] [[pleomorphism]]: | ||
* | :* Variation in size - often marked | ||
* | :* Variation in staining | ||
* | :* Variation in shape | ||
* | * +/-Macronucleolus - key feature | ||
* Eccentric nucleus | |||
* Architecture: | |||
:* Solid | |||
:* Papillary - classic | |||
*[[Glandular]] - uncommon | |||
* +/-Psammoma bodies - uncommon | |||
* +/-[[Necrosis]] - often extensive | |||
| | |||
|- | |- | ||
| | |Ovarian mucinous cystadenocarcinoma|| | ||
* | * Mucinous differentiation | ||
* | :* Tall columnar cells in glands with apical mucin | ||
* | :* May have an endocervical-like or intestinal-like appearance - see subtypes | ||
* | * Invasive morphology - one of the following: | ||
* | :* Back-to-back glands/confluent growth pattern | ||
* | :* Desmoplastic stromal response | ||
:* Cribriforming of glands | |||
* Malignant characteristics: | |||
:* +/-Nuclear atypia | |||
:* +/-Necrosis | |||
:* No cilia | |||
| | |||
|- | |- | ||
| | | Endometrioid carcinoma of the ovary|| | ||
* | * Tubular glands | ||
* | * Cribriform pattern common | ||
* | * May see mucinous secretion | ||
* | * May have squamous differentiation/squamous metaplasia | ||
* | * Resemblance to endometrial carcinoma, and over a third of cases have focal squamous differentiation | ||
|- | |- | ||
|} | |} | ||
===Clear cell tumor=== | |||
[[Clear cell tumor|Clear cell tumors]] can be either clear cell adenocarcinomas or clear cell sarcomas.On [[microscope|microscopic]] [[pathology|pathological]] examination, they are composed of cells with clear [[cytoplasm]] (that contains [[glycogen]]) and ''hob nail'' cells (from which the glycogen has been secreted).The pattern may be glandular, papillary or solid. | |||
Shown below is an image of Overian clear cell adenocarcinoma.(H&E stain,very high mag) | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
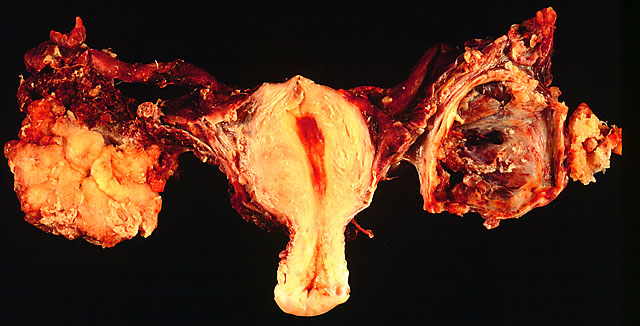
Image:ovserca.jpg|In this TAH-BSO specimen, the right ovary (on the left of the image) has been replaced by a solid serous carcinoma. The contralateral ovarian tumor is grossly cystic and could be termed a "cystadenocarcinoma." The patient had omental metastases and positive peritoneal fluid cytology. This cancer, which was discovered at exploratory laparotomy, apparently developed very rapidly; the patient had a normal pelvic ultrasound exam only 2 months before. (Courtesy of Ed Uthman, MD) | |||
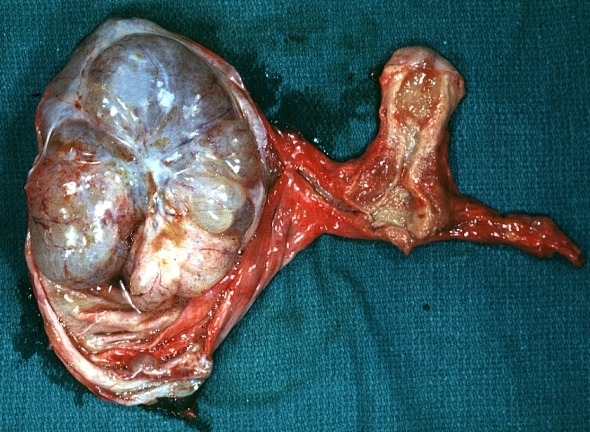
Image:Mucinous cystadenocarcinoma.jpg|Ovary: Mucinous cystadenocarcinoma: Gross, an excellent image of uterus is in picture and thus illustrates the very large size of the ovarian tumor. <br> <small> [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology</small>] | |||
</gallery> | |||
</div> | |||
==Video== | |||
Shown below is a video of clear cell adenocarcinoma of the vagina. | |||
{{#ev:youtube|qO2w8VLf690}} | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
| Line 109: | Line 130: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Gynecology]] | |||
[[Category:Surgery]] | |||
Latest revision as of 15:12, 6 September 2019
|
Ovarian cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ovarian cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Ovarian cancer pathophysiology |
|
Risk calculators and risk factors for Ovarian cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Huda A. Karman, M.D.
Overview
Ovarian cancer is usually diagnosed late resulting in a poor overall outcome for the patient. Pathological findings, therefore, often only occur in advanced symptomatic onset and tend to present more as severe pathologic outcomes.
Pathophysiology
Clear Cell Tumor
- Clear cell tumors are part of the surface epithelial-stromal tumor group of ovarian cancers, accounting for 6% of all neoplastic cases. Clear cell tumors are also associated with the pancreas and salivary glands.
- Benign and borderline variants of this neoplasm are rare, and most cases are malignant.
- Typically, they are cystic neoplasms with polypoid masses that protrude into the cyst.
Endometrioid Tumor
Endometrioid tumors are part of the surface epithelial tumor group of ovarian neoplasms (10-20% of which are the endometrioid type). Benign and borderline variants are rare, as the majority are malignant. There is an association with endometriosis and concurrent primary endometrial carcinoma (endometrial cancer).
Gross Patholgy
| Ovarian Carcinomas Subtype | Features on Gross Pathology |
| Ovarian serous cystadenocarcinoma |
|
| Ovarian mucinous cystadenocarcinoma |
|
| Endometrioid carcinoma of the ovary |
|
Microscopic Pathology
Histologic subtypes of epithelial ovarian tumor include:[1][2][3][4]
- Surface epithelial stromal ovarian tumor (60-70%)
- Ovarian serous tumor
- Ovarian serous cystadenoma: ~60% of serous tumor
- Ovarian borderline serous cystadenoma: ~15% of serous tumor
- Ovarian serous cystadenocarcinoma: ~25% of serous tumor. Commonest malignant ovarian tumor
- Ovarian mucinous tumor: ~20% of all ovarian tumor
- Ovarian mucinous cystadenoma: ~80% of mucinous tumor
- Ovarian bordeline mucinous cystadenoma: 10-15% of mucinous tumor
- Ovarian mucinous cystadenocarcinoma: 5-10% of mucinous tumor
- Ovarian endometrioid tumour: 8-15% of all ovarian tumor
- Clear cell ovarian carcinoma: ~5% of ovarian cancer
- Brenner tumour: ~2.5% of ovarian epithelial neoplasms
- Squamous cell carcinoma of the ovary
- Ovarian cystadenofibroma / ovarian adenofibroma: can be serous, mucinous, endometrioid, clear cell or mixed
- Ovarian cystadenocarcinofibroma: extremely rare
- Undifferentiated carcinoma of the ovary: ~4% of all ovarian tumor
| Vulvar Carcinomas Subtype | Features on Histopathological Microscopic Analysis | Image |
| Ovarian serous cystadenocarcinoma |
|
|
| Ovarian mucinous cystadenocarcinoma |
|
|
| Endometrioid carcinoma of the ovary |
|
Clear cell tumor
Clear cell tumors can be either clear cell adenocarcinomas or clear cell sarcomas.On microscopic pathological examination, they are composed of cells with clear cytoplasm (that contains glycogen) and hob nail cells (from which the glycogen has been secreted).The pattern may be glandular, papillary or solid.
Shown below is an image of Overian clear cell adenocarcinoma.(H&E stain,very high mag)
-
In this TAH-BSO specimen, the right ovary (on the left of the image) has been replaced by a solid serous carcinoma. The contralateral ovarian tumor is grossly cystic and could be termed a "cystadenocarcinoma." The patient had omental metastases and positive peritoneal fluid cytology. This cancer, which was discovered at exploratory laparotomy, apparently developed very rapidly; the patient had a normal pelvic ultrasound exam only 2 months before. (Courtesy of Ed Uthman, MD)
-
Ovary: Mucinous cystadenocarcinoma: Gross, an excellent image of uterus is in picture and thus illustrates the very large size of the ovarian tumor.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
Video
Shown below is a video of clear cell adenocarcinoma of the vagina.
{{#ev:youtube|qO2w8VLf690}}
References
- ↑ Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. ISBN 9780071716727.
- ↑ Malignant melanoma. Libre pathology. http://librepathology.org/wiki/index.php/Malignant_melanoma. URL Accessed on September 30, 2015
- ↑ Basal cell carcinoma . Libre pathology. http://librepathology.org/wiki/index.php/Basal_cell_carcinoma. URL Accessed on September 30, 2015
- ↑ Squamous cell carcinoma. Libre pathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma. URL Accessed on September 30, 2015