Osteosarcoma
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Osteosarcoma is the most common type of malignant bone cancer, accounting for 35% of primary bone malignancies. There is a preference for the metaphyseal region of tubular long bones. 50% of cases occur around the knee. It is a malignant connective (soft) tissue tumor whose neoplastic cells present osteoblastic differentiation and form tumoral bone.
Prevalence
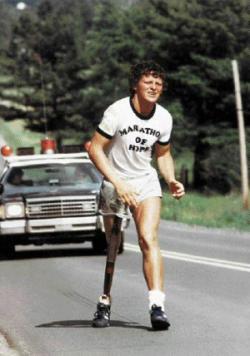
Osteosarcoma is the 6th leading cancer in children under age 15. Osteosarcoma affects 400 children under age 20 and 500 adults (most between the ages of 15-30) every year in the USA. Approximately 1/3 of the 900 will die each year, or about 300 a year. A second peak in incidence occurs in the elderly, usually associated with an underlying bone pathology such as Paget's disease, medullary infarct, or prior irradiation. Although about 90% of patients are able to have limb-salvage surgery, complications, such as infection, prosthetic loosening and non-union, or local tumor recurrence may cause the need for further surgery or amputation.
Pathology
The tumor may be localized at the end of the long bones. Most often it affects the upper end of tibia or humerus, or lower end of femur. The tumor is solid, hard, irregular ("fir-tree" or "sun-burst" appearance on X-ray examination) due to the tumor spicules of calcified bone radiating in right angles. These right angles form what is known as Codman's triangle. Surrounding tissues are infiltrated.
Microscopically: The characteric feature of osteosarcoma is presence of osteoid (bone formation) within the tumour. Tumor cells are very pleomorphic (anaplastic), some are giant, numerous atypical mitoses. These cells produce osteoid describing irregular trabeculae (amorphous, eosinophilic/pink) with or without central calcification (hematoxylinophilic/blue, granular) - tumor bone. Tumor cells are included in the osteoid matrix. Depending on the features of the tumour cells present (whether they resemble bone cells, cartilage cells or fibroblast cells), the tumour can be subclassified. Presence of immature blood vessels (sarcomatous vessels lacking endothelial cells) favors the bloodstream metastasizing.
Causes
The causes of osteosarcoma are not known. Questions remain about whether radium, or fluoride, in drinking water can act as "environmental triggers" for increasing the incidence of the disease. A low selenium or Vitamin D3 level or a high level of inflammation, as measured by interleukin-6, interleukin-8, or Nf-kB, Tumor Necrosis Factor Alpha may have a significant role as tumor suppressors and tumor initiators respectively. Recent studies show that an increased level of c-Fos can lead to osteosarcoma. The study that showed this result was done on transgenic mice in which the Fluid Sheer Stress (FSS) was increased to increase the number of osteoblast. Since c-Fos is ubiquitous in its overexpression it can not only increase the osteoblast resulting in the symptoms osteosarcoma. Therefore it is recently believed that a biological effect that may cause osteosarcoma is an error in the molecular pathway that controls c-Fos, causing an overexpression with no other counter stimuli to stop over production
Symptoms
Many patients first complain of pain that may be worse at night, and may have been occurring for some time. If the tumour is large, it can appear as a swelling. The affected bone is not as strong as normal bones and may fracture with minor trauma (a pathological fracture).
Genetics
Hereditary syndromes of osteosarcoma have been identified[1]:
- Rothmund-Thomson Syndrome
- RECQL4 gene mutations
- RB1 gene mutations (also implicated in retinoblastoma)
- Li-Fraumeni syndrome
These syndromes are extremely rare within the Osteosarcoma diagnosis, and probably represent less than 0.5% of those diagnosed
Diagnosis
Family physicians and orthopedists rarely see a malignant bone tumor (most bone tumors are benign). Thus, many patients are initially misdiagnosed with cysts or muscle problems, and some are sent straight to physical therapy without an x-ray.
The route to osteosarcoma diagnosis usually begins with an x-ray, continues with a combination of scans (CT scan, PET scan, bone scan, MRI) and ends with a surgical biopsy. Much can be seen on films, but the biopsy is the only definitive proof that a bone tumor is indeed malignant or benign.
The biopsy of suspected osteosarcoma should be performed by a qualified orthopedic oncologist. The American Cancer Society states: "Probably in no other cancer is it as important to perform this procedure properly. An improperly performed biopsy may make it difficult to save the affected limb from amputation."
MRI
Treatment
Patients with osteosarcoma are best managed by a medical oncologist and an orthopedic oncologist experienced in managing sarcomas. Current standard treatment is to use neoadjuvant chemotherapy (chemotherapy given before surgery) followed by surgical resection. The percentage of tumor cell necrosis (cell death) seen in the tumor after surgery gives an idea of the prognosis and also lets the oncologist know if the chemotherapy regime should be altered after surgery.
Standard therapy is a combination of limb-salvage orthopedic surgery and a combination of high dose methotrexate with leucovorin rescue, intra-arterial cisplatin caffeine, adriamycin, ifosfamide with mesna, BCD, etoposide, muramyl tri-peptite (MTP).
Ifosfamide can be used as an adjuvant treatment if the necrosis rate is low.
3-year event free survival ranges from 50% to 75%. and 5-year survival ranges from 60% to 85+% in some studies. Overall, 60-65% treated 5-years ago (2000) will be alive today. Osteosarcoma has one of the lowest survival rates for pediatric cancer despite chemotherapy's success in osteosarcoma of 6 chemotherapies, interferon-alpha, interleukin-2, and being the prototype of solid tumors in cancer.
Treatment studies come from Children's hospital Boston, Memorial Sloan-Kettering, Children's Oncology Group, Italian Oncology Group, Japan, and MD Anderson in Texas.
Fluids are given for hydration.
Drugs like Kytril and Zofran help with nausea and vomiting.
Neupogen, epogen, Neulasta help with white blood cell counts and neutrophil counts.
Blood helps with anemia.
Prognosis
- Prognosis is separated into three groups.
- Stage I osteosarcoma is rare and includes parosteal osteosarcoma or low-grade central osteosarcoma. It has an excellent prognosis (>90%) with wide resection.
- Stage IIb prognosis depends on the site of the tumor (proximal tibia, femur, pelvis, etc.) size of the tumor mass (in cm.), the degree of necrosis from neoadjuvant chemotherapy (beforeoperation chemotherapy), and pathological factors like the degree of p-glycoprotein, whether your tumor is cxcr4-positive.[2] Her2-positive as these can lead to distant metastases to the lung. Longer time to metastases, more than 12 months or 24 months and the number of metastases and resectability of them lead to the best prognosis with metastatic osteosarcoma. It is better to have fewer metastases than longer time to metastases. Those with a longer length of time(>24months) and few nodules (2 or fewer) have the best prognosis with a 2-year survival after the metastases of 50% 5-year of 40% and 10 year 20%. If metastases are both local and regional the prognosis is different unfortunately.
- Initial Presentation of stage III osteosarcoma with lung metastates depends on the resectability of the primary tumor and lung nodules, degree of necrosis of the primary tumor, and maybe the number of metastases. Overall prognosis is 30% or greater depending.
References
- ↑ Wang LL. Biology of osteogenic sarcoma. Cancer J 11:294-305, 2005.
- ↑ http://www.osteosarcomasupport.org/cxcr4_metastases.pdf
External links
- Superior Survivial Seen with Osteosarcoma 2004
- Osteosarcoma: A Multidisciplinary Approach to Diagnosis and Treatment
- http://www.emedicine.com/PED/topic1684.htm
- http://www.mayoclinic.org/osteosarcoma/index.html
- Support Group and Information for people with osteosarcoma
- Treatment Information from U.S. National Cancer Institute
- Osteosarcoma by Peter Buecker, MD and Mark Gebhardt, MD
- Green Drakkoman Foundation to assist Warriors of Rare Childhood Cancers
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson M.S., M.D. Template:SIB de:Osteosarkom it:Osteosarcoma nl:Osteosarcoom