Multiple sclerosis physical examination: Difference between revisions
m (Categories) |
No edit summary |
||
| Line 7: | Line 7: | ||
==Physical Examination== | ==Physical Examination== | ||
Physical examination of patients with multiple sclerosis is usually remarkable for: | |||
==== Lhermitte's Sign ==== | |||
About 25-40% of MS patients experience lhermitte’s sign as an electrical shock sensation going downward from neck when the patients neck bends forward. Lhermitte sign can correlate with MRI abnormalities of caudal medulla or cervical dorsal columns. .<ref>{{cite journal |author=Gutrecht JA, Zamani AA, Slagado ED|title=Anatomic-radiologic basis of Lhermitte's sign in multiple sclerosis |journal=Arch. Neurol. |volume=50 |issue=8 |pages=849-51|year=1993 |pmid=8352672 |doi=}}</ref><ref>{{cite journal |author=Al-Araji AH, Oger J |title=Reappraisal of Lhermitte's sign in multiple sclerosis |journal=Mult. Scler.|volume=11 |issue=4 |pages=398-402 |year=2005 |pmid=16042221 |doi=}}</ref><ref>{{cite journal |author=Sandyk R, Dann LC|title=Resolution of Lhermitte's sign in multiple sclerosis by treatment with weak electromagnetic fields |journal=Int. J. Neurosci.|volume=81 |issue=3-4 |pages=215-24 |year=1995 |pmid=7628912 |doi=}}</ref><ref>{{cite journal |author=Kanchandani R, Howe JG|title=Lhermitte's sign in multiple sclerosis: a clinical survey and review of the literature |journal=J. Neurol. Neurosurg. Psychiatr. |volume=45 |issue=4 |pages=308-12 |year=1982 |pmid=7077340 |doi=}}</ref> | |||
==== Internuclear Ophthalmoplegia ==== | |||
=== Internuclear Ophthalmoplegia === | |||
[[Image:Internuclear ophthalmoplegia.jpg|thumb|right|180px|''Schematic demonstrating right internuclear ophthalmoplegia, caused by injury of the right [[medial longitudinal fasciculus]] ]] | [[Image:Internuclear ophthalmoplegia.jpg|thumb|right|180px|''Schematic demonstrating right internuclear ophthalmoplegia, caused by injury of the right [[medial longitudinal fasciculus]] '']] | ||
{{Main|Internuclear ophthalmoplegia}} | {{Main|Internuclear ophthalmoplegia}} | ||
| Line 28: | Line 24: | ||
Up to 50% of patients with MS will develop an episode of optic neuritis, and 20% of the time optic neuritis is the presenting sign of MS. The presence of demyelinating white matter lesions on brain [[MRI]] at the time of presentation of optic neuritis is the strongest predictor for developing clinically definite MS. Almost half of the patients with optic neuritis have white matter lesions consistent with multiple sclerosis. | Up to 50% of patients with MS will develop an episode of optic neuritis, and 20% of the time optic neuritis is the presenting sign of MS. The presence of demyelinating white matter lesions on brain [[MRI]] at the time of presentation of optic neuritis is the strongest predictor for developing clinically definite MS. Almost half of the patients with optic neuritis have white matter lesions consistent with multiple sclerosis. | ||
At five years follow-up, the overall risk of developing MS is 30%, with or without MRI lesions. Patients with a normal MRI still develop MS (16%), but at a lower rate compared to those patients with three or more MRI lesions (51%). From the other perspective, however, almost half (44%) of patients with any demyelinating lesions on MRI at presentation will not have developed MS ten years later. <ref>{{cite journal |author=Beck RW, Trobe JD |title=What we have learned from the Optic Neuritis Treatment Trial|journal=Ophthalmology |volume=102 |issue=10 |pages=1504-8 |year=1995 |pmid=9097798}}</ref><ref>{{cite journal |author= |title=The 5-year risk of MS after optic neuritis: experience of the optic neuritis treatment trial. 1997 |journal=Neurology |volume=57|issue=12 Suppl 5 |pages=S36-45 |year=2001 |pmid=11902594}}</ref> | At five years follow-up, the overall risk of developing MS is 30%, with or without MRI lesions. Patients with a normal MRI still develop MS (16%), but at a lower rate compared to those patients with three or more MRI lesions (51%). From the other perspective, however, almost half (44%) of patients with any demyelinating lesions on MRI at presentation will not have developed MS ten years later. <ref>{{cite journal |author=Beck RW, Trobe JD |title=What we have learned from the Optic Neuritis Treatment Trial|journal=Ophthalmology |volume=102 |issue=10 |pages=1504-8 |year=1995 |pmid=9097798}}</ref><ref>{{cite journal |author= |title=The 5-year risk of MS after optic neuritis: experience of the optic neuritis treatment trial. 1997 |journal=Neurology |volume=57|issue=12 Suppl 5 |pages=S36-45 |year=2001 |pmid=11902594}}</ref> | ||
==References== | ==References== | ||
Revision as of 08:58, 1 March 2018
|
Multiple sclerosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Multiple sclerosis physical examination On the Web |
|
American Roentgen Ray Society Images of Multiple sclerosis physical examination |
|
Risk calculators and risk factors for Multiple sclerosis physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Physical Examination
Physical examination of patients with multiple sclerosis is usually remarkable for:
Lhermitte's Sign
About 25-40% of MS patients experience lhermitte’s sign as an electrical shock sensation going downward from neck when the patients neck bends forward. Lhermitte sign can correlate with MRI abnormalities of caudal medulla or cervical dorsal columns. .[1][2][3][4]
Internuclear Ophthalmoplegia
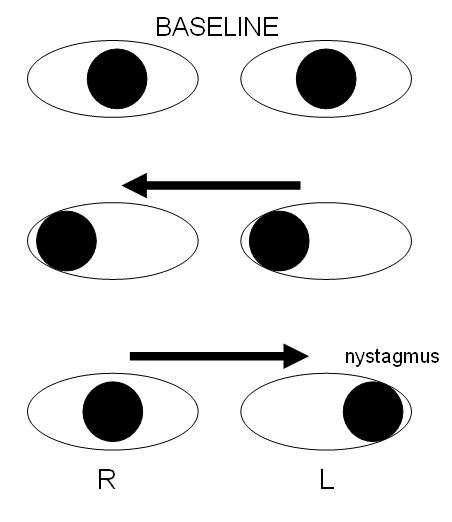
Internuclear ophthalmoplegia is a disorder of conjugate lateral gaze. The affected eye shows impairment of adduction. The partner eye diverges from the affected eye during abduction, producing diplopia; during extreme abduction, compensatory nystagmus can be seen in the partner eye. Diplopia means double vision while nystagmus is involuntary eye movement characterized by alternating smooth pursuit in one direction and a saccadic movement in the other direction.
Internuclear ophthalmoplegia occurs when MS affects a part of the brain stem called the medial longitudinal fasciculus, which is responsible for communication between the two eyes by connecting the abducens nucleus of one side to the oculomotor nucleus of the opposite side. This results in the failure of the medial rectus muscle to contract appropriately, so that the eyes do not move equally (called disconjugate gaze).
Optic Neuritis
Up to 50% of patients with MS will develop an episode of optic neuritis, and 20% of the time optic neuritis is the presenting sign of MS. The presence of demyelinating white matter lesions on brain MRI at the time of presentation of optic neuritis is the strongest predictor for developing clinically definite MS. Almost half of the patients with optic neuritis have white matter lesions consistent with multiple sclerosis. At five years follow-up, the overall risk of developing MS is 30%, with or without MRI lesions. Patients with a normal MRI still develop MS (16%), but at a lower rate compared to those patients with three or more MRI lesions (51%). From the other perspective, however, almost half (44%) of patients with any demyelinating lesions on MRI at presentation will not have developed MS ten years later. [5][6]
References
- ↑ Gutrecht JA, Zamani AA, Slagado ED (1993). "Anatomic-radiologic basis of Lhermitte's sign in multiple sclerosis". Arch. Neurol. 50 (8): 849–51. PMID 8352672.
- ↑ Al-Araji AH, Oger J (2005). "Reappraisal of Lhermitte's sign in multiple sclerosis". Mult. Scler. 11 (4): 398–402. PMID 16042221.
- ↑ Sandyk R, Dann LC (1995). "Resolution of Lhermitte's sign in multiple sclerosis by treatment with weak electromagnetic fields". Int. J. Neurosci. 81 (3–4): 215–24. PMID 7628912.
- ↑ Kanchandani R, Howe JG (1982). "Lhermitte's sign in multiple sclerosis: a clinical survey and review of the literature". J. Neurol. Neurosurg. Psychiatr. 45 (4): 308–12. PMID 7077340.
- ↑ Beck RW, Trobe JD (1995). "What we have learned from the Optic Neuritis Treatment Trial". Ophthalmology. 102 (10): 1504–8. PMID 9097798.
- ↑ "The 5-year risk of MS after optic neuritis: experience of the optic neuritis treatment trial. 1997". Neurology. 57 (12 Suppl 5): S36–45. 2001. PMID 11902594.