Multiple sclerosis causes: Difference between revisions
(Created page with "__NOTOC__ {{Template:Multiple sclerosis}} {{CMG}} ==Overview== == Causes == Although many risk factors for multiple sclerosis have been identified, no definitive cause has b...") |
|||
| Line 15: | Line 15: | ||
=== Environmental === | === Environmental === | ||
The most popular hypothesis is that a [[virus|viral]] infection or [[retrovirus|retroviral]] reactivation primes a susceptible immune system for an abnormal reaction later in life. On a [[molecule|molecular]] level, this might occur if there is a structural similarity between the infectious virus and some component of the central nervous system, leading to eventual confusion in the[[immune system]]. | The most popular hypothesis is that a [[virus|viral]] infection or [[retrovirus|retroviral]] reactivation primes a susceptible immune system for an abnormal reaction later in life. On a [[molecule|molecular]] level, this might occur if there is a structural similarity between the infectious virus and some component of the central nervous system, leading to eventual confusion in the [[immune system]]. | ||
Since MS seems to be more common in people who live farther from the equator, another theory proposes that decreased sunlight exposure<ref>{{cite journal |author=van der Mei IA, Ponsonby AL, Dwyer T, ''et al'' |title=Past exposure to sun, skin phenotype, and risk of multiple sclerosis: case-control study |journal=BMJ |volume=327 |issue=7410 |pages=316 |year=2003 |pmid=12907484|doi=10.1136/bmj.327.7410.316}}</ref> and possibly decreased [[vitamin D]] production may help cause MS. This theory is bolstered by recent research into the [[biochemistry]] of vitamin D, which has shown that it is an important immune system regulator. A large, 2006 study by the Harvard School of Public Health, reported evidence of a link between Vitamin D deficiency and the onset of multiple sclerosis.<ref>{{cite journal |author=Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A |title=Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis |journal=JAMA |volume=296 |issue=23 |pages=2832-8 |year=2006 |pmid=17179460|doi=10.1001/jama.296.23.2832}}</ref> Other data comes from a 2007 study which concluded that sun exposure during childhood reduces the risk of suffering MS, while controlling for genetic factors.<ref>[http://www.neurology.org/cgi/content/abstract/69/4/381?etocChildhood sun exposure influences risk of multiple sclerosis in monozygotic twins.] Talat Islam, MBBS, PhD, W. James Gauderman, PhD, Wendy Cozen, DO, MPH and Thomas M. Mack, MD, MPH. ''Neurology'' 2007;69:381-388</ref><ref>[http://news.bbc.co.uk/1/hi/health/6906712.stm Sunshine 'protective' against MS]. BBC News, 28 July 2007, 23:40 </ref> | Since MS seems to be more common in people who live farther from the equator, another theory proposes that decreased sunlight exposure<ref>{{cite journal |author=van der Mei IA, Ponsonby AL, Dwyer T, ''et al'' |title=Past exposure to sun, skin phenotype, and risk of multiple sclerosis: case-control study |journal=BMJ |volume=327 |issue=7410 |pages=316 |year=2003 |pmid=12907484|doi=10.1136/bmj.327.7410.316}}</ref> and possibly decreased [[vitamin D]] production may help cause MS. This theory is bolstered by recent research into the [[biochemistry]] of vitamin D, which has shown that it is an important immune system regulator. A large, 2006 study by the Harvard School of Public Health, reported evidence of a link between Vitamin D deficiency and the onset of multiple sclerosis.<ref>{{cite journal |author=Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A |title=Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis |journal=JAMA |volume=296 |issue=23 |pages=2832-8 |year=2006 |pmid=17179460|doi=10.1001/jama.296.23.2832}}</ref> Other data comes from a 2007 study which concluded that sun exposure during childhood reduces the risk of suffering MS, while controlling for genetic factors.<ref>[http://www.neurology.org/cgi/content/abstract/69/4/381?etocChildhood sun exposure influences risk of multiple sclerosis in monozygotic twins.] Talat Islam, MBBS, PhD, W. James Gauderman, PhD, Wendy Cozen, DO, MPH and Thomas M. Mack, MD, MPH. ''Neurology'' 2007;69:381-388</ref><ref>[http://news.bbc.co.uk/1/hi/health/6906712.stm Sunshine 'protective' against MS]. BBC News, 28 July 2007, 23:40 </ref> | ||
| Line 21: | Line 21: | ||
Other theories, noting that MS is less common in children with siblings, suggest that less exposure to illness in childhood leads to an immune system which is not primed to fight infection and is thus more likely to attack the body. One explanation for this would be an imbalance between the Th1 type of [[T helper cell|helper T-cells]], which fight infection, and the Th2 type, which are more active in [[allergy]] and more likely to attack the body. | Other theories, noting that MS is less common in children with siblings, suggest that less exposure to illness in childhood leads to an immune system which is not primed to fight infection and is thus more likely to attack the body. One explanation for this would be an imbalance between the Th1 type of [[T helper cell|helper T-cells]], which fight infection, and the Th2 type, which are more active in [[allergy]] and more likely to attack the body. | ||
Other theories describe MS as an immune response to a chronic infection. The association of MS with the [[Epstein-Barr virus]]suggests a potential viral contribution in at least some individuals.<ref>{{cite journal |author=Levin LI, Munger KL, Rubertone MV,''et al'' |title=Temporal relationship between elevation of epstein-barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis |journal=JAMA |volume=293 |issue=20 |pages=2496-500 |year=2005 |pmid=15914750|doi=10.1001/jama.293.20.2496}}</ref> Still others believe that MS may sometimes result from a chronic infection with[[spirochetal]] bacteria, a hypothesis supported by research in which cystic forms were isolated from the cerebrospinal fluid of all MS patients in a small study.<ref>{{cite journal |author=Brorson O, Brorson SH, Henriksen TH, Skogen PR, Schøyen R|title=Association between multiple sclerosis and cystic structures in cerebrospinal fluid |journal=Infection |volume=29 |issue=6|pages=315-9 |year=2001 |pmid=11787831 |doi=}}</ref> When the cysts were cultured, propagating spirochetes emerged. Another bacterium that has been implicated in MS is ''[[Chlamydophila pneumoniae]]''; it or its DNA has been found in the cerebrospinal fluid of MS patients by several research laboratories, with one study finding that the [[oligoclonal bands]] of 14 of the 17 MS patients studied consisted largely of antibodies to Chlamydophila antigens.<ref>{{cite journal |author=Yao SY, Stratton CW, Mitchell WM, Sriram S |title=CSF oligoclonal bands in MS include antibodies against Chlamydophila antigens |journal=Neurology |volume=56|issue=9 |pages=1168-76 |year=2001 |pmid=11342681 |doi=}}</ref> | Other theories describe MS as an immune response to a chronic infection. The association of MS with the [[Epstein-Barr virus]]suggests a potential viral contribution in at least some individuals.<ref>{{cite journal |author=Levin LI, Munger KL, Rubertone MV,''et al'' |title=Temporal relationship between elevation of epstein-barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis |journal=JAMA |volume=293 |issue=20 |pages=2496-500 |year=2005 |pmid=15914750|doi=10.1001/jama.293.20.2496}}</ref> Still others believe that MS may sometimes result from a chronic infection with [[spirochetal]] bacteria, a hypothesis supported by research in which cystic forms were isolated from the cerebrospinal fluid of all MS patients in a small study.<ref>{{cite journal |author=Brorson O, Brorson SH, Henriksen TH, Skogen PR, Schøyen R|title=Association between multiple sclerosis and cystic structures in cerebrospinal fluid |journal=Infection |volume=29 |issue=6|pages=315-9 |year=2001 |pmid=11787831 |doi=}}</ref> When the cysts were cultured, propagating spirochetes emerged. Another bacterium that has been implicated in MS is ''[[Chlamydophila pneumoniae]]''; it or its DNA has been found in the cerebrospinal fluid of MS patients by several research laboratories, with one study finding that the [[oligoclonal bands]] of 14 of the 17 MS patients studied consisted largely of antibodies to Chlamydophila antigens.<ref>{{cite journal |author=Yao SY, Stratton CW, Mitchell WM, Sriram S |title=CSF oligoclonal bands in MS include antibodies against Chlamydophila antigens |journal=Neurology |volume=56|issue=9 |pages=1168-76 |year=2001 |pmid=11342681 |doi=}}</ref> | ||
Severe stress may also be a factor—a large study in Denmark found that parents who had lost a child unexpectedly were 50% more likely to develop MS than parents who had not.<ref>{{cite journal | author = Li J, Johansen C, Bronnum-Hansen H, Stenager E, Koch-Henriksen N, Olsen J | title = The risk of multiple sclerosis in bereaved parents: A nationwide cohort study in Denmark. |journal = Neurology | volume = 62 | issue = 5 | pages = 726-9 | year = 2004 | pmid = 15007121}}</ref> [[Tobacco smoking|Smoking]]has also been shown to be an independent risk factor for developing MS.<ref>{{cite journal |author=Franklin GM, Nelson L|title=Environmental risk factors in multiple sclerosis: causes, triggers, and patient autonomy |journal=Neurology |volume=61|issue=8 |pages=1032-4 |year=2003 |pmid=14581658 |doi=}}</ref> | Severe stress may also be a factor—a large study in Denmark found that parents who had lost a child unexpectedly were 50% more likely to develop MS than parents who had not.<ref>{{cite journal | author = Li J, Johansen C, Bronnum-Hansen H, Stenager E, Koch-Henriksen N, Olsen J | title = The risk of multiple sclerosis in bereaved parents: A nationwide cohort study in Denmark. |journal = Neurology | volume = 62 | issue = 5 | pages = 726-9 | year = 2004 | pmid = 15007121}}</ref> [[Tobacco smoking|Smoking]]has also been shown to be an independent risk factor for developing MS.<ref>{{cite journal |author=Franklin GM, Nelson L|title=Environmental risk factors in multiple sclerosis: causes, triggers, and patient autonomy |journal=Neurology |volume=61|issue=8 |pages=1032-4 |year=2003 |pmid=14581658 |doi=}}</ref> | ||
Revision as of 13:56, 27 August 2012
|
Multiple sclerosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Multiple sclerosis causes On the Web |
|
American Roentgen Ray Society Images of Multiple sclerosis causes |
|
Risk calculators and risk factors for Multiple sclerosis causes |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Causes
Although many risk factors for multiple sclerosis have been identified, no definitive cause has been found. MS likely occurs as a result of some combination of both environmental and genetic factors. Various theories try to combine the known data into plausible explanations. Although most accept an autoimmune explanation, several theories suggest that MS is an appropriate immune response to one or several underlying conditions (the etiology could be heterogeneous[1]). The need for alternative theories is supported by the poor results of present therapies, since autoimmune theory predicted greater success.[2][3][4]
Environmental
The most popular hypothesis is that a viral infection or retroviral reactivation primes a susceptible immune system for an abnormal reaction later in life. On a molecular level, this might occur if there is a structural similarity between the infectious virus and some component of the central nervous system, leading to eventual confusion in the immune system.
Since MS seems to be more common in people who live farther from the equator, another theory proposes that decreased sunlight exposure[5] and possibly decreased vitamin D production may help cause MS. This theory is bolstered by recent research into the biochemistry of vitamin D, which has shown that it is an important immune system regulator. A large, 2006 study by the Harvard School of Public Health, reported evidence of a link between Vitamin D deficiency and the onset of multiple sclerosis.[6] Other data comes from a 2007 study which concluded that sun exposure during childhood reduces the risk of suffering MS, while controlling for genetic factors.[7][8]
Other theories, noting that MS is less common in children with siblings, suggest that less exposure to illness in childhood leads to an immune system which is not primed to fight infection and is thus more likely to attack the body. One explanation for this would be an imbalance between the Th1 type of helper T-cells, which fight infection, and the Th2 type, which are more active in allergy and more likely to attack the body.
Other theories describe MS as an immune response to a chronic infection. The association of MS with the Epstein-Barr virussuggests a potential viral contribution in at least some individuals.[9] Still others believe that MS may sometimes result from a chronic infection with spirochetal bacteria, a hypothesis supported by research in which cystic forms were isolated from the cerebrospinal fluid of all MS patients in a small study.[10] When the cysts were cultured, propagating spirochetes emerged. Another bacterium that has been implicated in MS is Chlamydophila pneumoniae; it or its DNA has been found in the cerebrospinal fluid of MS patients by several research laboratories, with one study finding that the oligoclonal bands of 14 of the 17 MS patients studied consisted largely of antibodies to Chlamydophila antigens.[11]
Severe stress may also be a factor—a large study in Denmark found that parents who had lost a child unexpectedly were 50% more likely to develop MS than parents who had not.[12] Smokinghas also been shown to be an independent risk factor for developing MS.[13]
Genetic
MS is not considered a hereditary disease. However, increasing scientific evidence suggests that genetics may play a role in determining a person's susceptibility to MS:
Some populations, such as the Roma, Inuit, and Bantus, rarely if ever get MS. The indigenous peoples of the Americas and Asians have very low incidence rates.
In the population at large, the chance of developing MS is less than a tenth of one percent. However, if one person in a family has MS, that person's first-degree relatives—parents, children, and siblings—have a one to three percent chance of getting the disease.
For identical twins, the likelihood that the second twin may develop MS if the first twin does is about 30%. For fraternal twins (who do not inherit an identical set of genes), the likelihood is closer to that for non-twin siblings, or about 4%. This pattern suggests that, while genetic factors clearly help determine the risk of MS, other factors such as environmental effects or random chance are also involved. The actual correlation may be somewhat higher than reported by these numbers as people with MS lesions remain essentially asymptomatic throughout their lives.
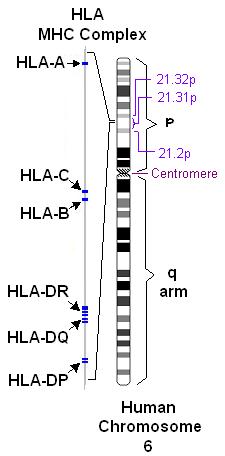
Further indications that more than one gene is involved in MS susceptibility comes from studies of families in which more than one member has MS. Several research teams found that people with MS inherit certain regions on individual genes more frequently than people without MS. Of particular interest is the human leukocyte antigen (HLA) or major histocompatibility complex region on chromosome 6. HLAs are genetically determined proteins that influence the immune system. However, there are other genes in this region which are not related to the immune system.
The HLA patterns of MS patients tend to be different from those of people without the disease. Investigations in northern Europe and America have detected three HLAs that are more prevalent in people with MS than in the general population. Studies of American MS patients have shown that people with MS also tend to exhibit these HLAs in combination—that is, they have more than one of the three HLAs—more frequently than the rest of the population. Furthermore, there is evidence that different combinations of the HLAs may correspond to variations in disease severity and progression.
A large study examining 334,923 single nucleotide polymorphisms (small variations in genes) in 931 families showed that apart from HLA-DRA there were two genes in which polymorphisms strongly predicted MS; these were the IL2RA (a subunit of the receptor for interleukin 2) and the IL7RA (idem forinterleukin 7) genes. Mutations in these genes were already known to be associated with diabetes mellitus type 1 and other autoimmune conditions; the findings circumstantially support the notion that MS is an autoimmune disease.[14]
Studies of families with multiple cases of MS and research comparing proteins expressed in humans with MS to those of mice with EAE suggest that another area related to MS susceptibility may be located on chromosome 5. Other regions on chromosomes 2, 3, 7, 11, 17, 19, and X have also been identified as possibly containing genes involved in the development of MS.
These studies strengthen the theory that MS is the result of a number of factors rather than a single gene or other agent. Development of MS is likely to be influenced by the interactions of a number of genes, each of which (individually) has only a modest effect. Additional studies are needed to specifically pinpoint which genes are involved, determine their function, and learn how each gene's interactions with other genes and with the environment make an individual susceptible to MS.
References
- ↑ Lassmann H (2007). "Experimental models of multiple sclerosis". Rev. Neurol. (Paris). 163 (6–7): 651–5. PMID 17607184.
- ↑ Peter Behan and Abhijit Chaudhuri (2002). "The pathogenesis of multiple sclerosis revisited" (PDF). J R Coll Physicians Edinb. 32: 244–265.
- ↑ Chaudhuri A, Behan P (2004). "Multiple sclerosis is not an autoimmune disease". Arch. Neurol. 61 (10): 1610–2. PMID 15477520.
- ↑ Altmann D (2005). "Evaluating the evidence for multiple sclerosis as an autoimmune disease". Arch. Neurol. 62 (4): 688, author reply 688-9. PMID 15824275.
- ↑ van der Mei IA, Ponsonby AL, Dwyer T; et al. (2003). "Past exposure to sun, skin phenotype, and risk of multiple sclerosis: case-control study". BMJ. 327 (7410): 316. doi:10.1136/bmj.327.7410.316. PMID 12907484.
- ↑ Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A (2006). "Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis". JAMA. 296 (23): 2832–8. doi:10.1001/jama.296.23.2832. PMID 17179460.
- ↑ sun exposure influences risk of multiple sclerosis in monozygotic twins. Talat Islam, MBBS, PhD, W. James Gauderman, PhD, Wendy Cozen, DO, MPH and Thomas M. Mack, MD, MPH. Neurology 2007;69:381-388
- ↑ Sunshine 'protective' against MS. BBC News, 28 July 2007, 23:40
- ↑ Levin LI, Munger KL, Rubertone MV; et al. (2005). "Temporal relationship between elevation of epstein-barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis". JAMA. 293 (20): 2496–500. doi:10.1001/jama.293.20.2496. PMID 15914750.
- ↑ Brorson O, Brorson SH, Henriksen TH, Skogen PR, Schøyen R (2001). "Association between multiple sclerosis and cystic structures in cerebrospinal fluid". Infection. 29 (6): 315–9. PMID 11787831.
- ↑ Yao SY, Stratton CW, Mitchell WM, Sriram S (2001). "CSF oligoclonal bands in MS include antibodies against Chlamydophila antigens". Neurology. 56 (9): 1168–76. PMID 11342681.
- ↑ Li J, Johansen C, Bronnum-Hansen H, Stenager E, Koch-Henriksen N, Olsen J (2004). "The risk of multiple sclerosis in bereaved parents: A nationwide cohort study in Denmark". Neurology. 62 (5): 726–9. PMID 15007121.
- ↑ Franklin GM, Nelson L (2003). "Environmental risk factors in multiple sclerosis: causes, triggers, and patient autonomy". Neurology. 61 (8): 1032–4. PMID 14581658.
- ↑ "Risk Alleles for Multiple Sclerosis Identified by a Genomewide Study". N Engl J Med. 2007. doi:10.1056/NEJMoa073493. PMID 17660530.