Mitral regurgitation surgery: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Mitral regurgitation surgery}} | {{Mitral regurgitation surgery}} | ||
'''For the WikiPatient page for this topic, click [[Mitral valve surgery (patient information)|here]]''' | '''For the WikiPatient page for this topic, click [[Mitral valve surgery (patient information)|here]]''' | ||
'''For the main page of mitral regurgitation, click [[Mitral regurgitation|here]]''' | |||
{{CMG}}; '''Associate Editor(s)-In-Chief:''' [[User:Mohammed Sbeih|Mohammed A. Sbeih, M.D.]] [mailto:msbeih@perfuse.org]; {{CZ}}; [[Varun Kumar]], M.B.B.S.; [[Lakshmi Gopalakrishnan]], M.B.B.S. | {{CMG}}; '''Associate Editor(s)-In-Chief:''' [[User:Mohammed Sbeih|Mohammed A. Sbeih, M.D.]] [mailto:msbeih@perfuse.org]; {{CZ}}; [[Varun Kumar]], M.B.B.S.; [[Lakshmi Gopalakrishnan]], M.B.B.S. | ||
Revision as of 13:57, 23 September 2011
|
Mitral regurgitation surgery | |
|
Treatment | |
|---|---|
|
Mitral regurgitation surgery On the Web | |
|
American Roentgen Ray Society Images of Mitral regurgitation surgery | |
|
Directions to Hospitals Performing Mitral regurgitation surgery | |
|
Risk calculators and risk factors for Mitral regurgitation surgery | |
For the WikiPatient page for this topic, click here
For the main page of mitral regurgitation, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Mohammed A. Sbeih, M.D. [2]; Cafer Zorkun, M.D., Ph.D. [3]; Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.
Overview
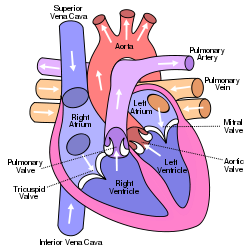
Mitral valve surgery is a surgery that can either repair or replace the mitral valve in the heart. It then closes, keeping blood from flowing backwards. Mitral valve surgery is indicated when the mitral regurgitation is severe or when the patient is symptomatic. Decision between valve repair or valve replacement is made based on the type and severity of damage to mitral valve.
In open surgery, the surgeon makes a large cut in the sternum to reach the heart. Minimally invasive mitral valve surgery is done through much smaller surgical cuts than the large cuts needed for open surgery.
Treatments for Mitral valve regurgitation
The choice of treatment depends on the symptoms present and the condition and function of the heart. Patients with high blood pressure or a weakened heart muscle may be given medications to reduce the strain on the heart and help improve the condition.
Anticoagulant or antiplatelet medications (blood thinners) may be used to prevent clots from forming in patients with atrial fibrillation.
Digitalis may be used to strengthen the heartbeat, along with diuretics (water pills) to remove excess fluid in the lungs.
A low-sodium diet may be helpful. Most people have no symptoms; but if a person develops symptoms, activity may be restricted.
Hospitalization may be required for diagnosis and treatment of severe symptoms. Surgical repair or replacement of the valve is recommended if heart function is poor, symptoms are severe, or the condition gets worse. Once the diagnosis of mitral regurgitation is made, the patient should have regular follow-ups with a specialist to determine whether he or she need surgery.
In the past, patients with heart valve problems such as mitral regurgitation were given antibiotics before dental work or an invasive procedure, such as colonoscopy. The antibiotics were given to prevent an infection of the damaged heart valve. However, antibiotics are now used much less often before dental work and other procedures.
Indications for Mitral valve regurgitation surgery
Surgery is indicated in patients with symptomatic mitral valve regurgitation, also it is indicated in patients with abnormalities in LV size or function (These include a left ventricular ejection fraction (LVEF) of less than 60% and a left ventricular end systolic dimension (LVESD) of greater than 45 mm), pulmonary hypertension, or new onset atrial fibrillation even without symptoms [1]. The patient with severe LV dysfunction (an LVEF < 30% and/or a left ventricular end-systolic dimension greater than 55 mm poses a higher risk but may undergo surgery if chordal preservation is likely. ACC/AHA guidelines recommend that patients with chronic MR who become symptomatic are candidates for corrective mitral surgery [1], even if the symptoms improve with medical therapy or the left ventricle appears to be compensated [1].
Surgery may be recommended in asymptomatic patients with preserved left ventricular function if the surgery performed in a center in which the likelihood of successful surgery is greater than 90 percent, otherwise; the patient can be safely treated with watchful waiting as long as the patient is carefully monitored [2]. The pstient should be seen every 6 to 12 months. Echocardiography should be obtained at these visits. The early surgery exposes the patient to perioperative morbidity and mortality as well as the long-term complications of a prosthetic valve. But it is important to have an objective measure of LV function in patients with asymptomatic MR, because there may be benefit from surgery prior to the onset of symptoms of the depression of the ventricular function in some cases. In patients with borderline values of ventricular size or function in whom access to such monitoring is limited; Surgery may be done earlier.
| Symptoms | LV EF | LVESD |
|---|---|---|
| NYHA II - IV | > 60 percent | < 45 mm |
| Asymptomatic or symptomatic | 50 - 60 percent | ≥ 45 mm |
| Asymptomatic or symptomatic | < 50 percent or ≥ 45 mm | |
| Pulmonary artery systolic pressure ≥ 50 mmHg | ||
The patient may also need valve surgery in the following conditions:
- The changes in the mitral valve are causing major heart symptoms, such as angina (chest pain), shortness of breath, fainting spells (syncope), or heart failure.
- Tests show that the changes in your mitral valve are beginning to seriously affect your heart function.
- The heart valve has been damaged by endocarditis (infection of the heart valve).
- The patient has received a new heart valve in the past, and it is not working well, or you have other problems such as blood clots, infection, or bleeding.
Mitral valve repair is recommended in following:
- Limited damage to certain areas of the mitral valve leaflets or chordae tendineae[4].
- Limited calcification of the leaflets or annulus.
- Prolapse of less than one-third of either leaflet.
- Pure annular dilatation.
- Valvular perforations.
- Incomplete papillary muscle rupture.
Mitral valve replacement is recommended in following:
- Extensive calcification or degeneration of a leaflet or annulus.
- Prolapse of more than one-third of the leaflet tissue.
- Extensive chordal fusion, calcification, or papillary muscle rupture.
- Extensive damage of mitral valve secondary to endocarditis.
Based on above, ACC/AHA 2008 guidelines[5] recommend mitral valve repair rather than mitral valve replacement if the anatomy is appropriate, including patients with rheumatic mitral valve disease[6] and mitral valve prolapse[7] (Grade 1C). The procedure should be performed at experienced surgical centers.
Preoperative preparation
The patient may need to have some tests before the procedure. The Cardiologist usually conducts a physical examination and diagnose the condition within few days, he or she will assess the general health of the patient and will recommend the most appropriate treatment for the patient and if he or she needs surgery. Some of the tests that can be done before the procedure include:
- Cardiac catheterization.
- Chest X-ray.
- Computed tomography (CT) scan.
- Echocardiogram (Doppler echocardiogram).
- Electrocardiogram (ECG).
- Electrophysiology tests.
- Exercise tests.
- Holter monitor.
- Magnetic resonance imaging (MRI).
Many patients with chronic MR requiring surgery also have coronary artery disease[8]. Usually coronary disease treated at the same operation if CABG (Coronary artery bypass grafting) is indicated. Studies showed that concurrent bypass surgery adds little morbidity to the valvular procedure and does not increase the mortality [1]. The 2006 ACC/AHA guidelines on the treatment of valvular heart disease included recommendations for coronary angiography prior to valve surgery in those who are suspected to have coronary artery disease and in those at risk for coronary disease [1]. A noninvasive angiography using computed tomography (CT) or magnetic resonance imaging may be an alternative.
Before the surgery:
- The surgeon needs to know if the patient is taking any drugs, supplements, or herbs before the procedure.
- The patient may be able to store blood in the blood bank for transfusions during and after the surgery. The family members can also donate blood (autologous donation).
- For the 2-week period before surgery, the patient should be asked to stop taking drugs that make it harder for the blood to clot. These might cause increased bleeding during the surgery. Some of these drugs are aspirin, ibuprofen (Advil, Motrin), and naproxen (Aleve, Naprosyn).
- The day before the surgery, the patient should shower and shampoo well and wash the whole body below the neck with a special soap.
- The patient may also be asked to take an antibiotic to guard against infection.
- The patient should be informed which drugs he or she should still take on the day of the surgery.
- The patient should stop smoking.
On the day of the surgery:
- An intravenous (IV) line will be placed into a blood vessel in the patient's arm or chest to give fluids and medicines.
- The patient should be asked not to drink or eat anything after midnight the night before surgery. This includes chewing gum and using breath mints. The patient can rinse mouth with water if it feels dry without swallowing.
- Make sure that the patient is taking the drugs that he or she needs to take with a small sip of water.
- Hair near the incision site may be shaved immediately before the surgery.
- The patient should be informed when to arrive to hospital on the day of the surgery.
The procedure
The Procedure can be done either by the traditional open heart surgery or by the Minimally invasive surgery. Before the surgery, the patient will receive general anesthesia. This will make the patient asleep and pain-free during the entire procedure.
- In thetraditional open heart surgery:
- The surgeon will make a 10-inch-long cut in the middle of the chest (sternum).
- Next, the surgeon will separate the breastbone (sternum) to be able to see the heart.
- Most people are connected to a heart-lung bypass machine or bypass pump. The heart is stopped while the patient is connected to this machine. This machine does the work of the heart while the heart is stopped.
- A small cut is made in the left side of the heart so the surgeon can repair or replace the mitral valve.
- In minimally invasive mitral valve surgery; there are several different ways to perform the procedure:
- The heart surgeon may make a 2-inch to 3-inch-long cut in the right part of your chest near the sternum (breastbone). Muscles in the area will be divided so the surgeon can reach the heart. A small cut is made in the left side of the heart so the surgeon can repair or replace the mitral valve.
- In Endoscopic surgery, the surgeon makes one to four small holes in the chest, then he or she uses special instruments and a camera to do the surgery.
- For Robotically-assisted valve surgery, the surgeon makes two to four tiny cuts (about a ½ to a ¾ inch) in the chest. The surgeon uses a special computer to control robotic arms during the surgery. The surgeon sees a three-dimensional view of the heart and mitral valve on the computer. This method is very precise.
The patient may or may not need to be on a heart-lung machine for these types of surgery, but if not, the heart rate will be slowed by medicine or a mechanical device.
If the surgeon can repair the mitral valve, the patient may have:
- Ring annuloplasty: The surgeon repairs the ring-like part around the valve by sewing a ring of metal, cloth, or tissue around the valve.
- Valve repair: The surgeon trims, shapes, or rebuilds one or more of the three leaflets of the valve. The leaflets are flaps that open and close the valve.
If the mitral valve is too damaged, the patient will need a new valve. This is called Replacement surgery. The surgeon will remove the mitral valve and sew a new one into place. There are two types of valves:
1. Mechanical which is made of man-made (synthetic) materials, such as a metal like titanium. These valves last the longest, but the patient will need to take blood-thinning medicine, such as warfarin (Coumadin) or aspirin, for the rest of his or her life.
2. Biological which made of human or animal tissue. These valves last 10 to 12 years, but the patient may not need to take blood thinners for life.
Once the new or repaired valve is working, the surgeon will:
- Close the heart and take you off the heart-lung machine.
- Place catheters (tubes) around the heart to drain fluids that build up.
- Close the sternum with stainless steel wires. It will take about 6 weeks for the bone to heal. The wires will stay inside the body.
The patient may have a temporary pacemaker connected to the heart until his or her natural heart rhythm returns.
The surgeon may also perform coronary artery bypass surgery at the same time, if needed.
Recovery
Recovery at hospital
The patient may spend 4 to 7 days in the hospital after surgery (much less in Minimally invasive mitral valve surgery-3 to 5 days). Then patient will wake up in the intensive care unit (ICU) and recover there for 1 or 2 days. Two to three tubes will be in the patient's chest to drain fluid from around the heart. They are usually removed 1 to 3 days after surgery.
The patient may have a catheter in the bladder to drain urine, and may also have intravenous lines to get fluids. Nurses will closely watch monitors that show information about the vital signs (pulse, temperature, and breathing).
The patient will be moved to a regular hospital room from the ICU. The nurses and doctors will continue to monitor the heart and vital signs until the patient is stable enough to go home. The patient will receive pain medicine to control pain around your surgical cut.
A nurse should help the patient to slowly resume some activity, and the patient should begin a physical therapy program to make the heart and body stronger. A temporary pacemaker may be placed in the patient's heart if the heart rate becomes too slow after surgery.
Recovery at home
The patient should be informed about the following:
- Taking care for his or her healing incisions.
- Recognizing signs of infection or other complications.
- Coping with after-effects of surgery.
- Followup appointments, medicines, and situations when he or she should call the doctor right away.
- When he or she can go back to daily routine, such as working, driving, and physical activity.
After-effects of heart surgery are normal. They may include muscle pain, chest pain, or swelling. Other after-effects may include loss of appetite, problems sleeping, constipation, and mood swings and depression. After-effects usually go away over time.
Less recovery time is needed for off-pump heart surgery and minimally invasive heart surgery.
Ongoing care
Ongoing care after valve surgery may include periodic checkups with the doctor. During these visits, the patient may have blood tests, an EKG (electrocardiogram), echocardiography, or a stress test. These tests will show how the patient's heart is working after the surgery.
Routine tests should be done to make sure the patient is getting the right amount of the blood-thinning medicine in case of mechanical valve placement.
The patient may be advised to change his or her lifestyle, this includes: quitting smoking, making changes to diet, being physically active, and reducing and managing stress.
Surgical outcome
The results of mitral valve repair are excellent in the centers that regularly perform this surgery.
Techniques for minimally invasive heart valve surgery have improved greatly over the past 10 years. These techniques are safe for most patients, and they reduce recovery time and pain.
Valve repair versus valve replacement
Advantages of Mitral valve repair include:
- Lower operative mortality rate [9][10]
- Improves left ventricular EF and function [11].
- Preserves native heart valve and avoids the use of a prosthetic heart valve with its complications.
- Has good overall outcome with good survival rates [12][7][13].
- Lower risk for endocarditis.
- Avoids long term use of anticoagulants.
Mechanical versus Biological valves
Mechanical heart valves do not fail often. They last from 12 to 20 years. However, blood clots develop on them. If a blood clot forms, the patient may have a stroke. Bleeding can occur, but this is rare. Biological valves tend to fail over time [14][15], but they have a lower risk of blood clots.
Possible complications
Risks for any surgery
- Blood clots in the legs that may travel to the lungs.
- Blood loss.
- Breathing problems.
- Infection, including in the lungs, kidneys, bladder, chest, or heart valves.
- Reactions to medicines.
Possible risks from having open-heart surgery
- Heart attack or stroke.
- Heart rhythm problems.
- Infection in the cut, which is more likely to happen in people who are obese, have diabetes, or have already had this surgery.
- Memory loss and loss of mental clarity, or "fuzzy thinking."
- Post-pericardiotomy syndrome, which is a low-grade fever and chest pain. This could last for up to 6 months.
Prosthetic heart valves are associated with a variety of complications
- Structural deterioration, particularly with bioprosthetic valves.
- Valve obstruction due to thrombosis or pannus formation.
- Systemic embolization.
- Bleeding.
- Endocarditis and other infections.
- Left ventricular systolic dysfunction, which may be preexisting.
- Hemolytic anemia.
Videos
- Minimally invasive mitral valve surgery (Right thoracotomy approach video)
<youtube v=EnJQh_W3r3A/>
- Robotic mitral valve repair surgery animation-(1)
<youtube v=VrIxRfWDOm8/>
- Robotic mitral valve repair surgery animation-(2)
<youtube v=GYAmSH2zwic/>
External links
http://en.wikipedia.org/wiki/Mitral_valve#cite_note-0
http://www.nlm.nih.gov/medlineplus/ency/article/000176.htm
http://www.nhlbi.nih.gov/health/health-topics/topics/hs/before.html
http://www.mayoclinic.org/mitral-valve-disease/
http://www.nlm.nih.gov/medlineplus/ency/article/007411.htm
http://www.nhlbi.nih.gov/health/health-topics/topics/hs/during.html
http://www.nhlbi.nih.gov/health/health-topics/topics/hs/after.html
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172.
- ↑ Rosenhek R, Rader F, Klaar U, Gabriel H, Krejc M, Kalbeck D; et al. (2006). "Outcome of watchful waiting in asymptomatic severe mitral regurgitation". Circulation. 113 (18): 2238–44. doi:10.1161/CIRCULATIONAHA.105.599175. PMID 16651470.
- ↑ "ACC/AHA guidelines for the management of patients with valvular heart disease. A report of the American College of Cardiology/American Heart Association. Task Force on Practice Guidelines (Committee on Management of Patients with Valvular Heart Disease)". Journal of the American College of Cardiology. 32 (5): 1486–588. 1998. PMID 9809971. Retrieved 2011-03-16. Unknown parameter
|month=ignored (help) - ↑ Gillinov AM, Faber C, Houghtaling PL, Blackstone EH, Lam BK, Diaz R; et al. (2003). "Repair versus replacement for degenerative mitral valve disease with coexisting ischemic heart disease". J Thorac Cardiovasc Surg. 125 (6): 1350–62. PMID 12830055.
- ↑ Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (13): e1–142. doi:10.1016/j.jacc.2008.05.007. PMID 18848134.
- ↑ Yau TM, El-Ghoneimi YA, Armstrong S, Ivanov J, David TE (2000). "Mitral valve repair and replacement for rheumatic disease". J Thorac Cardiovasc Surg. 119 (1): 53–60. PMID 10612761.
- ↑ 7.0 7.1 Mohty D, Orszulak TA, Schaff HV, Avierinos JF, Tajik JA, Enriquez-Sarano M (2001). "Very long-term survival and durability of mitral valve repair for mitral valve prolapse". Circulation. 104 (12 Suppl 1): I1–I7. PMID 11568020.
- ↑ Lin SS, Lauer MS, Asher CR, Cosgrove DM, Blackstone E, Thomas JD; et al. (2001). "Prediction of coronary artery disease in patients undergoing operations for mitral valve degeneration". J Thorac Cardiovasc Surg. 121 (5): 894–901. doi:10.1067/mtc.2001.112463. PMID 11326232.
- ↑ Tribouilloy CM, Enriquez-Sarano M, Schaff HV, Orszulak TA, Bailey KR, Tajik AJ; et al. (1999). "Impact of preoperative symptoms on survival after surgical correction of organic mitral regurgitation: rationale for optimizing surgical indications". Circulation. 99 (3): 400–5. PMID 9918527.
- ↑ Krayenbuehl HP (1986). "Surgery for mitral regurgitation. Repair versus valve replacement". Eur Heart J. 7 (8): 638–43. PMID 3769948.
- ↑ Enriquez-Sarano M, Schaff HV, Orszulak TA, Tajik AJ, Bailey KR, Frye RL (1995). "Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis". Circulation. 91 (4): 1022–8. PMID 7850937.
- ↑ Lee EM, Shapiro LM, Wells FC (1997). "Superiority of mitral valve repair in surgery for degenerative mitral regurgitation". Eur Heart J. 18 (4): 655–63. PMID 9129898.
- ↑ Thourani VH, Weintraub WS, Guyton RA, Jones EL, Williams WH, Elkabbani S; et al. (2003). "Outcomes and long-term survival for patients undergoing mitral valve repair versus replacement: effect of age and concomitant coronary artery bypass grafting". Circulation. 108 (3): 298–304. doi:10.1161/01.CIR.0000079169.15862.13. PMID 12835220.
- ↑ Hammermeister KE, Sethi GK, Henderson WG, Oprian C, Kim T, Rahimtoola S (1993). "A comparison of outcomes in men 11 years after heart-valve replacement with a mechanical valve or bioprosthesis. Veterans Affairs Cooperative Study on Valvular Heart Disease". N Engl J Med. 328 (18): 1289–96. doi:10.1056/NEJM199305063281801. PMID 8469251.
- ↑ Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C, Rahimtoola SH (2000). "Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial". J Am Coll Cardiol. 36 (4): 1152–8. PMID 11028464.