Lymphoma case study one: Difference between revisions
Apranta Deka (talk | contribs) No edit summary |
(Mahshid) |
||
| (34 intermediate revisions by 3 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; '''Associate Editor-In Chief:''' Apranta Deka Patel, M.B.B.S, M.D. | {{CMG}}; '''Associate Editor-In Chief:''' Apranta Deka Patel, M.B.B.S, M.D. | ||
== | ==Primary Cardiac Lymphoma- Rare EBV-negative Post-transplant Lymphoproliferative Disorder== | ||
===Case Presentation=== | ===Case Presentation=== | ||
A 77-year-old woman with past medical history of [[hypertension]], [[diabetes mellitus]] | A 77-year-old woman with past medical history of [[hypertension]], [[diabetes mellitus]] and [[autoimmune hepatitis]] status-post [[liver transplant]] presented to the [[Emergency Department]] for symptoms of worsening [[dyspnea on exertion]] progressing to [[shortness of breath]] at rest and [[pleuritic chest pain]] over the course of three months. Review of systems was otherwise negative. | ||
Her home medications included [[tacrolimus]], [[mycophenolate]], [[amlodipine]], [[valsartan]], [[metoprolol]], [[atorvastatin]], [[metformin]], [[glipizide]] and [[levothyroxine]]. | Her home medications included [[tacrolimus]], [[mycophenolate]], [[amlodipine]], [[valsartan]], [[metoprolol]], [[atorvastatin]], [[metformin]], [[glipizide]] and [[levothyroxine]]. | ||
| Line 13: | Line 13: | ||
===Past Medical History=== | ===Past Medical History=== | ||
Other than what is mentioned above, her [[autoimmune hepatitis]] was complicated by liver [[cirrhosis]] for which she had an orthotopic liver transplant four years prior to this presentation. [[Hepatocellular carcinoma]] and [[mixed cholangiocarcinoma]] were found on the explant with no evidence of spread. Post-transplant course was otherwise uncomplicated on stable doses of [[immunosuppresants]], [[tacrolimus]] and [[mycophenolate]]. | Other than what is mentioned above, her [[autoimmune hepatitis]] was complicated by liver [[cirrhosis]] for which she had an orthotopic [[liver transplant]] four years prior to this presentation. [[Hepatocellular carcinoma]] and [[mixed cholangiocarcinoma]] were found on the explant with no evidence of spread. Post-transplant course was otherwise uncomplicated on stable doses of [[immunosuppresants]], [[tacrolimus]] and [[mycophenolate]]. | ||
===Physical Examination=== | ===Physical Examination=== | ||
Vitals were stable with [[blood pressure]] of 155/100 mmHg, [[heart rate]] of 87 /min, mild [[tachypnea]] and [[oxygen saturation]] of 98% on room air. No [[pallor]], [[icterus]] or [[ | Vitals were stable with [[blood pressure]] of 155/100 mmHg, [[heart rate]] of 87 /min, mild [[tachypnea]] and [[oxygen saturation]] of 98% on room air. No [[pallor]], [[icterus]] or palpable [[lymph nodes]] were found on exam. Lung, abdominal and neurologic exams were normal. No [[pedal edema]] or [[jugular venous distension]] was noted. Heart sounds [[S1]] and [[S2]] were normal without any [[murmurs]], [[rubs]] or [[gallops]]. | ||
===Laboratory and Imaging Findings=== | ===Laboratory and Imaging Findings=== | ||
Initial laboratory evaluation revealed normal values for [[complete blood count]], [[liver function | Initial laboratory evaluation revealed normal values for [[complete blood count]], [[liver function tests]] and renal function panel but showed elevated [[D-dimer]] level at 1445 mg/mL (ref range 0-500 ng/mL). | ||
====CT Angiography==== | |||
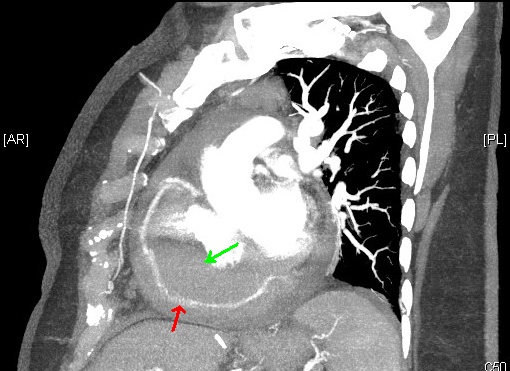
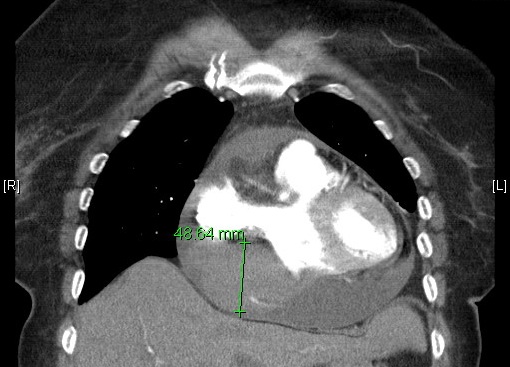
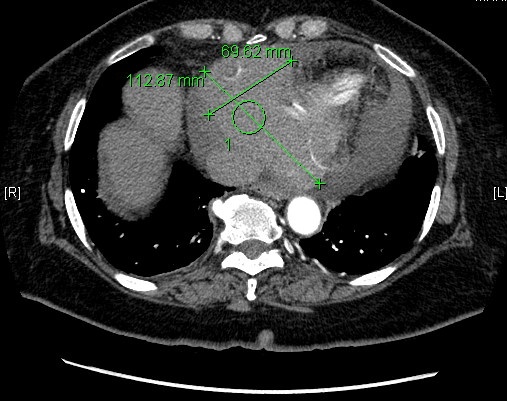
[[Computed tomography angiography]] was performed which ruled out [[pulmonary embolism]] but revealed a cardiac mass indenting the right heart chambers, extending [[inferiorly]] from the region of the [[atrioventricular groove]] along the right base of the heart measuring approximately 11x 7x 5 cm. This mass was noted to be encasing the [[right coronary artery]]. | [[Computed tomography angiography]] was performed which ruled out [[pulmonary embolism]] but revealed a cardiac mass indenting the right heart chambers, extending [[inferiorly]] from the region of the [[atrioventricular groove]] along the right base of the heart measuring approximately 11x 7x 5 cm. This mass was noted to be encasing the [[right coronary artery]]. | ||
[[Transthoracic echocardiogram]] also demonstrated a large | {{Gallery | ||
|title= | |||
|width=200 | |||
|height=200 | |||
|lines=4 | |||
|align=left | |||
|File:CTA_sagittal_PTLD_RCA.jpg|alt1=CTA sagittal section showing cardiac mass (green arrow) encasing the right coronary artery (red arrow).|CTA sagittal section showing cardiac mass (green arrow) encasing the right coronary artery (red arrow). | |||
|File:CTA_coronal_section_PTLD.jpg|alt2=CTA coronal section showing cardiac mass external to the right atrium (with measurements).|CTA coronal section showing cardiac mass external to the right atrium (with measurements). | |||
|File:CTA_cross_sectionPTLD.jpg|alt3=CTA cross-section showing cardiac mass external with measurements.|CTA cross-section showing cardiac mass external with measurements. | |||
}} | |||
<br /> <br /> <br /> <br /><br /> <br /> <br /> <br /><br /> <br /> <br /> <br /><br /> <br /> <br /> <br /><br /><!-- a br refers to a line break; these were added to add some spacing around your pictures ---> | |||
====Transthoracic echocardiogram==== | |||
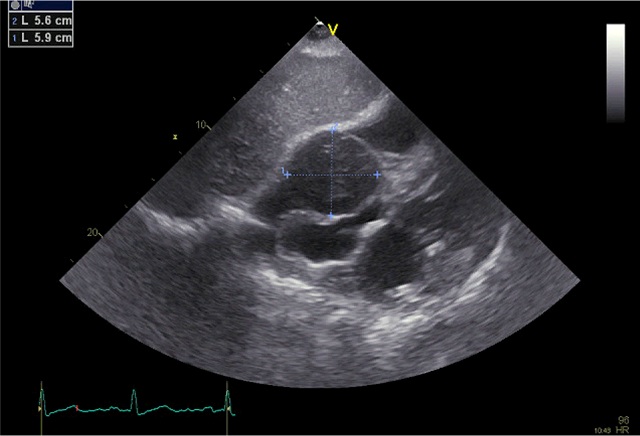
[[TTE|Transthoracic echocardiogram]] also demonstrated a large hypoechoic mass likely external to the [[right atrium]] arising from the region of the [[atrioventricular groove]] and compressing the [[right atrium]]. The [[left ventricular ejection fraction]] was normal. There was a loculated [[pericardial effusion]] measuring 3cm adjacent to the [[right ventricle]] with no clear signs of [[tamponade]]. | |||
== | [[Image:Subcostal_TTE.jpg||thumb|left|upright=1.8|Transthoracic echocardiography subcostal view showing the cardiac mass adjacent to and compressing the right atrium]] | ||
<br /> <br /> <br /> <br /><br /><br /> <br /><br /><br /> <br /><br /><br /> <br /><br /><br /> | |||
====CMR==== | |||
[[Cardiac magnetic resonance imaging]] was performed which stated a similar size with more details of the extent of the mass which was noted to invade the right [[atrial]] as well and right and left ventricular apical myocardium. | |||
[[Image:CardiacMRI_massPTLD.jpg|thumb|left|upright=1.0|Cardiac MRI showing cardiac mass invading right atrial and right and left ventricular apical myocardium with compression of right atrial chamber]] | |||
<br /> <br /> <br /> <br /><br /><br /> <br /><br /><br /> <br /><br /><br /> <br /><br /><br /><br /> | |||
===Diagnosis and Management=== | |||
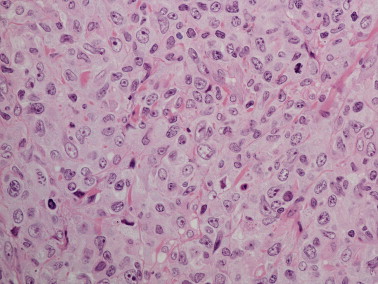
[[Image:Monomorphic_high_grade_PTLD.jpg|thumb|left|upright=1.0|Pathology:Monomorphic high grade B cell PTLD]] | |||
A [[sternotomy]] was performed with the plan for debulking and procuring tissue for [[biopsy]]. However, during induction of anesthesia, this was complicated by tamponade physiology needing emergent [[pericardiotomy]] which yielded serosanguinous fluid. Attempt at debulking failed due to friable cardiac tissue, but tissue for pathology was obtained. | |||
Biopsy of cardiac mass revealed monomorphic PTLD or [[Post-transplant lymphoproliferative disorder]] of high grade [[large B-cell lymphoma]] type. Pending EBV ([[Epstein-Barr virus]]) status test results, the patient was initiated on [[rituximab]] with the plan to follow it up with [[CHOP]]21 ([[cyclophosphamide]], [[doxorubicin]], [[vincristine]] and [[prednisolone]]) for four cycles with the presumption of EBV positivity. | |||
However, the blood [[EBV]] [[PCR]] and EBER ISH (EBV-encoded, nonpolyadenylated RNAs) tests came back negative and rituximab was stopped. Modified [[CHOP]] regimen was started and is currently ongoing pending tumor response. | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category: | [[Category:Up-To-Date]] | ||
[[Category: | [[Category:Oncology]] | ||
[[Category:Medicine]] | |||
[[Category:Hematology]] | [[Category:Hematology]] | ||
[[Category: | [[Category:Immunology]] | ||
Latest revision as of 02:24, 27 November 2017
|
Lymphoma Main Page |
|
Case Studies |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In Chief: Apranta Deka Patel, M.B.B.S, M.D.
Primary Cardiac Lymphoma- Rare EBV-negative Post-transplant Lymphoproliferative Disorder
Case Presentation
A 77-year-old woman with past medical history of hypertension, diabetes mellitus and autoimmune hepatitis status-post liver transplant presented to the Emergency Department for symptoms of worsening dyspnea on exertion progressing to shortness of breath at rest and pleuritic chest pain over the course of three months. Review of systems was otherwise negative.
Her home medications included tacrolimus, mycophenolate, amlodipine, valsartan, metoprolol, atorvastatin, metformin, glipizide and levothyroxine.
Past Medical History
Other than what is mentioned above, her autoimmune hepatitis was complicated by liver cirrhosis for which she had an orthotopic liver transplant four years prior to this presentation. Hepatocellular carcinoma and mixed cholangiocarcinoma were found on the explant with no evidence of spread. Post-transplant course was otherwise uncomplicated on stable doses of immunosuppresants, tacrolimus and mycophenolate.
Physical Examination
Vitals were stable with blood pressure of 155/100 mmHg, heart rate of 87 /min, mild tachypnea and oxygen saturation of 98% on room air. No pallor, icterus or palpable lymph nodes were found on exam. Lung, abdominal and neurologic exams were normal. No pedal edema or jugular venous distension was noted. Heart sounds S1 and S2 were normal without any murmurs, rubs or gallops.
Laboratory and Imaging Findings
Initial laboratory evaluation revealed normal values for complete blood count, liver function tests and renal function panel but showed elevated D-dimer level at 1445 mg/mL (ref range 0-500 ng/mL).
CT Angiography
Computed tomography angiography was performed which ruled out pulmonary embolism but revealed a cardiac mass indenting the right heart chambers, extending inferiorly from the region of the atrioventricular groove along the right base of the heart measuring approximately 11x 7x 5 cm. This mass was noted to be encasing the right coronary artery.
Transthoracic echocardiogram
Transthoracic echocardiogram also demonstrated a large hypoechoic mass likely external to the right atrium arising from the region of the atrioventricular groove and compressing the right atrium. The left ventricular ejection fraction was normal. There was a loculated pericardial effusion measuring 3cm adjacent to the right ventricle with no clear signs of tamponade.
CMR
Cardiac magnetic resonance imaging was performed which stated a similar size with more details of the extent of the mass which was noted to invade the right atrial as well and right and left ventricular apical myocardium.

Diagnosis and Management
A sternotomy was performed with the plan for debulking and procuring tissue for biopsy. However, during induction of anesthesia, this was complicated by tamponade physiology needing emergent pericardiotomy which yielded serosanguinous fluid. Attempt at debulking failed due to friable cardiac tissue, but tissue for pathology was obtained.
Biopsy of cardiac mass revealed monomorphic PTLD or Post-transplant lymphoproliferative disorder of high grade large B-cell lymphoma type. Pending EBV (Epstein-Barr virus) status test results, the patient was initiated on rituximab with the plan to follow it up with CHOP21 (cyclophosphamide, doxorubicin, vincristine and prednisolone) for four cycles with the presumption of EBV positivity.
However, the blood EBV PCR and EBER ISH (EBV-encoded, nonpolyadenylated RNAs) tests came back negative and rituximab was stopped. Modified CHOP regimen was started and is currently ongoing pending tumor response.