Hyperkalemia
| Hyperkalemia | |
 | |
|---|---|
| potassium | |
| ICD-10 | E87.5 |
| ICD-9 | 276.7 |
| DiseasesDB | 6242 |
| MeSH | D006947 |
|
Hyperkalemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hyperkalemia On the Web |
|
American Roentgen Ray Society Images of Hyperkalemia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Priyamvada Singh, M.B.B.S. [2]
Overview
Pathophysiology
Causes
Differential diagnosis
History and Symptoms
Diagnosis
In order to gather enough information for diagnosis, the measurement of potassium needs to be repeated, as the elevation can be due to hemolysis in the first sample. Generally, blood tests for renal function (creatinine, blood urea nitrogen), glucose and occasionally creatine kinase and cortisol will be performed. Calculating the trans-tubular potassium gradient can sometimes help in distinguishing the cause of the hyperkalemia.
In many cases, renal ultrasound will be performed, since hyperkalemia is highly suggestive of renal failure.
Also, electrocardiography (EKG/ECG) may be performed to determine if there is a significant risk of cardiac arrhythmias (see ECG/EKG Findings, below).
Lab tests
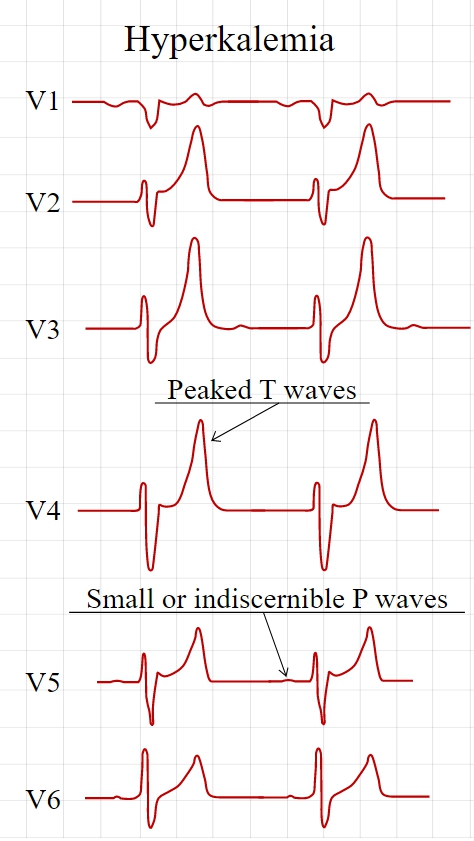
Electrocardiographic Findings
Electrocardiography (ECG) is generally done early to identify any influences on the heart, as hyperkalemia may cause fatal arrhythmias. With moderate hyperkalemia, there is reduction of the size of the P wave and development of tent-shaped T waves. Further hyperkalemia will lead to widening of the QRS complex, that ultimately may become sinusoidal in shape. There appears to be a direct effect of elevated potassium on some of the potassium channels that increases their activity and speeds membrane repolarization. Also, (as noted above), hyperkalemia causes an overall membrane depolarization that inactivates many sodium channels. The faster repolarization of the cardiac action potential causes the tenting of the T waves, and the inactivation of sodium channels causes a sluggish conduction of the electrical wave around the heart, which leads to smaller P waves and widening of the QRS complex.
Spcific findings include the following:
Tall, narrow, and peaked T waves
- Earliest sign of hyperkalemia
- Occurs with K > 5.5 meq/li
- Differential diagnosis of this EKG change includes the T wave changes of bradycardia or stroke. Prominent U waves and QTc prolongation are more consistent with stroke than hyperkalemia.
Intraventricular conduction defect
Decrease of the amplitude of the P wave or an absent P wave
- Decreased P wave amplitude occurs when the K is > 7.0 meq/li
- P waves may be absent when the K is > 8.8 meq/li
- The impulses are still being generated in the SA node and are conducted to the ventricles through specialized atrial fibers without depolarizing the atrial muscle
- Moderate or sever hyperkalemia can cause sinus arrest [1]
ST segment changes simulating current of injury
- Have been labeled the dialyzable current of injury
Cardiac arrhythmias: bradyarrhythmias, tachyarrhythmias, atrioventricular conduction defects
- Occurs with severe hyperkalemia, not mild to moderate hyperkalemia
-
Tall, symmetric, narrow based T waves in a hyperkalemic patient.
-
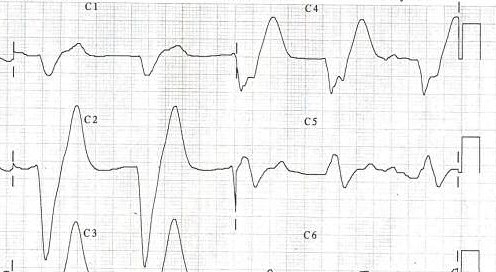
A patient's EKG with hyperkalemia.
-
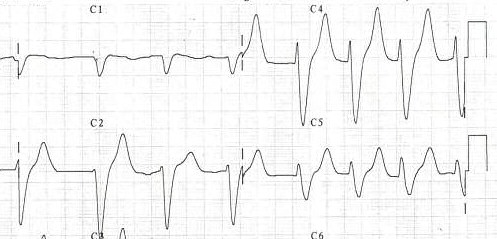
Same patient's EKG during treatment.
Treatment
When arrhythmias occur, or when potassium levels exceed 6.5 mmol/l, emergency lowering of potassium levels is mandated. Several agents are used to lower K levels. Choice depends on the degree and cause of the hyperkalemia, and other aspects of the patient's condition.
- Calcium supplementation (calcium gluconate 10% (10ml), preferably through a central venous catheter as the calcium may cause phlebitis) does not lower potassium but decreases myocardial excitability, protecting against life threatening arrhythmias.
- Insulin (e.g. intravenous injection of 10-15u of (short acting) insulin (e.g. Actrapid) {along with 50ml of 50% dextrose to prevent hypoglycemia}) will lead to a shift of potassium ions into cells, secondary to increased activity of the sodium-potassium ATPase.
- Bicarbonate therapy (e.g. 1 ampule (45mEq) infused over 5 minutes) is effective in cases of metabolic acidosis. The bicarbonate ion will stimulate an exchange of cellular H+ for Na+, thus leading to stimulation of the sodium-potassium ATPase.
- Salbutamol (albuterol, Ventolin®) is a β2-selective catacholamine that is administered by nebuliser (e.g. 10-20 mg). This drug promotes movement of K into cells, lowering the blood levels.
- Polystyrene sulfonate (Calcium Resonium, Kayexalate) is a binding resin that binds K within the intestine and removes it from the body by defecation. Calcium Resonium (15g three times a day in water) can be given by mouth. Kayexelate can be given by mouth or as an enema. In both cases, the resin absorbs K within the intestine and carries it out of the body by defecation. This medication may cause diarrhea.
- Refractory or severe cases may need dialysis to remove the potassium from the circulation.
- Preventing recurrence of hyperkalemia typically involves reduction of dietary potassium, removal of an offending medication, and/or the addition of a diuretic (such as furosemide (Lasix®) or hydrochlorothiazide).
See also
References
- ↑ Bonvini RF, Hendiri T, Anwar A (2006). "Sinus arrest and moderate hyperkalemia". Annales De Cardiologie Et D'angéiologie. 55 (3): 161–3. PMID 16792034. Unknown parameter
|month=ignored (help)
Template:Endocrine, nutritional and metabolic pathology