HIV AIDS: Difference between revisions
| Line 45: | Line 45: | ||
==[[AIDS causes|Causes of AIDS]]== | ==[[AIDS causes|Causes of AIDS]]== | ||
== | ==[[AIDS classification|Classification]]== | ||
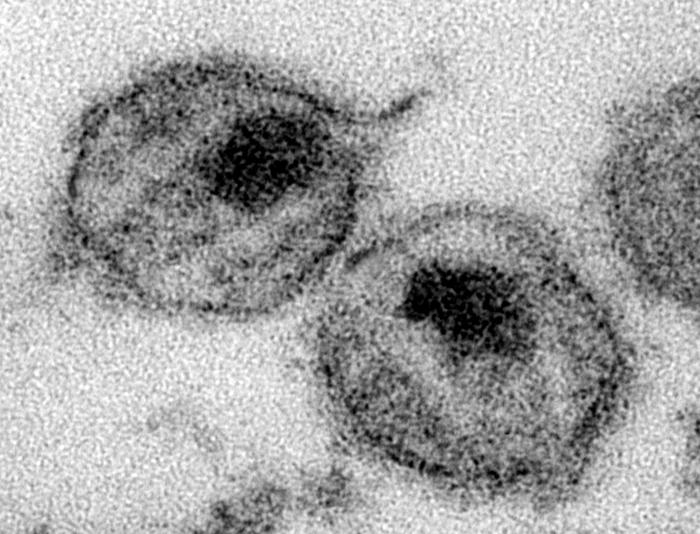
[[Image:TEM HIV.jpg|thumb|200px|Thin-section transmission electron micrograph (TEM) depicting the ultrastructural details of two ”human immunodeficiency virus” (HIV) virions]] | [[Image:TEM HIV.jpg|thumb|200px|Thin-section transmission electron micrograph (TEM) depicting the ultrastructural details of two ”human immunodeficiency virus” (HIV) virions]] | ||
[[Image:Kaposi's_sarcoma.jpg|thumb|Kaposi's sarcoma lesion commonly found in patients with stage IV AIDS]] | [[Image:Kaposi's_sarcoma.jpg|thumb|Kaposi's sarcoma lesion commonly found in patients with stage IV AIDS]] | ||
Revision as of 19:52, 7 January 2012
|
AIDS Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
HIV AIDS On the Web |
|
American Roentgen Ray Society Images of HIV AIDS |
| Acquired immunodeficiency syndrome (AIDS) | |
 | |
|---|---|
| The Red ribbon is a symbol for solidarity with HIV-positive people and those living with AIDS. | |
| ICD-10 | B24 |
| ICD-9 | 042 |
| DiseasesDB | 5938 |
| List of abbreviations used in this article AIDS: Acquired immune deficiency syndrome |
For AIDS Patient Information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Historical perspective
Epidemiology & Demographics
Pathophysiology
History and Symptoms
Causes of AIDS
Classification

Since June 5, 1981, many definitions have been developed for epidemiological surveillance such as the Bangui definition and the 1994 expanded World Health Organization AIDS case definition. However, clinical staging of patients was not an intended use for these systems as they are neither sensitive, nor specific. In developing countries, the World Health Organization staging system for HIV infection and disease, using clinical and laboratory data, is used and in developed countries, the Centers for Disease Control (CDC) Classification System is used.
WHO disease staging system for HIV infection and disease
In 1990, the World Health Organization (WHO) grouped these infections and conditions together by introducing a staging system for patients infected with HIV-1.[1] An update took place in September 2005. Most of these conditions are opportunistic infections that are easily treatable in healthy people.
- Stage I: HIV infection is asymptomatic and not categorized as AIDS
- Stage II: includes minor mucocutaneous manifestations and recurrent upper respiratory tract infections
- Stage III: includes unexplained chronic diarrhea for longer than a month, severe bacterial infections and pulmonary tuberculosis
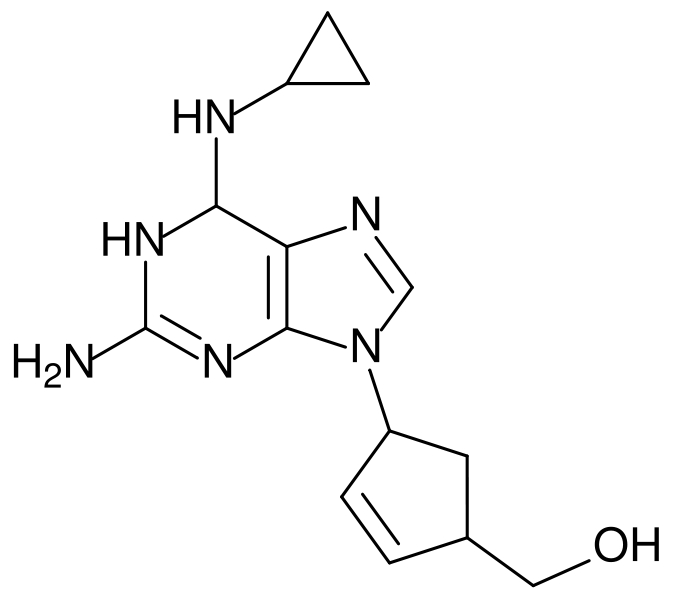
- Stage IV: includes toxoplasmosis of the brain, candidiasis of the esophagus, trachea, bronchi or lungs and Kaposi's sarcoma; these diseases are indicators of AIDS.
CDC classification system for HIV infection
In the beginning, the Centers for Disease Control and Prevention (CDC) did not have an official name for the disease, often referring to it by way of the diseases that were associated with it, for example, lymphadenopathy, the disease after which the discoverers of HIV originally named the virus.[2][3] They also used Kaposi's Sarcoma and Opportunistic Infections, the name by which a task force had been set up in 1981.[4] In the general press, the term GRID, which stood for Gay-related immune deficiency, had been coined.[5] However, after determining that AIDS was not isolated to the homosexual community,[4] the term GRID became misleading and AIDS was introduced at a meeting in July 1982.[6] By September 1982 the CDC started using the name AIDS, and properly defined the illness.[7] In 1993, the CDC expanded their definition of AIDS to include all HIV positive people with a CD4+ T cell count below 200 per µL of blood or 14% of all lymphocytes.[8] The majority of new AIDS cases in developed countries use either this definition or the pre-1993 CDC definition. The AIDS diagnosis still stands even if, after treatment, the CD4+ T cell count rises to above 200 per µL of blood or other AIDS-defining illnesses are cured.
HIV test
Many people are unaware that they are infected with HIV.[9] Less than 1% of the sexually active urban population in Africa has been tested, and this proportion is even lower in rural populations. Furthermore, only 0.5% of pregnant women attending urban health facilities are counseled, tested or receive their test results. Again, this proportion is even lower in rural health facilities.[9] Therefore, donor blood and blood products used in medicine and medical research are screened for HIV.
HIV tests are usually performed on venous blood. Many laboratories use fourth generation screening tests which detect anti-HIV antibody (IgG and IgM) and the HIV p24 antigen. The detection of HIV antibody or antigen in a patient previously known to be negative is evidence of HIV infection. Individuals whose first specimen indicates evidence of HIV infection will have a repeat test on a second blood sample to confirm the results. The window period (the time between initial infection and the development of detectable antibodies against the infection) can vary since it can take 3–6 months to seroconvert and to test positive. Detection of the virus using polymerase chain reaction (PCR) during the window period is possible, and evidence suggests that an infection may often be detected earlier than when using a fourth generation EIA screening test. Positive results obtained by PCR are confirmed by antibody tests.[10] Routinely used HIV tests for infection in neonates, born to HIV-positive mothers, have no value because of the presence of maternal antibody to HIV in the child's blood. HIV infection can only be diagnosed by PCR, testing for HIV pro-viral DNA in the children's lymphocytes.[11]
Transmission and prevention
| Exposure Route | Estimated infections per 10,000 exposures to an infected source | |||
|---|---|---|---|---|
| Blood Transfusion | 9,000[13] | |||
| Childbirth | 2,500[14] | |||
| Needle-sharing injection drug use | 67[15] | |||
| Percutaneous needle stick | 30[16] | |||
| Receptive anal intercourse* | 50[17][18] | |||
| Insertive anal intercourse* | 6.5[17][18] | |||
| Receptive penile-vaginal intercourse* | 10[17][18][19] | |||
| Insertive penile-vaginal intercourse* | 5[17][18] | |||
| Receptive oral intercourse*§ | 1[18] | |||
| Insertive oral intercourse* | 0.5[18]§ | |||
| * assuming no condom use § source refers to oral intercourse performed on a man | ||||
The three main transmission routes of HIV are sexual contact, exposure to infected body fluids or tissues, and from mother to fetus or child during perinatal period. It is possible to find HIV in the saliva, tears, and urine of infected individuals, but there are no recorded cases of infection by these secretions, and the risk of infection is negligible.[20]
Sexual contact
The majority of HIV infections are acquired through unprotected sexual relations between partners, one of whom has HIV. The primary mode of HIV infection worldwide is through sexual contact between members of the opposite sex.[21][22][23] Sexual transmission occurs with the contact between sexual secretions of one partner with the rectal, genital or oral mucous membranes of another. Unprotected receptive sexual acts are riskier than unprotected insertive sexual acts, with the risk for transmitting HIV from an infected partner to an uninfected partner through unprotected anal intercourse greater than the risk for transmission through vaginal intercourse or oral sex. Oral sex is not without its risks as HIV is transmissible through both insertive and receptive oral sex.[24] The risk of HIV transmission from exposure to saliva is considerably smaller than the risk from exposure to semen; contrary to popular belief, one would have to swallow liters of saliva from a carrier to run a significant risk of becoming infected.[25]
Approximately 30% of women in ten countries representing "diverse cultural, geographical and urban/rural settings" report that their first sexual experience was forced or coerced, making sexual violence a key driver of the HIV/AIDS pandemic.[26] Sexual assault greatly increases the risk of HIV transmission as protection is rarely employed and physical trauma to the vaginal cavity frequently occurs which facilitates the transmission of HIV.[27]
Sexually transmitted infections (STI) increase the risk of HIV transmission and infection because they cause the disruption of the normal epithelial barrier by genital ulceration and/or microulceration; and by accumulation of pools of HIV-susceptible or HIV-infected cells (lymphocytes and macrophages) in semen and vaginal secretions. Epidemiological studies from sub-Saharan Africa, Europe and North America have suggested that there is approximately a four times greater risk of becoming infected with HIV in the presence of a genital ulcer such as those caused by syphilis and/or chancroid. There is also a significant though lesser increased risk in the presence of STIs such as gonorrhea, Chlamydial infection and trichomoniasis which cause local accumulations of lymphocytes and macrophages.[28]
Transmission of HIV depends on the infectiousness of the index case and the susceptibility of the uninfected partner. Infectivity seems to vary during the course of illness and is not constant between individuals. An undetectable plasma viral load does not necessarily indicate a low viral load in the seminal liquid or genital secretions. Each 10-fold increment of blood plasma HIV RNA is associated with an 81% increased rate of HIV transmission.[28][29] Women are more susceptible to HIV-1 infection due to hormonal changes, vaginal microbial ecology and physiology, and a higher prevalence of sexually transmitted diseases.[30][31] People who are infected with HIV can still be infected by other, more virulent strains.
During a sexual act, only male or female condoms can reduce the chances of infection with HIV and other STDs and the chances of becoming pregnant. The best evidence to date indicates that typical condom use reduces the risk of heterosexual HIV transmission by approximately 80% over the long-term, though the benefit is likely to be higher if condoms are used correctly on every occasion.[32] The effective use of condoms and screening of blood transfusion in North America, Western and Central Europe is credited with contributing to the low rates of AIDS in these regions. Promoting condom use, however, has often proved controversial and difficult. Many religious groups, most noticeably the Roman Catholic Church, have opposed the use of condoms on religious grounds, and have sometimes seen condom promotion as an affront to the promotion of marriage, monogamy and sexual morality. Defenders of the Catholic Church's role in AIDS and general STD prevention state that, while they may be against the use of contraception, they are strong advocates of abstinence outside marriage.[33] This attitude is also found among some health care providers and policy makers in sub-Saharan African nations, where HIV and AIDS prevalence is extremely high.[34] They also believe that the distribution and promotion of condoms is tantamount to promoting sex amongst the youth and sending the wrong message to uninfected individuals. However, no evidence has been produced that promotion of condom use increases sexual promiscuity,[35] and abstinence-only programs have been unsuccessful in the United States both in changing sexual behavior and in reducing HIV transmission.[36] Evaluations of several abstinence-only programs in the US showed a negative impact on the willingness of youths to use contraceptives, due to the emphasis on contraceptives' failure rates.[37] The male latex condom, if used correctly without oil-based lubricants, is the single most effective available technology to reduce the sexual transmission of HIV and other sexually transmitted infections. Manufacturers recommend that oil-based lubricants such as petroleum jelly, butter, and lard not be used with latex condoms, because they dissolve the latex, making the condoms porous. If necessary, manufacturers recommend using water-based lubricants. Oil-based lubricants can however be used with polyurethane condoms.[38] Latex condoms degrade over time, making them porous, which is why condoms have expiration dates. In Europe and the United States, condoms have to conform to European (EC 600) or American (D3492) standards to be considered protective against HIV transmission.
The female condom is an alternative to the male condom and is made from polyurethane, which allows it to be used in the presence of oil-based lubricants. They are larger than male condoms and have a stiffened ring-shaped opening, and are designed to be inserted into the vagina. The female condom contains an inner ring, which keeps the condom in place inside the vagina – inserting the female condom requires squeezing this ring. However, at present availability of female condoms is very low and the price remains prohibitive for many women. Preliminary studies suggest that, where female condoms are available, overall protected sexual acts increase relative to unprotected sexual acts, making them an important HIV prevention strategy.[39]
With consistent and correct use of condoms, there is a very low risk of HIV infection. Studies on couples where one partner is infected show that with consistent condom use, HIV infection rates for the uninfected partner are below 1% per year.[40]
In December 2006, the last of three large, randomized trials confirmed that male circumcision lowers the risk of HIV infection among heterosexual African men by around 50%. It is expected that this intervention will be actively promoted in many of the countries worst affected by HIV, although doing so will involve confronting a number of practical, cultural and attitudinal issues. Some experts fear that a lower perception of vulnerability among circumcised men may result in more sexual risk-taking behavior, thus negating its preventive effects.[41] Furthermore, South African medical experts are concerned that the repeated use of unsterilized blades in the ritual circumcision of adolescent boys may be spreading HIV.[42]
Prevention strategies are well-known in developed countries, however, recent epidemiological and behavioral studies in Europe and North America have suggested that a substantial minority of young people continue to engage in high-risk practices and that despite HIV/AIDS knowledge, young people underestimate their own risk of becoming infected with HIV.[43]
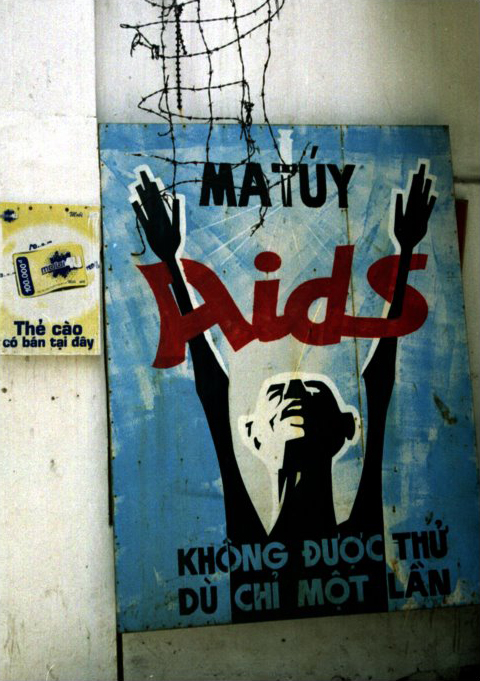
Exposure to infected body fluids

This transmission route is particularly relevant to intravenous drug users, hemophiliacs and recipients of blood transfusions and blood products. Sharing and reusing syringes contaminated with HIV-infected blood represents a major risk for infection with not only HIV, but also hepatitis B and hepatitis C. Needle sharing is the cause of one third of all new HIV-infections and 50% of hepatitis C infections in North America, China, and Eastern Europe. The risk of being infected with HIV from a single prick with a needle that has been used on an HIV-infected person is thought to be about 1 in 150 (see table above). Post-exposure prophylaxis with anti-HIV drugs can further reduce that small risk.[44] Health care workers (nurses, laboratory workers, doctors etc) are also concerned, although more rarely. This route can affect people who give and receive tattoos and piercings. Universal precautions are frequently not followed in both sub-Saharan Africa and much of Asia because of both a shortage of supplies and inadequate training. The WHO estimates that approximately 2.5% of all HIV infections in sub-Saharan Africa are transmitted through unsafe healthcare injections.[45] Because of this, the United Nations General Assembly, supported by universal medical opinion on the matter, has urged the nations of the world to implement universal precautions to prevent HIV transmission in health care settings.[46] Drug abuse has an additional effect of an increased tendency to engage in unprotected sexual intercourse.[47]
The risk of transmitting HIV to blood transfusion recipients is extremely low in developed countries where improved donor selection and HIV screening is performed. However, according to the WHO, the overwhelming majority of the world's population does not have access to safe blood and "between 5% and 10% of HIV infections worldwide are transmitted through the transfusion of infected blood and blood products".[48]
Medical workers who follow universal precautions or body-substance isolation, such as wearing latex gloves when giving injections and washing the hands frequently, can help prevent infection by HIV.
All AIDS-prevention organizations advise drug-users not to share needles and other material required to prepare and take drugs (including syringes, cotton balls, the spoons, water for diluting the drug, straws, crack pipes, etc). It is important that people use new or properly sterilized needles for each injection. Information on cleaning needles using bleach is available from health care and addiction professionals and from needle exchanges. In some developed countries, clean needles are available free in some cities, at needle exchanges or safe injection sites. Additionally, many nations have decriminalized needle possession and made it possible to buy injection equipment from pharmacists without a prescription.
Transmission of HIV between intravenous drug users has clearly decreased, and HIV transmission by blood transfusion has become quite rare in developed countries.
Mother-to-child transmission (MTCT)
The transmission of the virus from the mother to the child can occur in utero during the last weeks of pregnancy and at childbirth. In the absence of treatment, the transmission rate between the mother to the child during pregnancy, labor and delivery is 25%. However, when the mother has access to antiretroviral therapy and gives birth by caesarean section, the rate of transmission is just 1%.[14] A number of factors influence the risk of infection, particularly the viral load of the mother at birth (the higher the viral load, the higher the risk). Breastfeeding increases the risk of transmission by 4.04%.[49] This risk depends on clinical factors and may vary according to the pattern and duration of breast-feeding.[49]
Studies have shown that antiretroviral drugs, caesarean delivery and formula feeding reduce the chance of transmission of HIV from mother to child.[50] Current recommendations state that when replacement feeding is acceptable, feasible, affordable, sustainable and safe, HIV-infected mothers should avoid breast-feeding their infant. However, if this is not the case, exclusive breast-feeding is recommended during the first months of life and discontinued as soon as possible.[51] In 2005, around 700,000 children under 15 contracted HIV, mainly through MTCT, with 630,000 of these infections occurring in Africa.[52] Of the children currently living with HIV, almost 90% live in sub-Saharan Africa.[53]
In Africa, the number of MTCT and the prevalence of AIDS is beginning to reverse decades of steady progress in child survival.[54] Countries such as Uganda are attempting to curb the MTCT epidemic by offering VCT (voluntary counseling and testing), PMTCT (prevention of mother-to-child transmission) and ANC (ante-natal care) services, which include the distribution of antiretroviral therapy.
Treatment
- See also HIV Treatment and Antiretroviral drug.

There is currently no vaccine or cure for HIV or AIDS. The only known methods of prevention are based on avoiding exposure to the virus or, failing that, an antiretroviral treatment directly after a highly significant exposure, called post-exposure prophylaxis (PEP).[44] PEP has a very demanding four week schedule of dosage. It also has very unpleasant side effects including diarrhea, malaise, nausea and fatigue.[55]
Current treatment for HIV infection consists of highly active antiretroviral therapy, or HAART.[56] This has been highly beneficial to many HIV-infected individuals since its introduction in 1996 when the protease inhibitor-based HAART initially became available.[57] Current optimal HAART options consist of combinations (or "cocktails") consisting of at least three drugs belonging to at least two types, or "classes," of antiretroviral agents. Typical regimens consist of two nucleoside analogue reverse transcriptase inhibitors (NARTIs or NRTIs) plus either a protease inhibitor or a non-nucleoside reverse transcriptase inhibitor (NNRTI). Because HIV disease progression in children is more rapid than in adults, and laboratory parameters are less predictive of risk for disease progression, particularly for young infants, treatment recommendations are more aggressive for children than for adults.[58] In developed countries where HAART is available, doctors assess the viral load, rapidity in CD4 decline, and patient readiness while deciding when to recommend initiating treatment.[59]
HAART allows the stabilization of the patient’s symptoms and viremia, but it neither cures the patient of HIV, nor alleviates the symptoms, and high levels of HIV-1, often HAART resistant, return once treatment is stopped.[60][61] Moreover, it would take more than the lifetime of an individual to be cleared of HIV infection using HAART.[62] Despite this, many HIV-infected individuals have experienced remarkable improvements in their general health and quality of life, which has led to the plummeting of HIV-associated morbidity and mortality.[63][64][65] In the absence of HAART, progression from HIV infection to AIDS occurs at a median of between nine to ten years and the median survival time after developing AIDS is only 9.2 months.[66] HAART is thought to increase survival time by between 4 and 12 years.[67][68] This average reflects the fact that for some patients – and in many clinical cohorts this may be more than fifty percent of patients – HAART achieves far less than optimal results. This is due to a variety of reasons such as medication intolerance/side effects, prior ineffective antiretroviral therapy and infection with a drug-resistant strain of HIV. However, non-adherence and non-persistence with antiretroviral therapy is the major reason most individuals fail to get any benefit from and develop resistance to HAART.[69] The reasons for non-adherence and non-persistence with HAART are varied and overlapping. Major psychosocial issues, such as poor access to medical care, inadequate social supports, psychiatric disease and drug abuse contribute to non-adherence. The complexity of these HAART regimens, whether due to pill number, dosing frequency, meal restrictions or other issues, along with side effects that create intentional non-adherence, also has a weighty impact.[70][71][72] The side effects include lipodystrophy, dyslipidaemia, insulin resistance, an increase in cardiovascular risks and birth defects.[73][74]
Daily multivitamin and mineral supplements have been found to reduce HIV disease progression among men and women. This could become an important low-cost intervention provided during early HIV disease to prolong the time before antiretroviral therapy is required.[75] Some individual nutrients have also been tried.[76][77] Anti-retroviral drugs are expensive, and the majority of the world's infected individuals do not have access to medications and treatments for HIV and AIDS.[78] It has been postulated that only a vaccine can halt the pandemic because a vaccine would possibly cost less, thus being affordable for developing countries, and would not require daily treatments.[78] However, after over 20 years of research, HIV-1 remains a difficult target for a vaccine.[78]
Research to improve current treatments includes decreasing side effects of current drugs, further simplifying drug regimens to improve adherence, and determining the best sequence of regimens to manage drug resistance. A number of studies have shown that measures to prevent opportunistic infections can be beneficial when treating patients with HIV infection or AIDS. Vaccination against hepatitis A and B is advised for patients who are not infected with these viruses and are at risk of becoming infected.[79] Patients with substantial immunosuppression are also advised to receive prophylactic therapy for Pneumocystis jiroveci pneumonia (PCP), and many patients may benefit from prophylactic therapy for toxoplasmosis and Cryptococcus meningitis as well.[55]
Various forms of alternative medicine have been used to treat symptoms or alter the course of the disease.[80] In the first decade of the epidemic when no useful conventional treatment was available, a large number of people with AIDS experimented with alternative therapies. The definition of "alternative therapies" in AIDS has changed since that time. Then, the phrase often referred to community-driven treatments, untested by government or pharmaceutical company research, that some hoped would directly suppress the virus or stimulate immunity against it. Examples of alternative medicine that people hoped would improve their symptoms or their quality of life include massage, stress management, herbal and flower remedies such as boxwood,[81][82] and acupuncture;[80] when used with conventional treatment, many now refer to these as "complementary" approaches. Despite the widespread use of complementary and alternative medicine by people living with HIV/AIDS, the effectiveness of these therapies has not been established.[83]
Prognosis
Without treatment, the net median survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype,[53] and the median survival rate after diagnosis of AIDS in resource-limited settings where treatment is not available ranges between 6 and 19 months, depending on the study.[84] In areas where it is widely available, the development of HAART as effective therapy for HIV infection and AIDS reduced the death rate from this disease by 80%, and raised the life expectancy for a newly-diagnosed HIV-infected person to about 20 years.[85]
Economic impact
HIV and AIDS retard economic growth by destroying human capital.[86] Without proper nutrition, health care and medicine that is available in developed countries, large numbers of people are falling victim to AIDS. They will not only be unable to work, but will also require significant medical care. The forecast is that this will likely cause a collapse of economies and societies in the region. In some heavily infected areas, the epidemic has left behind many orphans cared for by elderly grandparents.[87]
The increased mortality in this region will result in a smaller skilled population and labor force.[87] This smaller labor force will be predominantly young people, with reduced knowledge and work experience leading to reduced productivity. An increase in workers’ time off to look after sick family members or for sick leave will also lower productivity. Increased mortality will also weaken the mechanisms that generate human capital and investment in people, through loss of income and the death of parents.[87] By killing off mainly young adults, AIDS seriously weakens the taxable population, reducing the resources available for public expenditures such as education and health services not related to AIDS resulting in increasing pressure for the state's finances and slower growth of the economy. This results in a slower growth of the tax base, an effect that will be reinforced if there are growing expenditures on treating the sick, training (to replace sick workers), sick pay and caring for AIDS orphans. This is especially true if the sharp increase in adult mortality shifts the responsibility and blame from the family to the government in caring for these orphans.[87]
On the level of the household, AIDS results in both the loss of income and increased spending on healthcare by the household. The income effects of this lead to spending reduction as well as a substitution effect away from education and towards healthcare and funeral spending. A study in Côte d'Ivoire showed that households with an HIV/AIDS patient spent twice as much on medical expenses as other households.[88]
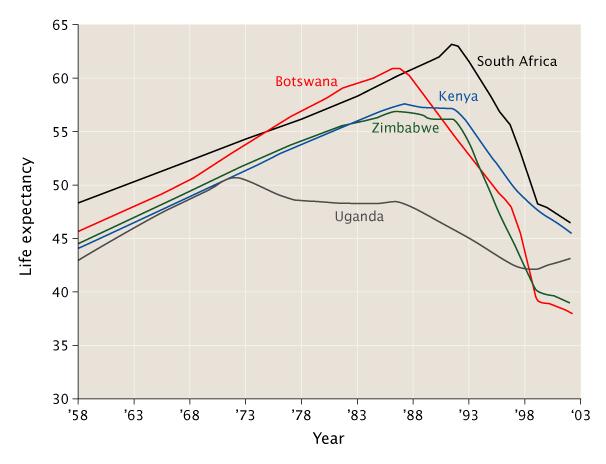
UNAIDS, WHO and the United Nations Development Programme have documented a correlation between the decreasing life expectancies and the lowering of gross national product in many African countries with prevalence rates of 10% or more. Indeed, since 1992 predictions that AIDS would slow economic growth in these countries have been published. The degree of impact depended on assumptions about the extent to which illness would be funded by savings and who would be infected.[88] Conclusions reached from models of the growth trajectories of 30 sub-Saharan economies over the period 1990–2025 were that the economic growth rates of these countries would be between 0.56 and 1.47% lower. The impact on gross domestic product (GDP) per capita was less conclusive. However, in 2000, the rate of growth of Africa's per capita GDP was in fact reduced by 0.7% per year from 1990–1997 with a further 0.3% per year lower in countries also affected by malaria.[89] The forecast now is that the growth of GDP for these countries will undergo a further reduction of between 0.5 and 2.6% per annum.[87] However, these estimates may be an underestimate, as they do not look at the effects on output per capita.[86]
Many governments in sub-Saharan Africa denied that there was a problem for years, and are only now starting to work towards solutions. Underfunding is a problem in all areas of HIV prevention when compared to even conservative estimates of the problems.
Recent research by the Overseas Development Institute (ODI) has suggested that the private sector has begun to recognize the impact of HIV/AIDS on the bottom line, both directly and indirectly. It is estimated that a company can generate an average return of US$3 for every US$1 invested in employee health due to a reduced absenteeism, better productivity and reduction in employee turnover.[90] Indirectly there are also important implications on the supply chain. Many multi-national corporations (MNCs) have therefore gotten involved in HIV/AIDS initiatives of three main types: a community-based partnerships, supply chain support, and sector-based initiatives.[91]
The launching of the world's first official HIV/AIDS Toolkit in Zimbabwe on October 3 2006 is a product of collaborative work between the International Federation of Red Cross and Red Crescent Societies, World Health Organization and the Southern Africa HIV/AIDS Information Dissemination Service. It is for the strengthening of people living with HIV/AIDS and nurses by minimal external support. The package, which is in form of eight modules focusing on basic facts about HIV and AIDS, was pre-tested in Zimbabwe in March 2006 to determine its adaptability. It disposes, among other things, categorized guidelines on clinical management, education and counseling of AIDS victims at community level.[92]
The Copenhagen Consensus is a project that seeks to establish priorities for advancing global welfare using methodologies based on the theory of welfare economics. The participants are all economists, with the focus of the project being a rational prioritization based on economic analysis. The project is based on the contention that, in spite of the billions of dollars spent on global challenges by the United Nations, the governments of wealthy nations, foundations, charities, and non-governmental organizations, the money spent on problems such as malnutrition and climate change is not sufficient to meet many internationally-agreed targets. The highest priority was assigned to implementing new measures to prevent the spread of HIV and AIDS. The economists estimated that an investment of $27 billion could avert nearly 30 million new infections by 2010.[93]
Stigma
AIDS stigma exists around the world in a variety of ways, including ostracism, rejection, discrimination and avoidance of HIV infected people; compulsory HIV testing without prior consent or protection of confidentiality; violence against HIV infected individuals or people who are perceived to be infected with HIV; and the quarantine of HIV infected individuals.[94] Stigma-related violence or the fear of violence prevents many people from seeking HIV testing, returning for their results, or securing treatment, possibly turning what could be a manageable chronic illness into a death sentence and perpetuating the spread of HIV.[95]
AIDS stigma has been further divided into the following three categories:
- Instrumental AIDS stigma—a reflection of the fear and apprehension that are likely to be associated with any deadly and transmissible illness.[96]
- Symbolic AIDS stigma—the use of HIV/AIDS to express attitudes toward the social groups or lifestyles perceived to be associated with the disease.[96]
- Courtesy AIDS stigma—stigmatization of people connected to the issue of HIV/AIDS or HIV- positive people.[97]
Often, AIDS stigma is expressed in conjunction with one or more other stigmas, particularly those associated with homosexuality, bisexuality, promiscuity, and intravenous drug use.
In many developed countries, there is an association between AIDS and homosexuality or bisexuality, and this association is correlated with higher levels of sexual prejudice such as anti-homosexual attitudes.[98] There is also a perceived association between AIDS and all male-male sexual behavior, including sex between uninfected men.[96]
Prevention
The diverse transmission routes of HIV are well-known and established. Also well-known is how to prevent transmission of HIV. However, recent epidemiological and behavioral studies in Europe and North America have suggested that a substantial minority of young people continue to engage in high-risk practices and that despite HIV/AIDS knowledge, young people underestimate their own risk of becoming infected with HIV (Dias et al., 2005). However, transmission of HIV between intravenous drug users has clearly decreased and HIV transmission by blood transfusion has become almost obsolete in this population.
Prevention of sexual transmission of HIV
Underlying science
- Unprotected receptive sexual acts are at more risk than unprotected insertive sexual acts, with the risk for transmitting HIV from an infected partner to an uninfected partner through unprotected insertive anal intercourse (UIAI) greater than the risk for transmission through receptive anal intercourse or oral sex. According to the French ministry for health, the probability of transmission per act varies from 0.03% to 0.07% for the case of receptive vaginal sex, from 0.02 to 0.05% in the case of insertive vaginal sex, from 0.01% to 0.185% in the case of insertive anal sex, and 0.5% to 3% in the case of receptive anal sex [1].
- Sexually-transmitted infections (STI) increase the risk of HIV transmission and infection because they cause the disruption of the normal epithelial barrier by genital ulceration and/or microulceration; and by accumulation of pools of HIV-susceptible or HIV-infected cells (lymphocytes and macrophages) in semen and vaginal secretions. Epidemiological studies from sub-Saharan Africa, Europe and North America have suggested that there is approximately, a four times greater risk of becoming HIV-infected in the presence of a genital ulcer such as caused by syphilis and/or chancroid; and a significant though lesser increased risk in the presence of STIs such as gonorrhoea, chlamydial infection and trichomoniasis which cause local accumulations of lymphocytes and macrophages (Laga et al., 1991).
- Transmission of HIV depends on the infectiousness of the index case and the susceptibility of the uninfected partner. Infectivity seems to vary during the course of illness and is not constant between individuals. An undetectable plasma viral load does not mean that you have a low viral load in the seminal liquid or genital secretions. Each 10 fold increment of seminal HIV RNA is associated with an 81% increased rate of HIV transmission (Tovanabutra et al., 2002).
- People who are infected with HIV can still be infected by other, more virulent strains.
- Oral sex is not without its risks as it has been established that HIV can be transmitted through both insertive and receptive oral sex (Rothenberg et al., 1998).
- Women are more susceptible to HIV-1 due to hormonal changes, vaginal microbial ecology and physiology, and a higher prevalence of sexually transmitted diseases (Sagar et al., 2004; Lavreys et al., 2004).
Prevention strategies
During a sexual act, only condoms, be they male or female, can reduce the chances of infection with HIV and other STIs and the chances of becoming pregnant. They must be used during all penetrative sexual intercourse with a partner who is HIV positive or whose status is unknown (Cayley, 2004). The effective use of condoms and screening of blood transfusion in North America, Western and Central Europe is credited with the low rates of AIDS in these regions. Adopting these effective prevention methods in other regions has proved controversial and difficult. Some claim this is in part because of the strong influence of the Roman Catholic Church, which opposes the use of condoms.
- The male latex condom is the single most efficient available technology to reduce the sexual transmission of HIV and other sexually transmitted infections. In order to be effective, they must be used correctly during each sexual act. Lubricants containing oil, such as petroleum jelly, or butter, must not be used as they weaken latex condoms and make them porous. If necessary, lubricants made from water are recommended. However, it is not recommended to use a lubricant for fellatio. Also, condoms have standards and expiration dates. It is essential to check the expiration date and if it conforms to European (EC 600) or American (D3492) standards before use.
- The female condom is an alternative to the male condom and is made from polyurethane, which allows it to be used in the presence of oil-based lubricants. They are larger than male condoms and have a stiffened ring-shaped opening, and are designed to be inserted into the vagina. The female condom also contains an inner ring which keeps the condom in place inside the vagina - inserting the female condom requires squeezing this ring.
With consistent and correct use of condoms, there is a very low risk of HIV infection. Studies on couples where one partner is infected show that with consistent condom use, HIV infection rates for the uninfected partner are below 1% per year
Government programs
The U.S. government and U.S. health organizations both endorse the ABC Approach to lower the risk of acquiring AIDS during sex:
- Abstinence or delay of sexual activity, especially for youth,
- Being faithful, especially for those in committed relationships,
- Condom use, for those who engage in risky behavior.
This approach has been very successful in Uganda, where HIV prevalence has decreased from 15% to 5%. However, the ABC approach is far from all that Uganda has done, as "Uganda has pioneered approaches towards reducing stigma, bringing discussion of sexual behavior out into the open, involving HIV-infected people in public education, persuading individuals and couples to be tested and counseled, improving the status of women, involving religious organizations, enlisting traditional healers, and much more." (Edward Green, Harvard medical anthropologist). Also, it must be noted that there is no conclusive proof that abstinence-only programs have been successful in any country in the world in reducing HIV transmission. This is why condom use is heavily co-promoted. There is also considerable overlap with the CNN Approach. This is:
- Condom use, for those who engage in risky behavior.
- Needles, use clean ones
- Negotiating skills; negotiating safer sex with a partner and empowering women to make smart choices
The ABC approach has been criticized, because a faithful partner of an unfaithful partner is at risk of AIDS [3]. Many think that the combination of the CNN approach with the ABC approach will be the optimum prevention platform.
Circumcision
Current research is clarifying the relationship between male circumcision and HIV in differing social and cultural contexts. UNAIDS believes that it is premature to recommend male circumcision services as part of HIV prevention programmes [4].
Moreover, South African medical experts are concerned that the repeated use of unsterilised blades in the ritual circumcision of adolescent boys may be spreading HIV.
Prevention of blood or blood product route of HIV transmission
Underlying science
- Sharing and reusing syringes contaminated with HIV-infected blood represents a major risk for infection with not only HIV but also hepatitis B and C. In the United States a third of all new HIV infections can be traced to needle sharing and almost 50% of long-term addicts have hepatitis C.
- The risk of being infected with HIV from a single prick with a needle that has been used on an HIV infected person though is thought to be about 1 in 150 (see table above). Post-exposure prophylaxis with anti-HIV drugs can further reduce that small risk.
- Universal precautions are frequently not followed in both sub-Saharan Africa and much of Asia because of both a shortage of supplies and inadequate training. The WHO estimates that approximately 2.5% of all HIV infections in sub-Saharan Africa are transmitted through unsafe healthcare injections.Because of this, the United Nations General Assembly, supported by universal medical opinion on the matter, has urged the nations of the world to implement universal precautions to prevent HIV transmission in health care settings.
Prevention strategies
- In those countries where improved donor selection and antibody tests have been introduced, the risk of transmitting HIV infection to blood transfusion recipients has been effectively eliminated. According to the WHO, the overwhelming majority of the world's population does not have access to safe blood and "between 5% and 10% of HIV infections worldwide are transmitted through the transfusion of infected blood and blood products."
- Medical workers who follow universal precautions or body substance isolation such as wearing latex gloves when giving injections and washing the hands frequently can help prevent infection of HIV.
- All AIDS-prevention organizations advise drug-users not to share needles and other material required to prepare and take drugs (including syringes, cotton balls, the spoons, water for diluting the drug, straws, crack pipes etc). It is important that people use new or properly sterilized needles for each injection. Information on cleaning needles using bleach is available from health care and addiction professionals and from needle exchanges. In the United States and other western countries, clean needles are available free in some cities, at needle exchanges or safe injection sites.
Mother to child transmission
Underlying science
- There is a 15–30% risk of transmission of HIV from mother to child during pregnancy, labour and delivery (Orendi et al., 1998). In developed countries the risk can of transmission of HIV from mother to child can be as low as 0-5%. A number of factors influence the risk of infection, particularly the viral load of the mother at birth (the higher the load, the higher the risk). Breastfeeding increases the risk of transmission by 10–15%. This risk depends on clinical factors and may vary according to the pattern and duration of breastfeeding.
Prevention strategies
- Studies have shown that antiretroviral drugs, cesarean delivery and formula feeding reduce the chance of transmission of HIV from mother to child (Sperling et al., 1996).
- When replacement feeding is acceptable, feasible, affordable, sustainable and safe, HIV-infected mothers are recommended to avoid breast feeding their infant. Otherwise, exclusive breastfeeding is recommended during the first months of life and should be discontinued as soon as possible.
References
http://en.wikipedia.org/wiki/Acquired_Immune_Deficiency_Syndrome#Prevention
References
- ↑ World Health Organization (1990). "Interim proposal for a WHO staging system for HIV infection and disease". WHO Wkly Epidem. Rec. 65 (29): 221&ndash, 228. PMID 1974812.
- ↑ Centers for Disease Control (CDC) (1982). "Persistent, generalized lymphadenopathy among homosexual males". MMWR Morb Mortal Wkly Rep. 31 (19): 249&ndash, 251. PMID 6808340.
- ↑ Barré-Sinoussi F, Chermann JC, Rey F; et al. (1983). "Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS)". Science. 220 (4599): 868–871. doi:10.1126/science.6189183. PMID 6189183.
- ↑ 4.0 4.1 Centers for Disease Control (CDC) (1982). "Opportunistic infections and Kaposi's sarcoma among Haitians in the United States". MMWR Morb Mortal Wkly Rep. 31 (26): 353&ndash, 354, 360&ndash, 361. PMID 6811853.
- ↑ Altman LK (1982-05-11). "New homosexual disorder worries officials". The New York Times.
- ↑ Kher U (1982-07-27). "A Name for the Plague". Time. Retrieved 2008-03-10.
- ↑ Centers for Disease Control (CDC) (1982). "Update on acquired immune deficiency syndrome (AIDS)—United States". MMWR Morb Mortal Wkly Rep. 31 (37): 507&ndash, 508, 513&ndash, 514. PMID 6815471.
- ↑ "1993 Revised Classification System for HIV Infection and Expanded Surveillance Case Definition for AIDS Among Adolescents and Adults". CDC. 1992. Retrieved 2006-02-09.
- ↑ 9.0 9.1 Kumaranayake L, Watts C (2001). "Resource allocation and priority setting of HIV/AIDS interventions: addressing the generalized epidemic in sub-Saharan Africa". J. Int. Dev. 13 (4): 451&ndash, 466. doi:10.1002/jid.798.
- ↑ Weber B (2006). "Screening of HIV infection: role of molecular and immunological assays". Expert Rev. Mol. Diagn. 6 (3): 399–411. doi:10.1586/14737159.6.3.399. PMID 16706742.
- ↑ Tóth FD, Bácsi A, Beck Z, Szabó J (2001). "Vertical transmission of human immunodeficiency virus". Acta Microbiol Immunol Hung. 48 (3–4): 413–27. PMID 11791341.
- ↑ Smith DK, Grohskopf LA, Black RJ; et al. (2005). "Antiretroviral Postexposure Prophylaxis After Sexual, Injection-Drug Use, or Other Nonoccupational Exposure to HIV in the United States". MMWR. 54 (RR02): 1&ndash, 20.
- ↑ Donegan E, Stuart M, Niland JC; et al. (1990). "Infection with human immunodeficiency virus type 1 (HIV-1) among recipients of antibody-positive blood donations". Ann. Intern. Med. 113 (10): 733&ndash, 739. PMID 2240875.
- ↑ 14.0 14.1 Coovadia H (2004). "Antiretroviral agents—how best to protect infants from HIV and save their mothers from AIDS". N. Engl. J. Med. 351 (3): 289&ndash, 292. PMID 15247337.
- ↑ Kaplan EH, Heimer R (1995). "HIV incidence among New Haven needle exchange participants: updated estimates from syringe tracking and testing data". J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 10 (2): 175&ndash, 176. PMID 7552482.
- ↑ Bell DM (1997). "Occupational risk of human immunodeficiency virus infection in healthcare workers: an overview". Am. J. Med. 102 (5B): 9&ndash, 15. PMID 9845490.
- ↑ 17.0 17.1 17.2 17.3 European Study Group on Heterosexual Transmission of HIV (1992). "Comparison of female to male and male to female transmission of HIV in 563 stable couples". BMJ. 304 (6830): 809&ndash, 813. PMID 1392708.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 Varghese B, Maher JE, Peterman TA, Branson BM,Steketee RW (2002). "Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use". Sex. Transm. Dis. 29 (1): 38&ndash, 43. PMID 11773877.
- ↑ Leynaert B, Downs AM, de Vincenzi I (1998). "Heterosexual transmission of human immunodeficiency virus: variability of infectivity throughout the course of infection. European Study Group on Heterosexual Transmission of HIV". Am. J. Epidemiol. 148 (1): 88&ndash, 96. PMID 9663408.
- ↑ "Facts about AIDS & HIV". avert.org. Retrieved 2007-11-30.
- ↑ Johnson AM, Laga M (1988). "Heterosexual transmission of HIV". AIDS. 2 (suppl. 1): S49–S56. PMID 3130121.
- ↑ N'Galy B, Ryder RW (1988). "Epidemiology of HIV infection in Africa". Journal of Acquired Immune Deficiency Syndromes. 1 (6): 551–558. PMID 3225742.
- ↑ Deschamps MM, Pape JW, Hafner A, Johnson WD Jr. (1996). "Heterosexual transmission of HIV in Haiti". Annals of Internal Medicine. 125 (4): 324&ndash, 330. PMID 8678397.
- ↑ Rothenberg RB, Scarlett M, del Rio C, Reznik D, O'Daniels C (1998). "Oral transmission of HIV". AIDS. 12 (16): 2095&ndash, 2105. PMID 9833850.
- ↑ Mastro TD, de Vincenzi I (1996). "Probabilities of sexual HIV-1 transmission". AIDS. 10 (Suppl A): S75&ndash, S82. PMID 8883613.
- ↑ "WHO Multi-country Study on Women's Health and Domestic Violence against Women". World Health Organization. 2006. Retrieved 2006-12-14.
- ↑ Koenig MA, Zablotska I, Lutalo T, Nalugoda F, Wagman J, Gray R (2004). "Coerced first intercourse and reproductive health among adolescent women in Rakai, Uganda". Int Fam Plan Perspect. 30 (4): 156–63. doi:10.1363/ifpp.30.156.04. PMID 15590381.
- ↑ 28.0 28.1 Laga M, Nzila N, Goeman J (1991). "The interrelationship of sexually transmitted diseases and HIV infection: implications for the control of both epidemics in Africa". AIDS. 5 (Suppl 1): S55&ndash, S63. PMID 1669925.
- ↑ Tovanabutra S, Robison V, Wongtrakul J; et al. (2002). "Male viral load and heterosexual transmission of HIV-1 subtype E in northern Thailand". J. Acquir. Immune. Defic. Syndr. 29 (3): 275&ndash, 283. PMID 11873077.
- ↑ Sagar M, Lavreys L, Baeten JM; et al. (2004). "Identification of modifiable factors that affect the genetic diversity of the transmitted HIV-1 population". AIDS. 18 (4): 615&ndash, 619. PMID 15090766.
- ↑ Lavreys L, Baeten JM, Martin HL Jr; et al. (2004). "Hormonal contraception and risk of HIV-1 acquisition: results of a 10-year prospective study". AIDS. 18 (4): 695&ndash, 697. PMID 15090778.
- ↑ Cayley WE Jr. (2004). "Effectiveness of condoms in reducing heterosexual transmission of HIV". Am. Fam. Physician. 70 (7): 1268&ndash, 1269. PMID 15508535.
- ↑ Catholic Church (1997). "Offenses against chastity". Catechism of the Catholic Church : Second Edition. Vatican: Amministrazione Del Patrimonio Della Sede Apostolica. p. 2353. Retrieved 2006-06-14.
- ↑ Human Rights Watch (2005). "Restrictions on Condoms". The Less They Know, the Better. New York NY: Human Rights Watch.
- ↑ "Ignorance only: HIV/AIDS, Human rights and federally funded abstinence-only programs in the United States. Texas: A case study". Human Rights Watch. 2002-09-02. Retrieved 2006-03-28.
- ↑ Hauser, Debra (2004). "Five Years of Abstinence-Only-Until-Marriage Education: Assessing the Impact" (PDF). Advocates for Youth. Retrieved 2006-06-07.
- ↑ "Module 5/Guidelines for Educators" (Microsoft Word). Durex. Retrieved 2006-04-17.
- ↑ PATH (2006). "The female condom: significant potential for STI and pregnancy prevention". Outlook. 22 (2).
- ↑ "Condom Facts and Figures". WHO. August 2003. Retrieved 2006-01-17.
- ↑ "Adult Male Circumcision Significantly Reduces Risk of Acquiring HIV: Trials Kenya and Uganda Stopped Early". NIAID. 2006-12-13. Retrieved 2006-12-15.
- ↑ "Repeated Use of Unsterilized Blades in Ritual Circumcision Might Contribute to HIV Spread in S. Africa, Doctors Say". Kaisernetwork.org. 2005. Retrieved 2006-03-28.
- ↑ Dias SF, Matos MG, Goncalves, A. C. (2005). "Preventing HIV transmission in adolescents: an analysis of the Portuguese data from the Health Behaviour School-aged Children study and focus groups". Eur. J. Public Health. 15 (3): 300&ndash, 304. PMID 15941747.
- ↑ 44.0 44.1 Fan H (2005). Fan, H., Conner, R. F. and Villarreal, L. P. eds, ed. AIDS: science and society (4th ed.). Boston, MA: Jones and Bartlett Publishers. ISBN 0-7637-0086-X.
- ↑ "WHO, UNAIDS Reaffirm HIV as a Sexually Transmitted Disease". WHO. 2003-03-17. Retrieved 2006-01-17.
- ↑ "HIV Transmission in the Medical Setting: A White Paper by Physicians for Human Rights". Partners in Health. Physicians for Human Rights. 2003-03-13. Retrieved 2006-03-01.
- ↑ Drugtext.org
- ↑ "Blood safety....for too few". WHO. 2001. Retrieved 2006-01-17.
- ↑ 49.0 49.1 Coovadia HM, Bland RM (2007). "Preserving breastfeeding practice through the HIV pandemic". Trop. Med. Int. Health. 12 (9): 1116&ndash, 1133. PMID 17714431.
- ↑ Sperling RS, Shapirom DE, Coombsm RW; et al. (1996). "Maternal viral load, zidovudine treatment, and the risk of transmission of human immunodeficiency virus type 1 from mother to infant". N. Engl. J. Med. 335 (22): 1621&ndash, 1629. PMID 8965861.
- ↑ WHO HIV and Infant Feeding Technical Consultation (2006). "Consensus statement" (PDF). Retrieved 2008-03-12.
- ↑ Berry S (2006-06-08). "Children, HIV and AIDS". avert.org. Retrieved 2006-06-15.
- ↑ 53.0 53.1
- ↑ "Fact Sheet: Mother-to-child transmission of HIV". United Nations. 2001. Retrieved 2006-03-10.
- ↑ 55.0 55.1 "A Pocket Guide to Adult HIV/AIDS Treatment February 2006 edition". Department of Health and Human Services. February 2006. Retrieved 2006-09-01.
- ↑ "A Pocket Guide to Adult HIV/AIDS Treatment February 2006 edition". Department of Health and Human Services. February 2006. Retrieved 2006-09-01.
- ↑
- ↑ "Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection" (PDF). Department of Health and Human Services Working Group on Antiretroviral Therapy and Medical Management of HIV-Infected Children. 2005-11-03. Retrieved 2006-01-17.
- ↑ "Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents" (PDF). Department of Health and Human Services Panel on Clinical Practices for Treatment of HIV Infection. 2005-10-06. Retrieved 2006-01-17.
- ↑ Martinez-Picado J, DePasquale MP, Kartsonis N; et al. (2000). "Antiretroviral resistance during successful therapy of human immunodeficiency virus type 1 infection". Proc. Natl. Acad. Sci. U. S. A. 97 (20): 10948&ndash, 10953. PMID 11005867.
- ↑ Dybul M, Fauci AS, Bartlett JG, Kaplan JE, Pau AK; Panel on Clinical Practices for Treatment of HIV. (2002). "Guidelines for using antiretroviral agents among HIV-infected adults and adolescents". Ann. Intern. Med. 137 (5 Pt 2): 381&ndash, 433. PMID 12617573.
- ↑ Blankson JN, Persaud D, Siliciano RF (2002). "The challenge of viral reservoirs in HIV-1 infection". Annu. Rev. Med. 53: 557&ndash, 593. PMID 11818490.
- ↑ Palella FJ, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, Aschman DJ, Holmberg SD (1998). "Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection". N. Engl. J. Med. 338 (13): 853&ndash, 860. PMID 9516219.
- ↑ Wood E, Hogg RS, Yip B, Harrigan PR, O'Shaughnessy MV, Montaner JS (2003). "Is there a baseline CD4 cell count that precludes a survival response to modern antiretroviral therapy?". AIDS. 17 (5): 711&ndash, 720. PMID 12646794.
- ↑ Chene G, Sterne JA, May M, Costagliola D, Ledergerber B, Phillips AN, Dabis F, Lundgren J, D'Arminio Monforte A, de Wolf F, Hogg R, Reiss P, Justice A, Leport C, Staszewski S, Gill J, Fatkenheuer G, Egger ME and the Antiretroviral Therapy Cohort Collaboration (2003). "Prognostic importance of initial response in HIV-1 infected patients starting potent antiretroviral therapy: analysis of prospective studies". Lancet. 362 (9385): 679&ndash, 686. doi:10.1016/S0140-6736(03)14229-8. PMID 12957089.
- ↑
- ↑ King JT, Justice AC, Roberts MS, Chang CH, Fusco JS and the CHORUS Program Team (2003). "Long-Term HIV/AIDS Survival Estimation in the Highly Active Antiretroviral Therapy Era". Medical Decision Making. 23 (1): 9&ndash, 20. PMID 12583451.
- ↑ Tassie JM, Grabar S, Lancar R, Deloumeaux J, Bentata M, Costagliola D and the Clinical Epidemiology Group from the French Hospital Database on HIV (2002). "Time to AIDS from 1992 to 1999 in HIV-1-infected subjects with known date of infection". Journal of acquired immune deficiency syndromes. 30 (1): 81&ndash, 7. PMID 12048367.
- ↑ Becker SL, Dezii CM, Burtcel B, Kawabata H, Hodder S. (2002). "Young HIV-infected adults are at greater risk for medication nonadherence". MedGenMed. 4 (3): 21. PMID 12466764.
- ↑ Nieuwkerk P, Sprangers M, Burger D, Hoetelmans RM, Hugen PW, Danner SA, van Der Ende ME, Schneider MM, Schrey G, Meenhorst PL, Sprenger HG, Kauffmann RH, Jambroes M, Chesney MA, de Wolf F, Lange JM and the ATHENA Project (2001). "Limited Patient Adherence to Highly Active Antiretroviral Therapy for HIV-1 Infection in an Observational Cohort Study". Arch. Intern. Med. 161 (16): 1962&ndash, 1968. PMID 11525698.
- ↑ Kleeberger C, Phair J, Strathdee S, Detels R, Kingsley L, Jacobson LP (2001). "Determinants of Heterogeneous Adherence to HIV-Antiretroviral Therapies in the Multicenter AIDS Cohort Study". J. Acquir. Immune Defic. Syndr. 26 (1): 82&ndash, 92. PMID 11176272.
- ↑ Heath KV, Singer J, O'Shaughnessy MV, Montaner JS, Hogg RS (2002). "Intentional Nonadherence Due to Adverse Symptoms Associated With Antiretroviral Therapy". J. Acquir. Immune Defic. Syndr. 31 (2): 211&ndash, 217. PMID 12394800.
- ↑ Montessori V, Press N, Harris M, Akagi L, Montaner JS (2004). "Adverse effects of antiretroviral therapy for HIV infection". CMAJ. 170 (2): 229&ndash, 238. PMID 14734438.
- ↑ Saitoh A, Hull AD, Franklin P, Spector SA (2005). "Myelomeningocele in an infant with intrauterine exposure to efavirenz". J. Perinatol. 25 (8): 555&ndash, 556. doi:10.1038/sj.jp.7211343. PMID 16047034.
- ↑ Fawzi W, Msamanga G, Spiegelman D, Hunter DJ (2005). "Studies of vitamins and minerals and HIV transmission and disease progression". J. Nutrition. 135 (4): 938&ndash, 944. PMID 15795466.
- ↑ (Selenium:) Hurwitz BE, Klaus JR, Llabre MM, Gonzalez A, Lawrence PJ, Maher KJ, Greeson JM, Baum MK, Shor-Posner G, Skyler JS, Schneiderman N (2007). "Suppression of human immunodeficiency virus type 1 viral load with selenium supplementation: a randomized controlled trial". Arch Intern Med. 167 (2): 148&ndash, 155. PMID 17242315.
- ↑ (Vitamin C:) Cathcart RR (1984). "Vitamin C in the Treatment of Acquired Immune Deficiency Syndrome". Medical Hypotheses. 14 (4): 423–433. doi:10.1016/0306-9877(84)90149-X. PMID 6238227.
- ↑ 78.0 78.1 78.2 Ferrantelli F, Cafaro A, Ensoli B (2004). "Nonstructural HIV proteins as targets for prophylactic or therapeutic vaccines". Curr Opin Biotechnol. 15 (6): 543&ndash, 556. PMID 15560981.
- ↑ Laurence J (2006). "Hepatitis A and B virus immunization in HIV-infected persons". AIDS Reader. 16 (1): 15&ndash, 17. PMID 16433468.
- ↑ 80.0 80.1 Saltmarsh S (2005). "Voodoo or valid? Alternative therapies benefit those living with HIV". Positively Aware. 3 (16): 46. PMID 16479668.
- ↑ Pharo A; et al. (1996). "Evaluation of the safety and efficacy of SPV-30 (boxwood extract) in patients with HIV disease". Int Conf AIDS (Jul 7–12): 11:19. abstract no. Mo. B.180.
- ↑ Durant J; et al. (1998). "Efficacy and safety of Buxussempervirens L. preparations (SPV-30) in HIV infected asymptomatic patients: a multi-centre, randomized, double-blind, placebo-controlled trial". Phytomedicine (5): 1–10.
- ↑ Mills E, Wu P, Ernst E (2005). "Complementary therapies for the treatment of HIV: in search of the evidence". Int. J. STD AIDS. 16 (6): 395&ndash, 403. PMID 15969772.
- ↑ Template:Cite paper
- ↑ Knoll B, Lassmann B, Temesgen Z (2007). "Current status of HIV infection: a review for non-HIV-treating physicians". Int J Dermatol. 46 (12): 1219–28. doi:10.1111/j.1365-4632.2007.03520.x. PMID 18173512.
- ↑ 86.0 86.1 Template:Cite paper
- ↑ 87.0 87.1 87.2 87.3 87.4 Greener R (2002). "AIDS and macroeconomic impact". In S, Forsyth (ed.). State of The Art: AIDS and Economics. IAEN. pp. 49&ndash, 55.
- ↑ 88.0 88.1 Over M (1992). "The macroeconomic impact of AIDS in Sub-Saharan Africa, Population and Human Resources Department". The World Bank.
- ↑ Bonnel R (2000). "HIV/AIDS and Economic Growth: A Global Perspective". S. A. J. Economics. 68 (5): 820&ndash, 855.
- ↑ Goetzel RZ, Ozminkowski RJ, Baase CM, Billotti GM (2005). "Estimating the return-on-investment from changes in employee health risks on the Dow Chemical Company's health care costs". Journal of Occupational and Environmental Medicine. 47: 759–68. PMID 16093925.
- ↑ "AIDS and the private sector: The case of South Africa" (PDF). Overseas Development Institute. 2007. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help) - ↑ Mu Xuequan (2006). "Zimbabwe launches world's first AIDS training package". xinhua. Retrieved 2006-10-03.
- ↑ "$27 Billion Boost for HIV Prevention Programs Could Avert Majority of Projected HIV Infections Worldwide". kaisernetwork.org. 2002. Retrieved 2008-03-10.
- ↑ "The impact of AIDS on people and societies" (PDF). 2006 Report on the global AIDS epidemic (PDF)
|format=requires|url=(help). UNAIDS. 2006. Retrieved 2006-06-14. - ↑ Ogden J, Nyblade L (2005). "Common at its core: HIV-related stigma across contexts" (PDF). International Center for Research on Women. Retrieved 2007-02-15.
- ↑ 96.0 96.1 96.2 Herek GM, Capitanio JP (1999). "AIDS Stigma and sexual prejudice" (PDF). American Behavioral Scientist. 42 (7): 1130–1147. doi:10.1177/0002764299042007006. Retrieved 2006-03-27.
- ↑ Snyder M, Omoto AM, Crain AL (1999). "Punished for their good deeds: stigmatization for AIDS volunteers". American Behavioral Scientist. 42 (7): 1175&ndash, 1192. doi:10.1177/0002764299042007009.
- ↑ Herek GM, Capitanio JP, Widaman KF (2002). "HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999" (PDF). Am J Public Health. 92 (3): 371–7. PMID 11867313. Retrieved 2008-03-10.
Further reading
- "2007 AIDS epidemic update" (pdf). UNAIDS. Retrieved 2008-03-21.
- "UNAIDS Annual Report - Making the money work" (pdf). UNAIDS. Retrieved 2008-03-21.
- "Financial Resources Required to Achieve, Universal Access to HIV Prevention, Treatment Care and Support" (pdf). UNAIDS. Retrieved 2008-03-21.
- "Practical Guidelines for Intensifying HIV Prevention" (pdf). UNAIDS. Retrieved 2008-03-21.
- "Antiretroviral Formulations" (pdf). US Department of Health and Human Services. Retrieved 2008-03-21.
- "Approved Medications to Treat HIV Infection" (pdf). US Department of Health and Human Services. Retrieved 2008-03-21.
- "The HIV Life Cycle" (pdf). US Department of Health and Human Services. Retrieved 2008-03-21.
External links
- Template:Dmoz
- "AIDSinfo - HIV/AIDS Treatment Information". US Department of Health and Human Services. Retrieved 2008-03-21.
- "UNAIDS: The Joint United Nations Programme on HIV/AIDS". UNAIDS. Retrieved 2008-03-21.
|
AIDS Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
HIV AIDS On the Web |
|
American Roentgen Ray Society Images of HIV AIDS |
Template:Viral diseases Template:STD/STI
Template:Link FA Template:Link FA af:Vigs als:AIDS am:ኤድስ an:SIDA ar:متلازمة العوز المناعي المكتسب ast:SIDA az:QİÇS bat-smg:AIDS be-x-old:СНІД bg:Синдром на придобитата имунна недостатъчност bm:Sida bn:এইডস bs:Sida ca:SIDA cs:AIDS da:Aids de:Aids dv:އެއިޑްސް ބަލި el:AIDS eo:Aidoso et:AIDS eu:Hartutako Immuno Eskasiaren Sindromea fa:ایدز fi:AIDS fur:AIDS ga:SEIF gd:AIDS gl:SIDA gu:એડ્સ he:איידס hi:एड्स hr:Sindrom stečene imunodeficijencije ht:Sida hu:AIDS hy:ՁԻԱՀ id:AIDS is:Alnæmi it:AIDS ka:შიდსი ki:AIDS km:ជំងឺអេដស៍ kn:ಏಡ್ಸ್ ರೋಗ ko:에이즈 ku:AIDS la:SCDI lb:Aids ln:Sida lo:ເອດສ໌ lt:AIDS lv:AIDS mk:СИДА ml:എയ്ഡ്സ് mn:Дархлалын олдмол хомсдол mr:एड्स ms:AIDS mt:AIDS new:एड्स nl:Aids nn:Hiv/aids no:Aids oc:SIDA ps:اېډز qu:Unquy hark'aypa chaskisqa waqlliynin scn:AIDS sh:AIDS si:ඒඩ්ස් simple:AIDS sk:Aids sl:Aids sr:Сида sv:Aids sw:Ukimwi ta:எய்ட்ஸ் te:ఎయిడ్స్ tg:СПИД th:เอดส์ tt:AİDS uk:СНІД ur:محصولی کسرمناعی متلازمہ uz:Orttirilgan Imunitet Tanqisligi Sindromi vec:AIDS yi:עידס yo:AIDS zh-min-nan:AIDS zh-yue:愛滋病
- Pages with reference errors
- Pages using duplicate arguments in template calls
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- CS1 maint: Multiple names: editors list
- CS1 maint: Extra text: editors list
- Pages with citations using unsupported parameters
- Pages using citations with format and no URL
- HIV/AIDS
- LGBT-related navigation templates
- Immune system disorders
- Infectious disease
- Viral diseases
- Pandemics
- Sexually transmitted infections
- Syndromes
- Virology
- AIDS origin hypotheses
- Medical disasters
- Acronyms
- Immunodeficiency
- Microbiology
- Overview complete