Glomerular disease: Difference between revisions
| Line 167: | Line 167: | ||
|- | |- | ||
| rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" + |Non-proliferative | | rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" + |Non-proliferative | ||
!Minimal change disease | ![[Minimal change disease]] | ||
| | | | ||
* Idiopathic | * [[Idiopathic]] | ||
* Protein tyrosine phosphatase receptor type O (glomerular epithelial protein 1- GLEPP1) | * [[Protein]] [[Protein tyrosine phosphatase|tyrosine phosphatase]] receptor type O (glomerular epithelial protein 1- GLEPP1) | ||
| | | | ||
* Young children | * Young children | ||
* Recent infection and immunization | * Recent [[infection]] and [[immunization]] | ||
* Atopy | * [[Atopy]] | ||
* Hodgkin lymphoma | * [[Hodgkin's lymphoma|Hodgkin lymphoma]] | ||
* Thrombosis (due to urinary loss of antithrombin-III) | * [[Thrombosis]] (due to [[Urinary system|urinary]] loss of [[Antithrombin III|antithrombin-III]]) | ||
| | | | ||
+ | + | ||
| Line 204: | Line 204: | ||
* Normal | * Normal | ||
| | | | ||
* Fusion of podocytes | * Fusion of [[podocytes]] | ||
| | | | ||
- | - | ||
|- | |- | ||
!Focal segmental glomerulosclerosis | ![[Focal segmental glomerulosclerosis]] | ||
| | | | ||
* Idiopathic | * Idiopathic | ||
* HIV | * [[Human Immunodeficiency Virus (HIV)|HIV]] | ||
* Heroine use | * [[Heroine hydrochloride|Heroine]] use | ||
* Sickle cell disease | * [[Sickle-cell disease|Sickle cell disease]] | ||
* Interferon | * [[Interferon]] | ||
* Severe obesity | * Severe [[obesity]] | ||
* Mixed | * [[Cryoglobulinemia|Mixed cryoglobulinemia]] ([[Hepatitis C]]) | ||
| | | | ||
* Adults | * Adults | ||
| Line 232: | Line 232: | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
* Focal (some glomeruli) and segmental (only part of glomerulus) | * Focal (some [[glomeruli]]) and segmental (only part of [[glomerulus]]) | ||
| | | | ||
* Effacement of podocytes | * Effacement of [[podocytes]] | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|- | |- | ||
!Membranous glomerulonephritis | ![[Membranous glomerulonephritis]] | ||
| | | | ||
* Idiopathic | * [[Idiopathic]] | ||
* Hepatitis B and C | * [[Hepatitis B]] and [[Hepatitis C|C]] | ||
* Solid tumors | * [[Solid tumors]] | ||
* Systemic lupus | * [[Systemic lupus erythematosus]] | ||
* Drugs (NSAIDS, | * Drugs ([[NSAIDS]], pencilamine, [[gold]], [[captopril]]) | ||
| | | | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 258: | Line 258: | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| | | | ||
* Thick glomerular basement | * Thick [[glomerular basement membrane]] | ||
| | | | ||
* Sub-epithelial immune complex depositis with 'spike and dome' appearance | * Sub-[[Epithelial cells|epithelial]] [[immune complex]] depositis with 'spike and dome' appearance | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|- | |- | ||
| rowspan="7" align="center" style="background:#4479BA; color: #FFFFFF;" + |Proliferative | | rowspan="7" align="center" style="background:#4479BA; color: #FFFFFF;" + |Proliferative | ||
!IgA nephropathy | ![[IgA nephropathy]] | ||
| | | | ||
* Idiopathic | * [[Idiopathic]] | ||
* Viral infections | * [[Viral infections]] | ||
| | | | ||
* Young children | * Young children | ||
* History of mucosal infections (e.g. gastroenteritis) and upper respiratory tract infection | * History of [[mucosal]] [[infections]] (e.g. [[gastroenteritis]]) and [[upper respiratory tract infection]] | ||
* 2-3 days after infection (synpharyngitic) | * 2-3 days after [[infection]] (synpharyngitic) | ||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 287: | Line 287: | ||
* Crescent formation | * Crescent formation | ||
| | | | ||
* Mesangial proliferation | * [[Mesangial cell|Mesangial]] proliferation | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|- | |- | ||
! rowspan="5" |Rapidly progressive glomerulonephritis | ! rowspan="5" |[[Rapidly progressive glomerulonephritis]] | ||
| | | | ||
* Goodpasture syndrome | * [[Goodpasture syndrome]] | ||
| | | | ||
* Young adults | * Young adults | ||
| Line 308: | Line 308: | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| | | | ||
* Hypercellular and inflamed glomeruli (Crescent formation) | * Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | ||
| | | | ||
* Diffuse thickening of the glomerular basement membrane with absence of | * Diffuse thickening of the [[glomerular basement membrane]] with absence of sub-[[Epithelial cells|epithelial]] and sub-[[endothelial]] deposits | ||
|<nowiki>+ (Linear)</nowiki> | |<nowiki>+ (Linear)</nowiki> | ||
|- | |- | ||
| | | | ||
* Post infectious glomerulonephritis | * [[Poststreptococcal glomerulonephritis|Post infectious glomerulonephritis]] | ||
| | | | ||
* Streptococcal skin infections | * [[Streptococcal infections|Streptococcal]] [[skin]] [[infections]] | ||
* Streptococcal pharyngitis | * [[Streptococcus|Streptococcal]] [[pharyngitis]] | ||
* 2-3 weeks after infection | * 2-3 weeks after [[infection]] | ||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 332: | Line 332: | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| | | | ||
* Hypercellular and inflamed glomeruli | * Hypercellular and [[inflamed]] [[glomeruli]] | ||
| | | | ||
* Sub-epithelial immune complex deposits | * Sub-[[epithelial]] [[immune complex]] deposits | ||
| + (Granular) | | + (Granular) | ||
|- | |- | ||
| | | | ||
* Granulomatosis with polyangitis (Wegner's granulomatosis) | * [[Granulomatosis with polyangiitis|Granulomatosis with polyangitis]] ([[Wegener's granulomatosis|Wegner's granulomatosis]]) | ||
| | | | ||
* Necrotizing granulomas (Nasopharynx, lungs, kidneys) | * [[Necrotizing]] [[granulomas]] ([[Nasopharynx]], [[lungs]], [[kidneys]]) | ||
* [[Conjunctivitis]] | * [[Conjunctivitis]] | ||
* Ulceration of the [[cornea]] | * Ulceration of the [[cornea]] | ||
* [[Episcleritis]] | * [[Episcleritis]] | ||
* Peripheral neuropathy | * [[Peripheral neuropathy]] | ||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 354: | Line 354: | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| | | + ([[C-ANCA]]) | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
* Hypercellular and inflamed glomeruli (Crescent formation) | * Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | ||
|<nowiki>- (pauci-immune)</nowiki> | |<nowiki>- (pauci-immune)</nowiki> | ||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|- | |- | ||
| | | | ||
* Churg Strauss syndrome | * [[Churg-Strauss syndrome|Churg Strauss syndrome]] | ||
| | | | ||
* Necrotizing granulomas (Lungs and kidneys) | * [[Necrotizing]] [[granulomas]] ([[Lungs]] and [[kidneys]]) | ||
* Asthma | * [[Asthma]] | ||
* Peripheral neuropathy | * [[Peripheral neuropathy]] | ||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 378: | Line 378: | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| | | | ||
+ (C-ANCA) | + ([[C-ANCA]]) | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
* Hypercellular and inflamed glomeruli (Crescent formation) | * Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | ||
|<nowiki>- (pauci-immune)</nowiki> | |<nowiki>- (pauci-immune)</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|- | |- | ||
| | | | ||
* Microscopic | * [[Microscopic polyangiitis]] | ||
| | | | ||
* Necrotizing vasculitis (no granuloma) | * [[Necrotizing]] [[vasculitis]] (no [[granuloma]]) | ||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 400: | Line 400: | ||
| + | | + | ||
| | | | ||
+ (P-ANCA) | + ([[P-ANCA]]) | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
* Hypercellular and inflamed glomeruli (Crescent formation) | * Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | ||
|<nowiki>- (pauci-immune)</nowiki> | |<nowiki>- (pauci-immune)</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|- | |- | ||
!Membranoproliferative glomerulonephritis | ![[Membranoproliferative glomerulonephritis]] | ||
| | | | ||
* Idiopathic | * [[Idiopathic]] | ||
* Hepatitis B and C (Type 1) | * [[Hepatitis B]] and [[Hepatitis C|C]] (Type 1) | ||
* C3 nepritic factor (Type2) | * C3 nepritic factor (Type2) | ||
| | | | ||
* | * [[Hematuria]] | ||
* Oliguria | * [[Oliguria]] | ||
* Periorbital edema | * [[Periorbital edema]] | ||
* Hypertension | * [[Hypertension]] | ||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| Line 431: | Line 431: | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| | | | ||
* Thick glomerular basement membrane (Tram-track appearance) | * Thick [[glomerular basement membrane]] (Tram-track appearance) | ||
| | | | ||
* Mesangial proliferation and leukocyte infiltration | * [[Mesangial cell|Mesangial]] proliferation and [[Leukocytes|leukocyte]] infiltration | ||
|<nowiki>+ (Granular)</nowiki> | |<nowiki>+ (Granular)</nowiki> | ||
|} | |} | ||
Revision as of 15:27, 2 May 2018
This page contains general information about Glomerular disease. For more information on specific types, please visit the pages on [[
| Glomerular disease | |
 | |
|---|---|
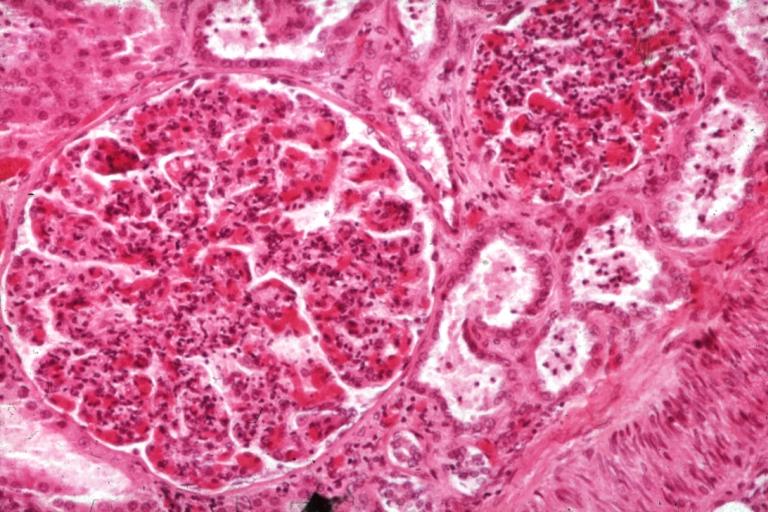
| Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2], Syed Hassan A. Kazmi BSc, MD [3]
Overview
Glomerular disease is a condition that affects the glomerulus. It consists of different diseases with different clinical courses and treatment options. Glomerular disease can be isolated hematuria, isolated proteinuria; acute or chronic glomerulonephritis, and nephrotic or nephritic features of glomerulonephritis. The end stage of all of these diseases will be glomerulosclerosi swhich is characterized by fibrosis of the glomerulus, and end-stage renal disease.
Classification
Glomerular diseases can be classified by their clinical symptoms as below:
Glomerular hematuria:
1- Glomerulonephritis
This disease is further categorized into two pathological patterns named non-proliferative or proliferative types. In each type the treatment options and the clinical outcome are different. These disease spectrum can be due to primary causes or secondary causes (discussed in each type in related chapter separately).
2- Isolated hematuria
For differential diagnosis and causes of isolated hematuria, click here.
Proteinuria:
1- Nephrotic syndrome
2- Isolated proteinuria
For differential diagnosis and causes of isolated proteinuria, click here.
Non Proliferative Glomerulonephritis
This is characterised by a lack of hypercellularity in the glomeruli. They usually cause nephrotic syndrome. This includes the following types:
1. Minimal change GN
This form of GN causes 80% of nephrotic syndrome in children, but only 20% in adults. As the name indicates, there are no changes visible on simple light microscopy, but on electron microscopy there is fusion of podocytes (supportive cells in the glomerulus). Immunohistochemistry staining is negative. Treatment consists of supportive care for the massive fluid accumulation in the patients body (= oedema) and as well as steroids to halt the disease process (e.g. Prednisone 1 mg/ kg). Over 90% of children respond well to steroids, being essentially cured after 3 months of treatment. Adults have a lower response rate (80%). Failure to respond to steroids ('steroid resistant') or return of the disease when steroids are stopped ('steroid dependent') may require cytotoxic therapy (e.g. cyclosporin) which is associated with many side-effects. As we all may know
2. Focal Segmental Glomerulosclerosis (FSGS)
FSGS may be primary or secondary to reflux nephropathy, Alport syndrome, heroin use or HIV. FSGS presents as a nephrotic syndrome with varying degrees of impaired renal function (seen as a rising serum creatinine, hypertension). As the name suggests, only certain foci of glomeruli within the kidney are affected, and then only a segment of an individual glomerulus.
The pathological lesion is sclerosis (fibrosis) within the glomerulus and hyalinisation of the feeding arterioles, but no increase in the number of cells (hence non proliferative). The hyaline is an amorphous material, pink, homogeneous, resulting from combination of plasma proteins, increased mesangial matrix and collagen. Staining for antibodies and complement is essentially negative. Steroids are often tried but not shown to be effective. 50% of people with FSGS continue to have progressive deterioration of kidney function, ending in renal failure.
3. Membranous glomerulonephritis
Presents as nephrotic syndrome, leading cause in adults (35%). It is usually idiopathic, but may be associated with cancers (lung, bowel), infection (hepatitis, malaria), drugs (penicillamine), SLE. The basement membrane on which the glomerular cells sit is thickened, but no increase in cells. Immune staining shows diffuse granular uptake of IgG (immunoglobulin G) and complement type 3. A third of people continue having the disease, 1/3 remit, 1/3 progress to end-stage kidney failure. As glomerulonephritis progresses (in any type), the tubules of the kidney (which are separate to the glomerulus) also become affected, showing atrophy and hyalinisation. The kidney grossly appears shrunken. Treatment with steroids is attempted if it is progressive.
Proliferative Glomerulonephritis
This type is characterised by increased number of cells in the glomerulus (hypercellular). Usually present as a nephritic syndrome and usually progress to end-stage renal failure (ESRF) over weeks to years (depending on type).
1. IgA disease (Berger's nephropathy)
This is the most common type of glomerulonephritis in adults world-wide. It usually presents as macroscopic haematuria (visibly bloody urine). It occasionally presents as a nephrotic syndrome. It often affects young males after an upper respiratory tract infection. Microscopic examination of biopsy specimens shows increased number of mesangial cells with increased matrix (the 'cement' which holds everything together). Immuno-staining is positive for immunoglobulin A deposits within the matrix. Prognosis is variable, 20% progress to ESRF. Steroids and immunosuppression are not effective treatments for this disease; ACE inhibitors are the mainstay of treatment.
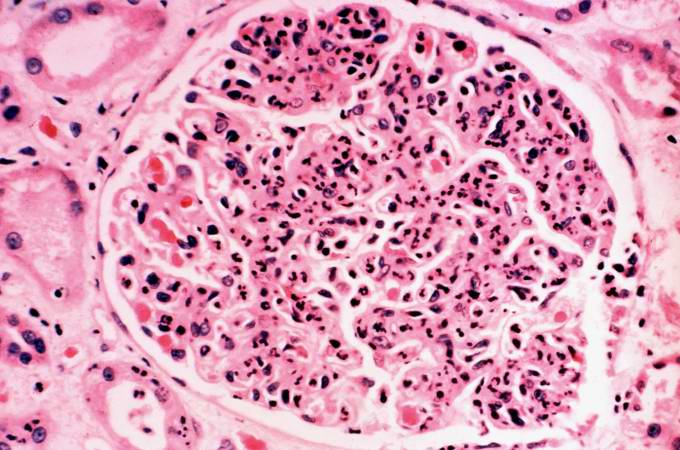
2. Post-infectious Glomerulonephritis
Post-infectious glomerulonephritis occurs after Streptococcal infection - usually of the skin, after a latency of 10 days. This condition is essentially defined as an inflammation of the kidneys. Light microscopy shows diffuse hypercellularity due to proliferation of endothelial and mesangial cells, inflammatory infiltrate with neutrophils and with monocytes. The Bowman space is reduced (compressed), in severe cases might see cresent formation [see later]. However, biopsy is seldom done because the disease usually regresses. Patients present with a nephritic syndrome. Diagnosis is suggested by positive streptococcal titers in the blood (ASOT). Treatment is supportive, and the disease resolves (as a rule) in 2 weeks.
3. Mesangiocapillary Glomerulonephritis
This is primary, or secondary to SLE, viral hepatitis, hypocomplementemia. One sees 'hypercellular and hyperlobular' glomeruli due to proliferation of both cells and the matrix within the mesangium. Presents usually with as a nephrotic syndrome but can be nephritic, with inevitable progression to ESRF.
4. Rapidly progressive Glomerulonephritis (Crescentic GN)
As the name suggests, this type has a poor prognosis, with rapid progression to kidney failure over weeks. Any of the above types of GN can be rapidly progressive. Additionally two further causes present as solely RPGN. One is Goodpasture's syndrome. This is an autoimmune disease whereby antibodies are directed against antigens found in the kidney and lungs. As well as kidney failure, patient have hemoptysis (cough up blood). High dose immunosupression is required (intravenous methylprednisone) and cyclophosphamide, plus plasmapharesis. Immunohistochemistry staining of tissue specimens shows linear IgG deposits. The second cause is vasculitic disorders such as Wegener's and polyarteritis. There is a lack of immune deposits on staining, but blood tests are positive for ANCA antibody.
Pathophysiology
Microscopic Pathology
-
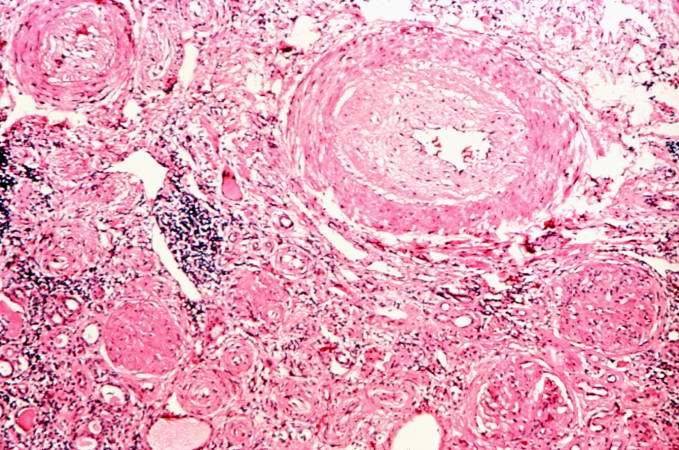
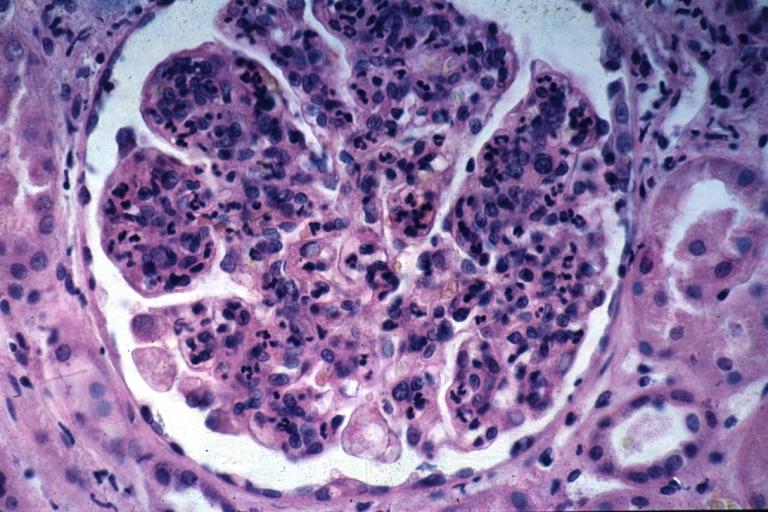
Glomerulonephritis: Micro H&E med mag; an excellent example of AGN with many neutrophils
-
Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis.
Glomerulonephritis Videos
Rapidly progressive glomerulonephritis
{{#ev:youtube|CqSyj4cVZPE}}
Chronic glomerulonephritis
{{#ev:youtube|eA1vYarRAWo}}
Images
-
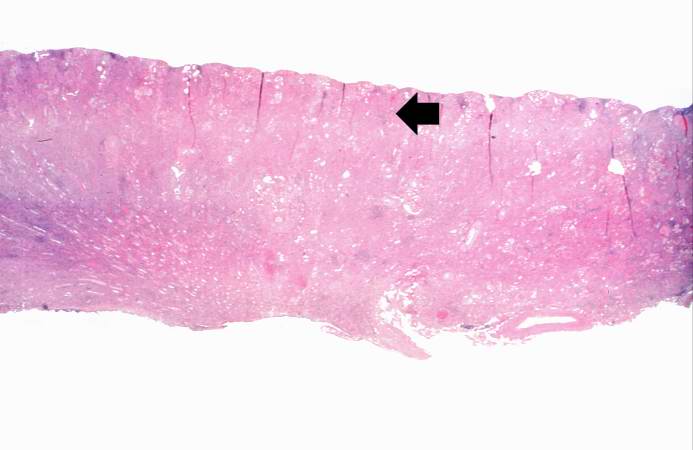
This is a low-power photomicrograph of a saggital section of end stage chronic glomerulonephritis (GN). Note the marked thinning of the cortex (arrow).
-
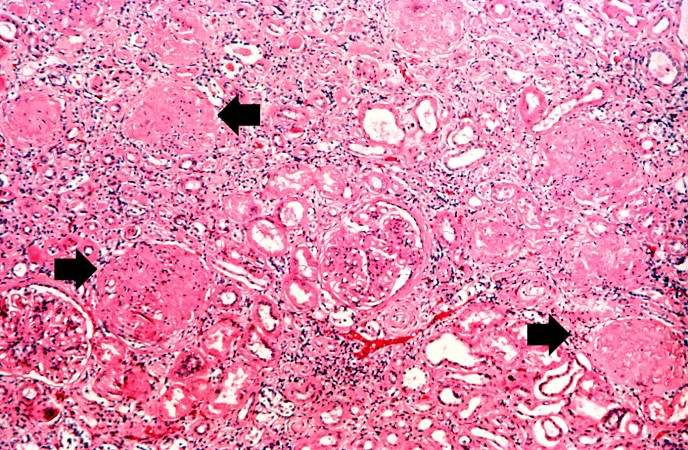
This is a higher-power photomicrograph of hyalinized glomeruli (arrows) and glomeruli with thick basement membranes.
-
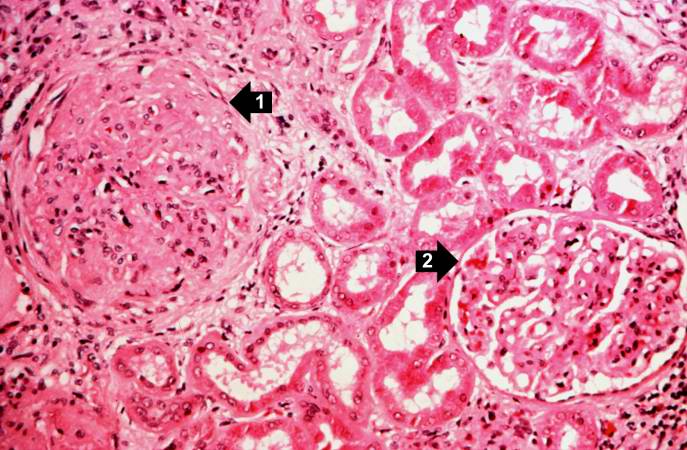
This is a higher-power photomicrograph of hyalinized glomeruli (1) and glomeruli with thickened basement membranes (2).
-
This is a photomicrograph of interstitial and vascular lesions in end stage renal disease.
-
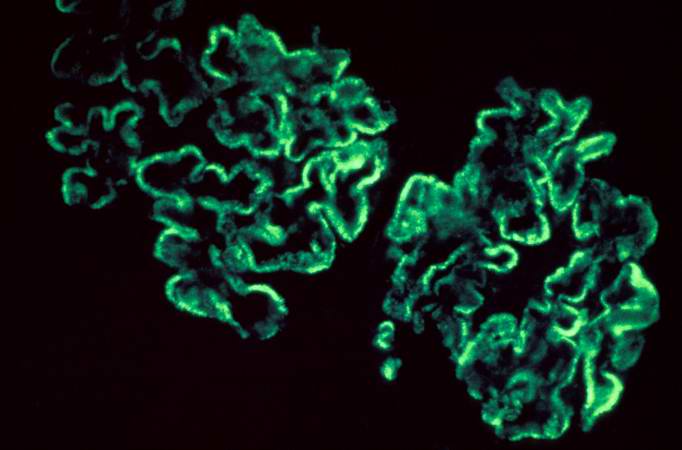
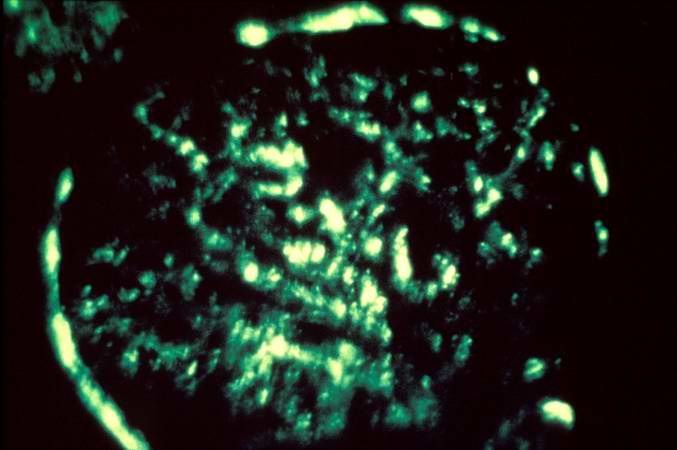
This is an immunofluorescent photomicrograph of granular membranous immunofluorescence (immune complex disease). The antibody used for these studies was specific for IgG.
-
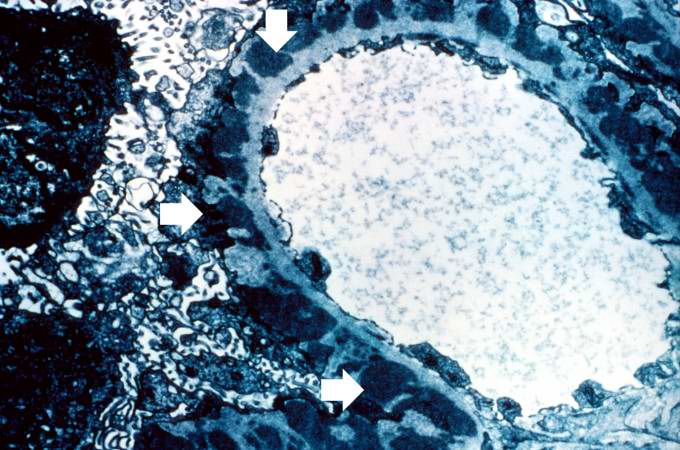
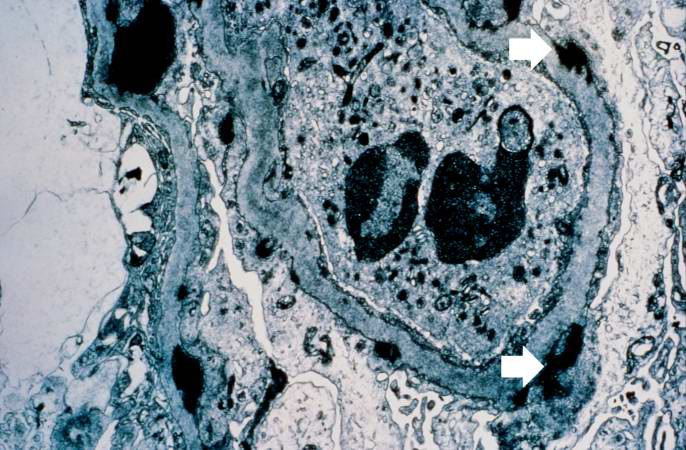
This is an electron micrograph of subepithelial granular electron dense deposits (arrows) which correspond to the granular immunofluorescence seen in the previous image.
-
This is a photomicrograph of a glomerulus from another case with acute poststreptococcal glomerulonephritis. In this case the immune complex glomerular disease is ongoing with necrosis and accumulation of neutrophils in the glomerulus.
-
This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern.
-
This electron micrograph demonstrates scattered subepithelial dense deposits (arrows) and a polymorphonuclear leukocyte in the lumen.
-
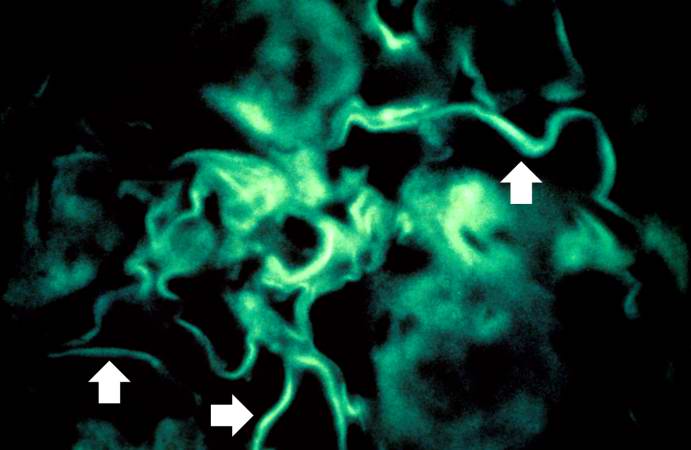
For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome.
Images:
Differential Diagnosis
Glomerulonephritis may be proliferative or non-proliferative and may be associated with nephrotic or nephritic features. The various types of glomerulonephritides should be differentiated from each other based on associations, presence of pitting edema, hemeturia, hypertension, hemoptysis, oliguria, peri-orbital edema, hyperlipidemia, type of antibodies, light and electron microscopic features. The following table differentiates between various types of glomerulonephritides:[1][2][3][4][5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24]
| Glomerulonephritis | Sub-entity | Causes and associations | History and Symtoms | Laboratory Findings | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyperlipidemia and hypercholesterolemia | Nephrotic features | Nephritic features | ANCA | Anti-glomerular basement membrane antibody (Anti-GBM antibody) | Immune complex formation | Light microscope | Electron microscope | Immunoflourescence pattern | ||||||||||
| History | Pitting edema | Hemeturia (pre-dominantly microscopic) | Hypertension | Hemoptysis | Oliguria | Peri-orbital edema | ||||||||||||
| Non-proliferative | Minimal change disease |
|
|
+ |
- |
- |
- |
+/- |
- |
+ |
+ |
- |
- |
- |
- |
|
|
- |
| Focal segmental glomerulosclerosis |
|
|
+ | - | - | - | +/- | - | + | + | - | - | - | - |
|
|
- | |
| Membranous glomerulonephritis |
|
+ | - | - | - | +/- | - | + | + | - | - | - | + |
|
- | |||
| Proliferative | IgA nephropathy |
|
+/- | + | + | - | + | +/- | - | - | + | - | - | + |
|
|
- | |
| Rapidly progressive glomerulonephritis |
|
+/- | + | + | + | + | + | - | - | + | - | + | + |
|
+ (Linear) | |||
|
+/- | + | + | + | + | + | - | - | + | - | - | + |
|
+ (Granular) | ||||
|
+/- | + | + | + | + | + | - | - | + | + (C-ANCA) | - | - | - (pauci-immune) | +/- | ||||
| +/- | + | + | + | + | + | - | - | + |
+ (C-ANCA) |
- | - | - (pauci-immune) | - | |||||
| +/- | + | + | + | + | + | - | - | + |
+ (P-ANCA) |
- | - | - (pauci-immune) | - | |||||
| Membranoproliferative glomerulonephritis |
|
+/- | + | + | + | + | + | - | + | - | - | - | + |
|
+ (Granular) | |||
References
- ↑ Saha TC, Singh H (November 2006). "Minimal change disease: a review". South. Med. J. 99 (11): 1264–70. doi:10.1097/01.smj.0000243183.87381.c2. PMID 17195422.
- ↑ Saleem MA, Kobayashi Y (2016). "Cell biology and genetics of minimal change disease". F1000Res. 5. doi:10.12688/f1000research.7300.1. PMC 4821284. PMID 27092244.
- ↑ Keskar V, Jamale TE, Kulkarni MJ, Kiggal Jagadish P, Fernandes G, Hase N (October 2013). "Minimal-change disease in adolescents and adults: epidemiology and therapeutic response". Clin Kidney J. 6 (5): 469–72. doi:10.1093/ckj/sft063. PMC 4438390. PMID 26064510.
- ↑ Chugh SS, Clement LC, Macé C (February 2012). "New insights into human minimal change disease: lessons from animal models". Am. J. Kidney Dis. 59 (2): 284–92. doi:10.1053/j.ajkd.2011.07.024. PMC 3253318. PMID 21974967.
- ↑ Rosenberg AZ, Kopp JB (March 2017). "Focal Segmental Glomerulosclerosis". Clin J Am Soc Nephrol. 12 (3): 502–517. doi:10.2215/CJN.05960616. PMC 5338705. PMID 28242845.
- ↑ Jefferson JA, Shankland SJ (September 2014). "The pathogenesis of focal segmental glomerulosclerosis". Adv Chronic Kidney Dis. 21 (5): 408–16. doi:10.1053/j.ackd.2014.05.009. PMC 4149756. PMID 25168829.
- ↑ Gephardt GN, Tubbs RR, Popowniak KL, McMahon JT (October 1986). "Focal and segmental glomerulosclerosis. Immunohistologic study of 20 renal biopsy specimens". Arch. Pathol. Lab. Med. 110 (10): 902–5. PMID 2429634.
- ↑ Lai WL, Yeh TH, Chen PM, Chan CK, Chiang WC, Chen YM, Wu KD, Tsai TJ (February 2015). "Membranous nephropathy: a review on the pathogenesis, diagnosis, and treatment". J. Formos. Med. Assoc. 114 (2): 102–11. doi:10.1016/j.jfma.2014.11.002. PMID 25558821.
- ↑ Wasserstein AG (April 1997). "Membranous glomerulonephritis". J. Am. Soc. Nephrol. 8 (4): 664–74. PMID 10495797.
- ↑ Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA (October 2011). "The pathophysiology of IgA nephropathy". J. Am. Soc. Nephrol. 22 (10): 1795–803. doi:10.1681/ASN.2011050464. PMC 3892742. PMID 21949093.
- ↑ Wyatt RJ, Julian BA (June 2013). "IgA nephropathy". N. Engl. J. Med. 368 (25): 2402–14. doi:10.1056/NEJMra1206793. PMID 23782179.
- ↑ He S, Wu Z (November 2011). "Gene-based Higher Criticism methods for large-scale exonic single-nucleotide polymorphism data". BMC Proc. 5 Suppl 9: S65. doi:10.1186/1753-6561-5-S9-S65. PMC 3287904. PMID 22373436.
- ↑ Higgins RM, Goldsmith DJ, Connolly J, Scoble JE, Hendry BM, Ackrill P, Venning MC (January 1996). "Vasculitis and rapidly progressive glomerulonephritis in the elderly". Postgrad Med J. 72 (843): 41–4. PMC 2398323. PMID 8746284.
- ↑ Jennette JC (March 2003). "Rapidly progressive crescentic glomerulonephritis". Kidney Int. 63 (3): 1164–77. doi:10.1046/j.1523-1755.2003.00843.x. PMID 12631105.
- ↑ Bolton WK (November 1996). "Goodpasture's syndrome". Kidney Int. 50 (5): 1753–66. PMID 8914046.
- ↑ Mathew TH, Hobbs JB, Kalowski S, Sutherland PW, Kincaid-Smith P (February 1975). "Goodpasture's syndrome: normal renal diagnostic findings". Ann. Intern. Med. 82 (2): 215–8. PMID 1090223.
- ↑ Renaudineau Y, Le Meur Y (October 2008). "Renal involvement in Wegener's granulomatosis". Clin Rev Allergy Immunol. 35 (1–2): 22–9. doi:10.1007/s12016-007-8066-6. PMID 18172777.
- ↑ Weiss MA, Crissman JD (October 1984). "Renal biopsy findings in Wegener's granulomatosis: segmental necrotizing glomerulonephritis with glomerular thrombosis". Hum. Pathol. 15 (10): 943–56. PMID 6384024.
- ↑ Sinico RA, Di Toma L, Maggiore U, Tosoni C, Bottero P, Sabadini E, Giammarresi G, Tumiati B, Gregorini G, Pesci A, Monti S, Balestrieri G, Garini G, Vecchio F, Buzio C (May 2006). "Renal involvement in Churg-Strauss syndrome". Am. J. Kidney Dis. 47 (5): 770–9. doi:10.1053/j.ajkd.2006.01.026. PMID 16632015.
- ↑ Cartin-Ceba R, Keogh KA, Specks U, Sethi S, Fervenza FC (September 2011). "Rituximab for the treatment of Churg-Strauss syndrome with renal involvement". Nephrol. Dial. Transplant. 26 (9): 2865–71. doi:10.1093/ndt/gfq852. PMC 3218640. PMID 21325353.
- ↑ Chung SA, Seo P (August 2010). "Microscopic polyangiitis". Rheum. Dis. Clin. North Am. 36 (3): 545–58. doi:10.1016/j.rdc.2010.04.003. PMC 2917831. PMID 20688249.
- ↑ Pagnoux C (March 2008). "[Wegener's granulomatosis and microscopic polyangiitis]". Rev Prat (in French). 58 (5): 522–32. PMID 18524109.
- ↑ Alchi B, Jayne D (August 2010). "Membranoproliferative glomerulonephritis". Pediatr. Nephrol. 25 (8): 1409–18. doi:10.1007/s00467-009-1322-7. PMC 2887509. PMID 19908070.
- ↑ Davis AE, Schneeberger EE, Grupe WE, McCluskey RT (May 1978). "Membranoproliferative glomerulonephritis (MPGN type I) and dense deposit disease (DDD) in children". Clin. Nephrol. 9 (5): 184–93. PMID 657595.