Glioma MRI
|
Glioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Glioma MRI On the Web |
|
American Roentgen Ray Society Images of Glioma MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2], Sujit Routray, M.D. [3]
Overview
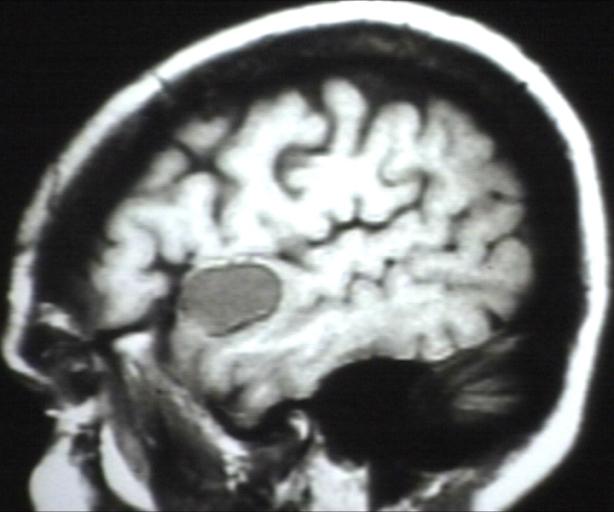
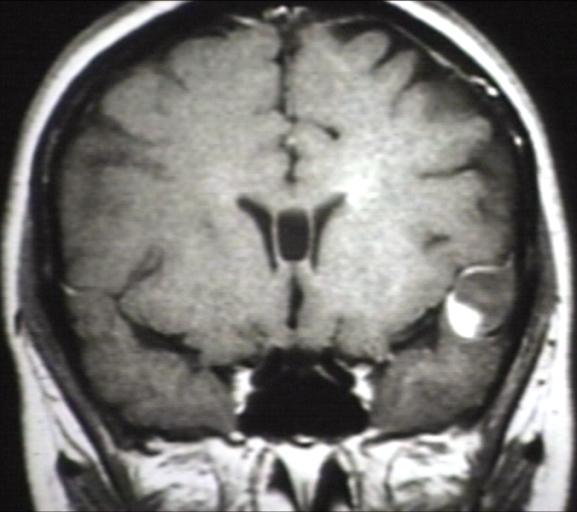
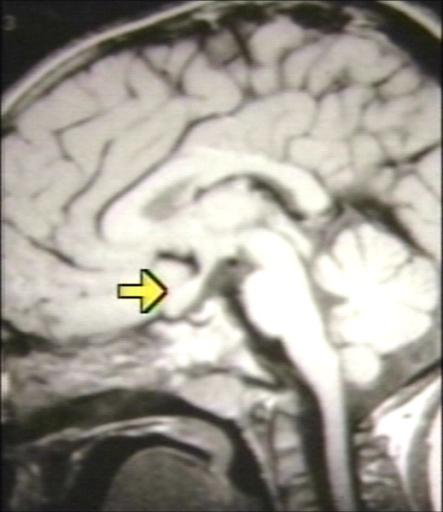
Brain MRI may be diagnostic of glioma.[1][2][3][4][5][6]
MRI
Brain MRI may be diagnostic of glioma.[1][2][3][4][5][6]
| Type of glioma | CT findings |
|---|---|
| |
| |
| |
| |
| |
|
References
- ↑ 1.0 1.1 Radiological findings of pilocytic astrocytoma. Radiopaedia.org 2015. http://radiopaedia.org/articles/pilocytic-astrocytoma
- ↑ 2.0 2.1 Radiological findings of low grade infiltrative astrocytoma. http://radiopaedia.org/articles/low-grade-infiltrative-astrocytoma
- ↑ 3.0 3.1 Radiological findings of anaplastic astrocytoma. http://radiopaedia.org/articles/anaplastic-astrocytoma
- ↑ 4.0 4.1 Radiological findings of glioblastoma. http://radiopaedia.org/articles/glioblastoma
- ↑ 5.0 5.1 Radiological findings of oligodendroglioma. http://radiopaedia.org/articles/oligodendroglioma
- ↑ 6.0 6.1 Radiological findings of ependymoma. Radiopaedia.org 2015. http://radiopaedia.org/articles/ependymoma