Glioma CT: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
(→CT) |
||
| Line 18: | Line 18: | ||
[[Pilocytic astrocytoma]] | [[Pilocytic astrocytoma]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
:1. Large cystic component with a brightly enhancing mural nodule (67%) | :1. Large [[cystic]] component with a brightly enhancing mural nodule (67%) | ||
:* Non enhancing cyst wall (21%) | :* Non enhancing cyst wall (21%) | ||
:* Enhancing cyst wall (46%) | :* Enhancing cyst wall (46%) | ||
:2. Heterogeneous, mixed solid and multiple cysts and central necrosis (16%) | :2. Heterogeneous, mixed solid and multiple cysts and central [[necrosis]] (16%) | ||
:3. Completely solid (17%) | :3. Completely solid (17%) | ||
|- | |- | ||
| Line 30: | Line 30: | ||
:2. Positive mass effect | :2. Positive mass effect | ||
:3. No enhancement | :3. No enhancement | ||
:4. Calcification is rare | :4. [[Calcification]] is rare | ||
:5. Cystic component | :5. Cystic component | ||
|- | |- | ||
| Line 47: | Line 47: | ||
:3. Marked mass effect | :3. Marked mass effect | ||
:4. Surrounding vasogenic [[edema]] | :4. Surrounding vasogenic [[edema]] | ||
:5. Hemorrhage | :5. [[Hemorrhage]] | ||
:6. Calcification is rare | :6. [[Calcification]] is rare | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | ||
| Line 54: | Line 54: | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
:1. Hypodense to isodense | :1. Hypodense to isodense | ||
:2. Calcification (70-90%) | :2. [[Calcification]] (70-90%) | ||
:3. Hemorrhage | :3. [[Hemorrhage]] | ||
:4. Overlying skull may show pressure erosion | :4. Overlying skull may show pressure erosion | ||
|- | |- | ||
| Line 61: | Line 61: | ||
[[Ependymoma]] | [[Ependymoma]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
:1. Coarse calcification is common (50%) | :1. Coarse [[calcification]] is common (50%) | ||
:2. Cystic areas (50%) | :2. Cystic areas (50%) | ||
:3. Iso- to hypodense solid component | :3. Iso- to hypodense solid component | ||
:4. Heterogeneous enhancement | :4. Heterogeneous enhancement | ||
:5. Hemorrhage | :5. [[Hemorrhage]] | ||
|} | |} | ||
Revision as of 18:32, 22 September 2015
|
Glioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Glioma CT On the Web |
|
American Roentgen Ray Society Images of Glioma CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2], Sujit Routray, M.D. [3]
Overview
Head CT scan may be diagnostic of glioma.
CT
Head CT scan may be diagnostic of glioma.[1][2][3][4][5][6]
| Type of glioma | CT findings |
|---|---|
| |
| |
| |
| |
|
-
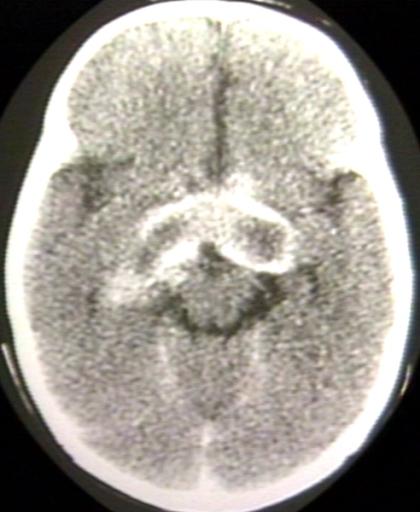
BRAIN: GLIOMA, OPTICOCHIASMATIC; WITH CONTRAST
-
BRAIN: GLIOMA, OPTICOCHIASMATIC; 1 OF 4 WITHOUT CONTRAST
-
BRAIN: GLIOMA, OPTICOCHIASMATIC; 2 OF 4 WITH CONTRAST
-
BRAIN: GLIOMA, OPTICOCHIASMATIC; 3 OF 4 WITH CONTRAST
-
BRAIN: GLIOMA, OPTICOCHIASMATIC; 4 OF 4 WITH CONTRAST
References
- ↑ Radiological findings of pilocytic astrocytoma. Radiopaedia.org 2015. http://radiopaedia.org/articles/pilocytic-astrocytoma
- ↑ Radiological findings of low grade infiltrative astrocytoma. http://radiopaedia.org/articles/low-grade-infiltrative-astrocytoma
- ↑ Radiological findings of anaplastic astrocytoma. http://radiopaedia.org/articles/anaplastic-astrocytoma
- ↑ Radiological findings of glioblastoma. http://radiopaedia.org/articles/glioblastoma
- ↑ Radiological findings of oligodendroglioma. http://radiopaedia.org/articles/oligodendroglioma
- ↑ Radiological findings of ependymoma. Radiopaedia.org 2015. http://radiopaedia.org/articles/ependymoma