Esophageal stricture pathophysiology: Difference between revisions
No edit summary |
|||
| (20 intermediate revisions by 6 users not shown) | |||
| Line 4: | Line 4: | ||
{{CMG}}; {{AE}} {{MA}} | {{CMG}}; {{AE}} {{MA}} | ||
==Overview== | ==Overview== | ||
Esophageal stricture is the result of lower pressure of [[esophageal sphincter]] in [[gastroesophageal reflux disease]], esophageal motor disorder, and [[inflammation]] and [[fibrosis]] in [[neoplasia]]. The characteristic findings on [[gross pathology]] are thickening of the lower [[esophageal]] wall in [[gastroesophageal reflux disease]], pale [[mucosa]] in [[lymphocytic]] [[esophagitis]], and [[hemorrhagic]] [[congestion]] in [[caustic]] ingestion. Characteristic [[histopathological]] findings of esophageal stricture are intraepithelial [[lymphocytes|lymphocytosis]] and [[basal cell]] [[hyperplasia]] in [[gastroesophageal reflux disease]]; [[T cell|T lymphocyte]] infiltration in [[squamous]] [[mucosa]] in [[lymphocytic]] [[esophagitis]] and [[eosinophilic]] [[necrosis]] in [[Caustic burn|caustic ingestion]]. | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
{|align="right" | {| align="right" | ||
| | | | ||
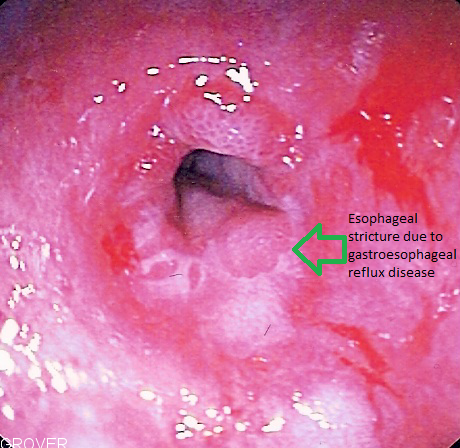
[[File:Esophageal stricture due to GERD.png|300px|thumb|Esophageal stricture due to GERD, via wikipedia.org<ref>From en.wikipedia.org, Public Domain, <"https://commons.wikimedia.org/w/index.php?curid=1931423"></ref>]] | [[File:Esophageal stricture due to GERD.png|300px|thumb|Esophageal stricture due to GERD, via wikipedia.org<ref>From en.wikipedia.org, Public Domain, <"https://commons.wikimedia.org/w/index.php?curid=1931423"></ref>]] | ||
|} | |} | ||
The normal [[esophageal]] diameter is up to 30 mm. An esophageal | The normal [[esophageal]] diameter is up to 30 mm. An esophageal stricture is a narrowing of the [[esophagus]] usually 13 mm or less in diameter that causes [[dysphagia]]. [[Peptic]] strictures occur usually at the squamocolumnar junction.<ref name="pmid8338082">{{cite journal |vauthors=Marks RD, Richter JE |title=Peptic strictures of the esophagus |journal=Am. J. Gastroenterol. |volume=88 |issue=8 |pages=1160–73 |year=1993 |pmid=8338082 |doi= |url=}}</ref> | ||
* | Esophageal stricture is the result of:<ref name=":0">{{cite book | last = Holzheimer | first = R | title = Surgical treatment : evidence-based and problem-oriented | publisher = Zuckschwerdt | location = München New York | year = 2001 | isbn = 3-88603-714-2 }}</ref><ref name="pmid24640761">{{cite journal |vauthors=Belevich VL, Ovchinnikov DV |title=[Treatment of benign esophageal stricture] |language=Russian |journal=Vestn. Khir. Im. I. I. Grek. |volume=172 |issue=5 |pages=111–4 |year=2013 |pmid=24640761 |doi= |url=}}</ref> | ||
* | |||
*Lower pressure of [[esophageal sphincter]] in [[gastroesophageal reflux disease]] | |||
*[[Esophageal]] motor disorders | |||
*[[Inflammation]] and [[fibrosis]] due to intrinsic diseases of [[esophagus]], such as [[neoplasia]] | |||
*Most peptic strictures are result of chronic [[reflux esophagitis]] and the process of esophageal | *Surgical esophageal [[anastomosis]] | ||
**[[Lower esophageal sphincter]] (LES) tone is | *[[Esophageal]] compression by other organs | ||
*[[Radiation therapy]] for thoracic or head and neck [[tumors]] is one of the less common cause of proximal esophageal | |||
*Most [[peptic]] strictures are result of chronic [[reflux esophagitis]] and the process of esophageal stricture is due to [[mucosal]] [[edema]] and [[Infiltration (medical)|infiltration]] of [[inflammatory cells]] in lamina propria and finally [[collagen]] deposits, [[fibrosis]] and [[scar]] of [[esophagus]].<ref name="pmid8338082" /> | |||
**[[Lower esophageal sphincter]] (LES) tone is usually less than 8 mmHg in esophageal stricture due to [[reflux esophagitis]]. | |||
*[[Radiation therapy]] for [[thoracic]] or head and neck [[tumors]] is one of the less common cause of proximal esophageal stricture by inducing chronic [[ischemia]] and [[fibrosis]].<ref name="pmid89440642">{{cite journal |vauthors=Dhir V, Vege SS, Mohandas KM, Desai DC |title=Dilation of proximal esophageal strictures following therapy for head and neck cancer: experience with Savary Gilliard dilators |journal=J Surg Oncol |volume=63 |issue=3 |pages=187–90 |year=1996 |pmid=8944064 |doi=10.1002/(SICI)1096-9098(199611)63:3<187::AID-JSO10>3.0.CO;2-2 |url=}}</ref> | |||
*[[Liquefactive necrosis]] is the mechanism of esophageal stricture in [[alkali]] ingestion and [[superficial]] [[coagulation necrosis]] is the mechanism of esophageal stricture in [[acid]] ingestion.<ref name="pmid4012549">{{cite journal |vauthors=Fisher RA, Eckhauser ML, Radivoyevitch M |title=Acid ingestion in an experimental model |journal=Surg Gynecol Obstet |volume=161 |issue=1 |pages=91–9 |year=1985 |pmid=4012549 |doi= |url=}}</ref><ref name="pmid1539568">{{cite journal |vauthors=Zargar SA, Kochhar R, Nagi B, Mehta S, Mehta SK |title=Ingestion of strong corrosive alkalis: spectrum of injury to upper gastrointestinal tract and natural history |journal=Am. J. Gastroenterol. |volume=87 |issue=3 |pages=337–41 |year=1992 |pmid=1539568 |doi= |url=}}</ref> | |||
**A grading system for [[esophageal]] injury due to [[caustic]] ingestion: | |||
{| class="wikitable" | {| class="wikitable" | ||
!Grade | !Grade | ||
| Line 50: | Line 52: | ||
==Genetics== | ==Genetics== | ||
[[Gene]]<nowiki/>s involved in the [[pathogenesis]] of esophageal stricture due to [[Dyskeratosis congenita|Dyskeratosis Congenita]] include:<ref name="pmid20301779">{{cite journal |vauthors=Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Mefford HC, Stephens K, Amemiya A, Ledbetter N, Savage SA |title= |journal= |volume= |issue= |pages= |year= |pmid=20301779 |doi= |url=}}</ref> | |||
*''[[ACD (gene)|ACD]]'' | *''[[ACD (gene)|ACD]]'' | ||
*''CTC1'' | *''CTC1'' | ||
| Line 62: | Line 65: | ||
*''[[TINF2]]'' | *''[[TINF2]]'' | ||
*''WRAP53 '' | *''WRAP53 '' | ||
==Associated Conditions== | ==Associated Conditions== | ||
*The most important diseases associated with esophageal | |||
*The most important diseases associated with esophageal stricture include: | |||
**[[Gastroesophageal reflux disease]] | **[[Gastroesophageal reflux disease]] | ||
**[[Caustic]] ingestion | **[[Caustic]] ingestion | ||
==Gross Pathology== | ==Gross Pathology== | ||
*On [[gross pathology]], circumferential thickening of the lower esophageal wall are characteristic finding of | |||
*Pale [[mucosa]] with white [[exudate]] in lymphocytic [[esophagitis]]<ref name="MaejimaUno2016">{{cite journal|last1=Maejima|first1=Ryuhei|last2=Uno|first2=Kaname|last3=Iijima|first3=Katsunori|last4=Fujishima|first4=Fumiyoshi|last5=Noguchi|first5=Tetsuya|last6=Ara|first6=Nobuyuki|last7=Asano|first7=Naoki|last8=Koike|first8=Tomoyuki|last9=Imatani|first9=Akira|last10=Shimosegawa|first10=Tooru|title=A Japanese case of lymphocytic esophagitis|journal=Digestive Endoscopy|volume=28|issue=4|year=2016|pages=476–480|issn=09155635|doi=10.1111/den.12578}}</ref> | *On [[gross pathology]], circumferential thickening of the lower [[esophageal]] wall are characteristic finding of esophageal stricture due to [[gastroesophageal reflux disease]].<ref name="YamasakiOzawa2016">{{cite journal|last1=Yamasaki|first1=Yasushi|last2=Ozawa|first2=Soji|last3=Oguma|first3=Junya|last4=Kazuno|first4=Akihito|last5=Ninomiya|first5=Yamato|title=Long peptic strictures of the esophagus due to reflux esophagitis: a case report|journal=Surgical Case Reports|volume=2|issue=1|year=2016|issn=2198-7793|doi=10.1186/s40792-016-0190-1}}</ref> | ||
*[[Swelling]] and [[hemorrhagic]] [[congestion]] in [[caustic]] ingestion <ref name="Contini2013">{{cite journal|last1=Contini|first1=Sandro|title=Caustic injury of the upper gastrointestinal tract: A comprehensive review|journal=World Journal of Gastroenterology|volume=19|issue=25|year=2013|pages=3918|issn=1007-9327|doi=10.3748/wjg.v19.i25.3918}}</ref> | *Pale [[mucosa]] with white [[exudate]] in [[lymphocytic]] [[esophagitis]]<ref name="MaejimaUno2016">{{cite journal|last1=Maejima|first1=Ryuhei|last2=Uno|first2=Kaname|last3=Iijima|first3=Katsunori|last4=Fujishima|first4=Fumiyoshi|last5=Noguchi|first5=Tetsuya|last6=Ara|first6=Nobuyuki|last7=Asano|first7=Naoki|last8=Koike|first8=Tomoyuki|last9=Imatani|first9=Akira|last10=Shimosegawa|first10=Tooru|title=A Japanese case of lymphocytic esophagitis|journal=Digestive Endoscopy|volume=28|issue=4|year=2016|pages=476–480|issn=09155635|doi=10.1111/den.12578}}</ref> | ||
*[[Swelling]] and [[hemorrhagic]] [[congestion]] in [[caustic]] ingestion<ref name="Contini2013">{{cite journal|last1=Contini|first1=Sandro|title=Caustic injury of the upper gastrointestinal tract: A comprehensive review|journal=World Journal of Gastroenterology|volume=19|issue=25|year=2013|pages=3918|issn=1007-9327|doi=10.3748/wjg.v19.i25.3918}}</ref> | |||
*Multiple yellow [[plaque]]<nowiki/>s in infectious [[esophagitis]] due to ''Candida''<ref name="pmid24719600">{{cite journal |vauthors=Wilcox CM |title=Overview of infectious esophagitis |journal=Gastroenterol Hepatol (N Y) |volume=9 |issue=8 |pages=517–9 |year=2013 |pmid=24719600 |pmc=3980995 |doi= |url=}}</ref> | |||
*Ulceration of the [[esophagus]] in [[viral]] [[esophagitis]] | |||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
{| align="right" | {| align="right" | ||
| | | | ||
[[File:Esophagus path.jpg| | [[File:Esophagus path.jpg|300px|thumb|Normal esophagus, via Wikimedia.org<ref><"https://commons.wikimedia.org/wiki/File%3ATinci%C3%B3n_hematoxilina-eosina.jpg"> via Wikimedia Commons</ref>]] | ||
[[File:Gastroesophageal refllux disease.jpeg|300px|thumb|Gastroesophageal refllux disease, via Wikimedia.org<ref>"https://commons.wikimedia.org/wiki/File%3AGastroesophageal_reflux_disease_--_low_mag.jpg">via Wikimedia Commons</ref>]] | |||
|} | |} | ||
*On microscopic histopathological analysis, characteristic findings of esophageal stricture due to [[gastroesophageal reflux disease]] are:<ref name="urlEsophageal stricture - Libre Pathology">{{cite web |url=https://librepathology.org/wiki/Esophageal_stricture |title=Esophageal stricture - Libre Pathology |format= |work= |accessdate=}}</ref> | *On [[microscopic]] [[histopathological]] analysis, characteristic findings of esophageal stricture due to [[gastroesophageal reflux disease]] are:<ref name="urlEsophageal stricture - Libre Pathology">{{cite web |url=https://librepathology.org/wiki/Esophageal_stricture |title=Esophageal stricture - Libre Pathology |format= |work= |accessdate=}}</ref> | ||
**Intraepithelial [[lymphocyte]]s | **Intraepithelial [[lymphocyte|lymphocytosi]]s | ||
**Basal cell [[hyperplasia]] | **[[Basal cell]] [[hyperplasia]] | ||
**[[Ulceration]] <ref name="YamasakiOzawa2016" /> | **[[Ulceration]] <ref name="YamasakiOzawa2016" /> | ||
*[[Microscopic]] [[histopathological]] characteristic findings of | *[[Microscopic]] [[histopathological]] characteristic findings of esophageal stricture due to [[Lymphocyte|lymphocytic]] [[esophagitis]] are:<ref name="MaejimaUno2016" /> | ||
**[[Infiltration (medical)|Infiltration]] of many [[CD3 (immunology)|CD3+]] /[[CD4+]] / [[CD8+ T cells|CD8+]] [[T lymphocytes]] in [[squamous]] [[mucosa]] in the peripapaillary region without any [[Granulocyte|granulocytes]] | **[[Infiltration (medical)|Infiltration]] of many [[CD3 (immunology)|CD3+]] /[[CD4+]] / [[CD8+ T cells|CD8+]] [[T lymphocytes]] in [[squamous]] [[mucosa]] in the peripapaillary region without any [[Granulocyte|granulocytes]] | ||
*[[Eosinophilic]] [[necrosis]] in esophageal | *[[Eosinophilic]] [[necrosis]] in esophageal stricture due to [[caustic]] ingestion<ref name="Contini2013" /> | ||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
==References== | ==References== | ||
| Line 92: | Line 130: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
<references /> | |||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
Latest revision as of 03:28, 24 October 2020
|
Esophageal stricture Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Esophageal stricture pathophysiology On the Web |
|
American Roentgen Ray Society Images of Esophageal stricture pathophysiology |
|
Risk calculators and risk factors for Esophageal stricture pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mahda Alihashemi M.D. [2]
Overview
Esophageal stricture is the result of lower pressure of esophageal sphincter in gastroesophageal reflux disease, esophageal motor disorder, and inflammation and fibrosis in neoplasia. The characteristic findings on gross pathology are thickening of the lower esophageal wall in gastroesophageal reflux disease, pale mucosa in lymphocytic esophagitis, and hemorrhagic congestion in caustic ingestion. Characteristic histopathological findings of esophageal stricture are intraepithelial lymphocytosis and basal cell hyperplasia in gastroesophageal reflux disease; T lymphocyte infiltration in squamous mucosa in lymphocytic esophagitis and eosinophilic necrosis in caustic ingestion.
Pathophysiology
Pathogenesis
 |
The normal esophageal diameter is up to 30 mm. An esophageal stricture is a narrowing of the esophagus usually 13 mm or less in diameter that causes dysphagia. Peptic strictures occur usually at the squamocolumnar junction.[2]
Esophageal stricture is the result of:[3][4]
- Lower pressure of esophageal sphincter in gastroesophageal reflux disease
- Esophageal motor disorders
- Inflammation and fibrosis due to intrinsic diseases of esophagus, such as neoplasia
- Surgical esophageal anastomosis
- Esophageal compression by other organs
- Most peptic strictures are result of chronic reflux esophagitis and the process of esophageal stricture is due to mucosal edema and infiltration of inflammatory cells in lamina propria and finally collagen deposits, fibrosis and scar of esophagus.[2]
- Lower esophageal sphincter (LES) tone is usually less than 8 mmHg in esophageal stricture due to reflux esophagitis.
- Radiation therapy for thoracic or head and neck tumors is one of the less common cause of proximal esophageal stricture by inducing chronic ischemia and fibrosis.[5]
- Liquefactive necrosis is the mechanism of esophageal stricture in alkali ingestion and superficial coagulation necrosis is the mechanism of esophageal stricture in acid ingestion.[6][7]
- A grading system for esophageal injury due to caustic ingestion:
| Grade | pathophysiological injury |
|---|---|
| 0 | Normal |
| 1 | Mucosal edema and hyperemia |
| 2A | Superficial ulcers, bleeding, exudates |
| 2B | Deep focal or circumferential ulcers |
| 3A | Focal necrosis |
| 3B | Extensive necrosis |
Genetics
Genes involved in the pathogenesis of esophageal stricture due to Dyskeratosis Congenita include:[8]
Associated Conditions
- The most important diseases associated with esophageal stricture include:
- Gastroesophageal reflux disease
- Caustic ingestion
Gross Pathology
- On gross pathology, circumferential thickening of the lower esophageal wall are characteristic finding of esophageal stricture due to gastroesophageal reflux disease.[9]
- Pale mucosa with white exudate in lymphocytic esophagitis[10]
- Swelling and hemorrhagic congestion in caustic ingestion[11]
- Multiple yellow plaques in infectious esophagitis due to Candida[12]
- Ulceration of the esophagus in viral esophagitis
Microscopic Pathology
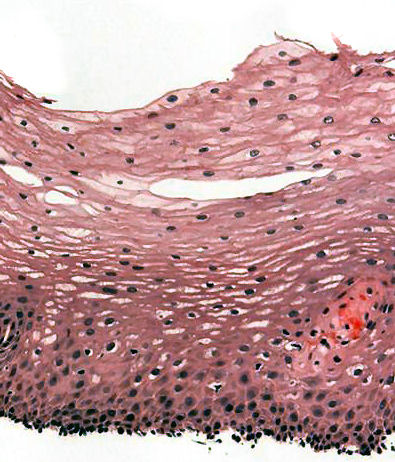  |
- On microscopic histopathological analysis, characteristic findings of esophageal stricture due to gastroesophageal reflux disease are:[15]
- Intraepithelial lymphocytosis
- Basal cell hyperplasia
- Ulceration [9]
- Microscopic histopathological characteristic findings of esophageal stricture due to lymphocytic esophagitis are:[10]
- Infiltration of many CD3+ /CD4+ / CD8+ T lymphocytes in squamous mucosa in the peripapaillary region without any granulocytes
- Eosinophilic necrosis in esophageal stricture due to caustic ingestion[11]
References
- ↑ From en.wikipedia.org, Public Domain, <"https://commons.wikimedia.org/w/index.php?curid=1931423">
- ↑ 2.0 2.1 Marks RD, Richter JE (1993). "Peptic strictures of the esophagus". Am. J. Gastroenterol. 88 (8): 1160–73. PMID 8338082.
- ↑ Holzheimer, R (2001). Surgical treatment : evidence-based and problem-oriented. München New York: Zuckschwerdt. ISBN 3-88603-714-2.
- ↑ Belevich VL, Ovchinnikov DV (2013). "[Treatment of benign esophageal stricture]". Vestn. Khir. Im. I. I. Grek. (in Russian). 172 (5): 111–4. PMID 24640761.
- ↑ Dhir V, Vege SS, Mohandas KM, Desai DC (1996). "Dilation of proximal esophageal strictures following therapy for head and neck cancer: experience with Savary Gilliard dilators". J Surg Oncol. 63 (3): 187–90. doi:10.1002/(SICI)1096-9098(199611)63:3<187::AID-JSO10>3.0.CO;2-2. PMID 8944064.
- ↑ Fisher RA, Eckhauser ML, Radivoyevitch M (1985). "Acid ingestion in an experimental model". Surg Gynecol Obstet. 161 (1): 91–9. PMID 4012549.
- ↑ Zargar SA, Kochhar R, Nagi B, Mehta S, Mehta SK (1992). "Ingestion of strong corrosive alkalis: spectrum of injury to upper gastrointestinal tract and natural history". Am. J. Gastroenterol. 87 (3): 337–41. PMID 1539568.
- ↑ Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean L, Mefford HC, Stephens K, Amemiya A, Ledbetter N, Savage SA. PMID 20301779. Vancouver style error: initials (help); Missing or empty
|title=(help) - ↑ 9.0 9.1 Yamasaki, Yasushi; Ozawa, Soji; Oguma, Junya; Kazuno, Akihito; Ninomiya, Yamato (2016). "Long peptic strictures of the esophagus due to reflux esophagitis: a case report". Surgical Case Reports. 2 (1). doi:10.1186/s40792-016-0190-1. ISSN 2198-7793.
- ↑ 10.0 10.1 Maejima, Ryuhei; Uno, Kaname; Iijima, Katsunori; Fujishima, Fumiyoshi; Noguchi, Tetsuya; Ara, Nobuyuki; Asano, Naoki; Koike, Tomoyuki; Imatani, Akira; Shimosegawa, Tooru (2016). "A Japanese case of lymphocytic esophagitis". Digestive Endoscopy. 28 (4): 476–480. doi:10.1111/den.12578. ISSN 0915-5635.
- ↑ 11.0 11.1 Contini, Sandro (2013). "Caustic injury of the upper gastrointestinal tract: A comprehensive review". World Journal of Gastroenterology. 19 (25): 3918. doi:10.3748/wjg.v19.i25.3918. ISSN 1007-9327.
- ↑ Wilcox CM (2013). "Overview of infectious esophagitis". Gastroenterol Hepatol (N Y). 9 (8): 517–9. PMC 3980995. PMID 24719600.
- ↑ <"https://commons.wikimedia.org/wiki/File%3ATinci%C3%B3n_hematoxilina-eosina.jpg"> via Wikimedia Commons
- ↑ "https://commons.wikimedia.org/wiki/File%3AGastroesophageal_reflux_disease_--_low_mag.jpg">via Wikimedia Commons
- ↑ "Esophageal stricture - Libre Pathology".