|
|
| (66 intermediate revisions by 9 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = {{PAGENAME}} | | | Name = | |
| Image = Ebstein's anomaly 001.jpg| | | Image = Ebstein_diagram.jpg| |
| Caption = Chest X-ray of a patient with Ebstein's anomaly <br> [http://www.radswiki.net Image courtesy of RadsWiki]|
| |
| DiseasesDB = 4039 |
| |
| ICD10 = {{ICD10|Q|22|5|q|20}} |
| |
| ICD9 = {{ICD9|746.2}} |
| |
| ICDO = |
| |
| OMIM = 224700 |
| |
| MedlinePlus = |
| |
| eMedicineSubj = med |
| |
| eMedicineTopic = 627 |
| |
| MeshID = D004437 |
| |
| }} | | }} |
| {{SI}}
| |
| {{CMG}} and Claudia P. Hochberg, M.D. [mailto:chochber@bidmc.harvard.edu]
| |
| __NOTOC__
| |
| '''Contributors:''' [[User:Zorkun|Cafer Zorkun]] M.D. PhD.
| |
|
| |
| {{Editor Join}}
| |
|
| |
| ==Overview==
| |
|
| |
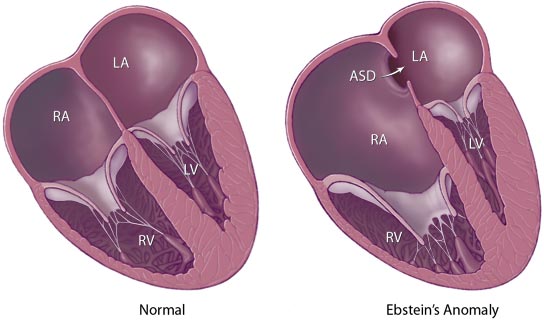
| '''Ebstein's anomaly''' is a congenital heart defect in which the opening of the [[tricuspid valve]] is displaced towards the apex of the [[right ventricle]] of the heart (congenital apical displacement of the [[tricuspid valve]] that typically causes significant [[tricuspid regurgitation]]).
| |
|
| |
| The annulus of the valve is in normal position. The valve leaflets however, are to a varying degree attached to the walls and septum of the [[right ventricle]]. There is subsequent atrialization of a portion of the morphologic right ventricle (which is then contiguous with the [[right atrium]]). This causes the [[right atrium]] to be large and the anatomic [[right ventricle]] to be small in size. 50% of cases involve an atrial shunt (either a [[PFO]] or an [[ASD]]).
| |
|
| |
| ==History==
| |
| Ebstein's anomaly was named after Wilhelm Ebstein.<ref>{{WhoNamedIt|synd|435}}</ref><ref>W. Ebstein. Über einen sehr seltenen Fall von Insufficienz der Valvula tricuspidalis, bedingt durch eine angeborene hochgradige Missbildung derselben. Archiv für Anatomie, Physiologie und wissenschaftliche Medicin, Leipzig, 1866, 238-254.</ref>
| |
|
| |
| ==Associated Abnormalities ==
| |
|
| |
| While Ebstein's anomaly is defined as the congenital displacement of the [[tricuspid valve]] towards the apex of the right ventricle, it is often associated with other abnormalities.
| |
|
| |
| == Anatomy ==
| |
|
| |
| Typically, there are anatomic abnormalities of the [[tricuspid valve]], with enlargement of the anterosuperior leaflet of the valve which is often adherent to the right ventricular free wall.
| |
|
| |
| About 50% of individuals with Ebstein's anomaly have an associated shunt between the right and [[left atrium]]s, either an [[atrial septal defect]] [[ASD]] or a [[patent foramen ovale]] [[PFO]].
| |
|
| |
| - The [[tricuspid valve]] leaflets are displaced toward the RV apex.
| |
|
| |
| - The RV cavity is dilated and the free wall is thin.
| |
|
| |
| - May be associated with LV dysfunction and [[mitral valve prolapse]] ([[MVP]]).
| |
|
| |
| - It has also been associated with [[right ventricular outflow tract obstruction|pulmonic stenosis]] [[right ventricular outflow tract obstruction| (PS)]], [[VSD]], [[pulmonary hypertension]], [[aortic stenosis|bicuspid aortic valve]] and right sided aortic arch.
| |
|
| |
| -It is commonly associated with congenitally corrected [[transposition of the great vessels]] and occasionally with [[tetralogy of Fallot]].
| |
|
| |
| - Is often associated with one or more accessory conduction pathways in 25%, and [[WPW]] in 13%. Usually this is a right sided accessory pathway.
| |
|
| |
| - The presence of an [[ASD]] permits right-to-left shunting and [[cyanosis]]. The degree of [[cyanosis]] is related to the degree of [[tricuspid regurgitation]] ([[tricuspid regurgitation|TR]]), [[tricuspid stenosis]] ([[tricuspid stenosis|TS]]) and the compliance of the RV.
| |
|
| |
| <div align="left">
| |
| <gallery heights="175" widths="300">
| |
| Image:Ebstein diagram.jpg|Graphical represntation of Ebstein's Anomaly from the Mayo Clinic website (note there is also an ASD on this diagram)
| |
| Image:EbsteinAnomaly.png|Ebstein Anomaly
| |
| </gallery>
| |
| </div>
| |
|
| |
| == Epidemiology and Demographics ==
| |
|
| |
| *Is a rare congenital heart disease.
| |
| *About 1:1,000 patients with [[congenital heart disease]], or 1:210,000 live births.
| |
| *Males = females.
| |
| *Higher incidence in infants whose mothers are treated with [[Lithium]] Carbonate during pregnancy
| |
|
| |
| == Genetics ==
| |
| *Multifactorial inheritance, risk if a sibling has the disease is 1%.
| |
|
| |
| == Diagnosis ==
| |
|
| |
| === History ===
| |
| *Presentation depends greatly on the degree of apical displacement of the tricuspid valve leaflet as well as the degree of dysfunction of the [[tricuspid valve]]. If the [[tricuspid valve]] is severely deformed, [[fetal hydrops]] may occur. If the valve is functioning, patients may remain symptom free for many years.
| |
|
| |
| *The majority of patients have [[dyspnea]] and [[cyanosis]] (40%) but some may be asymptomatic.
| |
|
| |
| *Palpitations may occur secondary to SVTs ([[supraventricular tachycardia]]) and [[WPW]] ([[Wolff-Parkinson-White syndrome]]) (8%).
| |
|
| |
| *Growth and development are normal.
| |
|
| |
| === Physical Examination ===
| |
|
| |
| ====General Appearance====
| |
| Patients may have a bluish coloration of their face depending on the degree of [[cyanosis]] and right to left shunting.
| |
|
| |
| ==== Heart ====
| |
| Because the RA is dilated and compliant, there are no large v waves even in the presence of TR ([[tricuspid regurgitation]]) and the jugular venous pressure is often normal on exam. The chest may be asymmetric due to an enlarged right heart.
| |
|
| |
| The first heart sound is widely split. There is a wide split S2 as a result of [[RBBB]] and delayed closure of the pulmonic valve. TR ([[tricuspid regurgitation]]), produces a holosystolic murmur which is heard best along the left lower sternal border and increases with inspiration.
| |
|
| |
| === Laboratory Findings ===
| |
|
| |
| ==== Electrocardiogram ====
| |
|
| |
| The EKG is abnormal in 50 to 67%.
| |
|
| |
| About 50% of individuals with Ebstein's anomaly have evidence of [[Wolff-Parkinson-White Syndrome]] (syndrome of pre-excitation of the ventricles due to an accessory pathway known as the Bundle of Kent), secondary to the the apical displacement of the septal tricuspid valve leaflet resulting in discontinuity of the central fibrous body.
| |
|
| |
| [[Image:Ebstein's anomaly ECG.png|thumb|left|350px|10-lead ECG of a woman with '''Ebstein's anomaly'''. The ECG shows signs of right atrial enlargement, best seen in V1. Other P waves are broad and tall, these are termed "Himalayan" P waves. There is also a right bundle branch block pattern and a first degree atrioventricular block (prolonged PR-interval) due to intra-atrial conduction delay. There is no evidence of a Kent-bundle in this patient. There is T wave inversion in V1-4 and a marked Q wave in III; these changes are characteristic for Ebstein's anomaly and do not reflect ischemic ECG changes in this patient.]]
| |
| <br clear="left"/>
| |
|
| |
| Other abnormalities that can be seen on the ECG include:<ref name="pmid18056539">{{cite journal |author=Khairy P, Marelli AJ |title=Clinical use of electrocardiography in adults with congenital heart disease |journal=Circulation |volume=116 |issue=23 |pages=2734–46 |year=2007 |month=December |pmid=18056539 |doi=10.1161/CIRCULATIONAHA.107.691568 |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=18056539}}</ref>
| |
|
| |
| (1) signs of right atrial enlargement or tall and broad 'Himalayan' P waves,
| |
|
| |
| (2) first degree atrioventricular block manifesting as a prolonged PR-interval,
| |
|
| |
| (3) low amplitude QRS complexes in the right precordial leads,
| |
|
| |
| (4) atypical [[right bundle branch block]],
| |
|
| |
| (5) T wave inversion in V1-V4 and Q waves in V1-V4 and II, III and aVF.
| |
|
| |
| (6) a short [[PR interval]] and a [[delta wave]] and low voltages.
| |
|
| |
| ==== Chest X Ray ====
| |
|
| |
| The Chest X-ray shows a balloon shaped heart that looks a lot like a [[pericardial effusion]]. The RA is dilated. The heart looks globular.
| |
|
| |
| [[Image:Ebstein's anomaly 001.jpg|thumb|left|350px|Chest x-ray of a patient with Ebstein anomaly]]
| |
| <br clear="left"/>
| |
|
| |
| ==== Echocardiogram ====
| |
|
| |
| See [[Echo in Ebstein's anomaly of the tricuspid valve]] for more info/images
| |
|
| |
| a) Can be used to assess the severity of dilatation of the [[right atrium]], and the functional status of the [[tricuspid valve]] as well as the [[right ventricle]].
| |
|
| |
| b) Normally the tricuspid valve closes within 30 msec of the mitral valve. In Ebstein's, the tricuspid valve closes 50 to 60 msec after the mitral valve.
| |
|
| |
| c) The delayed tricuspid closure is not due to [[RBBB]] because it also occurs with preexcitation.
| |
|
| |
| d) 2D ECHO allows you to assess whether the repair can be accomplished without a prosthetic valve, and detects whether an interatrial shunt is present.
| |
|
| |
| [[Image:Ebstein4.jpg|left|400px|thumb|Pathological specimen and ultrasound image of a heart with Ebstein's anomaly. Abbreviations: RA: Right atrium; ARV: Atrialized right ventricle; FRV: Functional right ventricle; AL: Anterior leaflet; SL: Septal leaflet; LA: Left atrium; LV: Left ventricle; asterisk: grade II tethering of the tricuspid septal leaflet.]]
| |
| <br clear="left"/>
| |
| Below is an apical 4-chamber transthoracic view, showing apically-displaced leaflets of the tricuspid valve. Note substantial [[tricuspid regurgitation]], which originates close to the apex, where the abnormal leaflets actually coapt:
| |
|
| |
| <Youtube v=KEko3kM26bY/>
| |
|
| |
| ===CT and MRI===
| |
|
| |
| Inferior displacement of tricuspid valve leaflets with enlargement of the right atrium and enlargement and dysfunction of the [[right ventricle]].
| |
|
| |
| ==== Cardiac catheterization and hemodynamics ====
| |
|
| |
| a) RA pressure usually not increased due to the fact that the RA is enlarged and compliant.
| |
|
| |
| b) Normal RV pressures unless significant [[TR]] is present.
| |
|
| |
| c) PA pressures are normal or slightly decreased due to [[TR]] and a large right-to-left shunt.
| |
|
| |
| d) An [[ASD]] may be present
| |
|
| |
| == Treatment ==
| |
|
| |
| ===Pharmagolical Management===
| |
|
| |
| Ebstein's cardiophysiology typically presents as an (antidromic) [[AV nodal reentrant tachycardia]] with associated [[pre-excitation]]. In this setting, the preferred pharmacological treatment agent is [[procainamide]]. Since AV-blockade may promote conduction over the accessory pathway, drugs like [[beta blockers]], [[calcium channel blocker]]s and [[digoxin]] are contraindicated.
| |
|
| |
| If there is [[atrial fibrillation]] with pre-excitation, treatment options include [[procainamide]], [[flecainide]], [[propafenone]], [[dofetilide]] and [[ibutilide]] since these medications slow conduction in the accessory pathway causing the tachycardia and should be administered before considering electrical [[cardioversion]]. Intravenous [[amiodarone]] may also convert atrial fibrillation and/or slow the ventricular response.
| |
|
| |
| === Mechanical and Device Based Therapy ===
| |
|
| |
| The protracted natural history of this disease in contrast to the uncertainty of long-term results of surgical intervention supports the policy of postponing surgical intervention until the onset of disability.
| |
|
| |
| ===Surgery may include===
| |
|
| |
| - Tricuspid valve repair or replacement (when possible repair is preferable to replacement as it is associated with a lower mortality rate and fewer complications).
| |
|
| |
| *[[Atrial septal defect]] repair.
| |
| *Right atrial plication (unclear whther this improves right ventricular function).
| |
| *Cardiac defibrillator implantation.
| |
| *Accessory pathways may require surgical intervention or ablation.
| |
|
| |
| Hospital mortality at the Mayo for valve reconstruction is 6.7%. Only 1.6% in the Mayo series required reoperation. Long term follow up in the Mayo series showed 92% to have Class I or II symptoms and a 10 year mortality rate of 8%.
| |
|
| |
| Generally, surgical treatment improves the exercise intolerance from NYHA-FC III or IV to NYHA-FC I or II.
| |
|
| |
|
| Regardless of severity of the Ebstein’s Anomaly and type of treatment, risk of sudden death remains an important issue in patients with Ebstein's anomaly.
| | '''For patient information, click [[{{PAGENAME}} (patient information)|here]]''' |
| | {{Ebstein's anomaly of the tricuspid valve}} |
|
| |
|
| ==Prognosis==
| | {{CMG}}; '''Associate Editor-In-Chief:''' [[Priyamvada Singh|Priyamvada Singh, M.B.B.S.]] [mailto:psingh13579@gmail.com]; {{CZ}}}; '''Assistant Editor-In-Chief:''' [[Kristin Feeney|Kristin Feeney, B.S.]] [mailto:kfeeney@elon.edu] |
|
| |
|
| ===Adverse prognostic factors are=== | | ==[[Ebstein's anomaly of the tricuspid valve overview|Overview]]== |
|
| |
| a) NYHA Class III or IV
| |
|
| |
|
| b) Moderate to severe [[cardiomegaly]]
| | ==[[Ebstein's anomaly of the tricuspid valve anatomy|Anatomy]]== |
|
| |
|
| c) [[Cyanosis]] or an O2 sat < 90%
| | ==[[Ebstein's anomaly of the tricuspid valve historical perspective|Historical Perspective]]== |
|
| |
|
| d) Disability during infancy
| | ==[[Ebstein's anomaly of the tricuspid valve pathophysiology|Pathophysiology]]== |
|
| |
|
| e)Paradoxical emboli
| | ==[[Ebstein's anomaly of the tricuspid valve causes|Causes]]== |
|
| |
|
| ==References== | | ==[[Ebstein's anomaly of the tricuspid valve differential diagnosis|Differentiating Ebstein’s anomaly of the tricuspid valve from other Disorders]]== |
| {{Reflist}}
| |
|
| |
|
| ==Additional Resources== | | ==[[Ebstein's anomaly of the tricuspid valve epidemiology and demographics|Epidemiology and demographics]]== |
|
| |
|
| * Emma C. Ferguson, Rajesh Krishnamurthy, and Sandra A. A. Oldham. [http://radiographics.rsnajnls.org/cgi/content/abstract/27/5/1323 Classic Imaging Signs of Congenital Cardiovascular Abnormalities.] RadioGraphics 2007 27: 1323-1334.
| | ==[[Ebstein's anomaly of the tricuspid valve risk factors|Risk Factors]]== |
| * Joris P. A. Beerepoot, and Pamela K. Woodard. [http://radiology.rsnajnls.org/cgi/content/full/231/3/747 Case 71: Ebstein Anomaly]. Radiology 2004 231: 747-751.
| |
|
| |
|
| ==External Links== | | ==[[Ebstein's anomaly of the tricuspid valve natural history, complications & prognosis|Natural history, Complications, and Prognosis]]== |
| * [http://goldminer.arrs.org/search.php?query=Ebstein's%20anomaly Goldminer: Ebstein's anomaly]
| |
|
| |
|
| ==Acknowledgements and Initial Contributors to Page== | | ==Diagnosis== |
| | [[Ebstein's anomaly of the tricuspid valve history and symptoms|History and Symptoms]] | [[Ebstein's anomaly of the tricuspid valve physical examination|Physical Examination]] | [[Ebstein's anomaly of the tricuspid valve electrocardiogram | Electrocardiogram]] | [[Ebstein's anomaly of the tricuspid valve chest x ray|Chest X Ray]] | [[Ebstein's anomaly of the tricuspid valve MRI|MRI]] | [[Ebstein's anomaly of the tricuspid valve CT|CT]] | [[Ebstein's anomaly of the tricuspid valve echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Ebstein's anomaly of the tricuspid valve other imaging findings|Cardiac Catheterization]] | [[Ebstein's anomaly of the tricuspid valve other diagnostic studies|Electrophysiological Testings]] | [[Ebstein's anomaly of the tricuspid valve ACC/AHA Guidelines for diagnostic tests |ACC/AHA Guidelines for Diagnostic Tests ]] | [[Ebstein's anomaly of the tricuspid valve ACC/AHA Guidelines for evaluation of Patients|ACC/AHA Guidelines for Evaluation of Patients]] |
|
| |
|
| Leida Perez, M.D.
| | ==Treatment== |
| | [[Ebstein's anomaly of the tricuspid valve medical therapy|Medical Therapy]] | [[Ebstein's anomaly of the tricuspid valve surgery|Surgery]] | [[Ebstein's anomaly of the tricuspid valve primary prevention|Prevention]] | [[Ebstein's anomaly of the tricuspid valve ACC/AHA Guidelines for reproduction|ACC/AHA Guidelines for Reproduction]] |
|
| |
|
| {{Congenital malformations and deformations of circulatory system}}
| | [[Category:Cardiovascular system]] |
| {{SIB}}
| |
| [[Category:DiseaseState]] | |
| [[Category:Cardiology]] | | [[Category:Cardiology]] |
| | [[Category:Congenital heart disease]] |
| | [[Category:Pediatrics]] |
| | [[Category:Disease]] |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WH}} |
| {{WikiDoc Sources}} | | {{WS}} |