Differentiating Diabetes insipidus from other diseases: Difference between revisions
No edit summary |
|||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
The most important differential diagnosis for diabetes insipidus include: Central diabetes insipidus, acquired, [[Trauma]] ([[surgery]], deceleration injury), [[Vascular]] ([[cerebral hemorrhage]], [[infarction]], [[anterior communicating artery aneurysm]] or [[ligation]], intra-hypothalamic [[hemorrhage]]), [[Neoplastic]] ([[craniopharyngioma]], [[meningioma]], [[germinoma]], [[pituitary tumor]] or [[Metastasis|metastases]]), [[Granulomatous]] ([[histiocytosis]], [[sarcoidosis]]), [[Infectious]] ([[meningitis]], [[encephalitis]]), [[Inflammatory]]/[[autoimmune]] ([[lymphocytic]] infundibuloneurohypophysitis), [[Drug]]/[[toxin]]-induced ([[ethanol]], [[diphenylhydantoin]], snake venom), [[hydrocephalus]], [[Idiopathic]], [[Congenital disorder|congenital]], [[Congenital malformations]], nephrogenic diabetes insipidus: [[Acquired disorder|Acquired]], drug-induced ([[demeclocycline]], [[lithium]], [[cisplatin]], [[methoxyflurane]], etc.), [[Hypercalcemia]], [[hypokalemia]], infiltrating lesions ([[sarcoidosis]], [[amyloidosis]], [[multiple myeloma]], [[Sjögren's syndrome|Sjogren's disease]]), [[Vascular]] ([[Sickle-cell disease|sickle cell disease]]), congenital, [[X-linked recessive]], primary polydipsia,[[Psychogenic]], dipsogenic (downward resetting of thirst threshold), gestational diabetes insipidus, [[Diabetes mellitus]]. | |||
Central diabetes insipidus | |||
[[Trauma]] ([[surgery]], deceleration injury) | |||
[[Vascular]] ([[cerebral hemorrhage]], [[infarction]], [[anterior communicating artery aneurysm]] or [[ligation]], intra-hypothalamic [[hemorrhage]]) | |||
[[Neoplastic]] ([[craniopharyngioma]], [[meningioma]], [[germinoma]], [[pituitary tumor]] or [[Metastasis|metastases]]) | |||
[[Granulomatous]] ([[histiocytosis]], [[sarcoidosis]]) | |||
[[Infectious]] ([[meningitis]], [[encephalitis]]) | |||
[[Inflammatory]]/[[autoimmune]] ([[lymphocytic]] infundibuloneurohypophysitis) | |||
[[Drug]]/[[toxin]]-induced ([[ethanol]], [[diphenylhydantoin]], snake venom) | |||
[[Congenital disorder| | |||
[[Congenital malformations]] | |||
[[Acquired disorder|Acquired]] | |||
[[Hypercalcemia]], [[hypokalemia]] | |||
[[Vascular]] ([[Sickle-cell disease|sickle cell disease]]) | |||
[[X-linked recessive]] | |||
[[Psychogenic]] | |||
[[Diabetes mellitus]] | |||
== Differentiating diabetes insipidus based on the type of diabetes insipidus caused == | == Differentiating diabetes insipidus based on the type of diabetes insipidus caused == | ||
<ref name="pmid10369876">{{cite journal| author=Willcutts MD, Felner E, White PC| title=Autosomal recessive familial neurohypophyseal diabetes insipidus with continued secretion of mutant weakly active vasopressin. | journal=Hum Mol Genet | year= 1999 | volume= 8 | issue= 7 | pages= 1303-7 | pmid=10369876 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10369876 }} </ref><ref name="pmid19897608">{{cite journal| author=Abu Libdeh A, Levy-Khademi F, Abdulhadi-Atwan M, Bosin E, Korner M, White PC et al.| title=Autosomal recessive familial neurohypophyseal diabetes insipidus: onset in early infancy. | journal=Eur J Endocrinol | year= 2010 | volume= 162 | issue= 2 | pages= 221-6 | pmid=19897608 | doi=10.1530/EJE-09-0772 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19897608 }} </ref> | The most important differential diagnosis for diabetes insipidus include:<ref name="pmid10369876">{{cite journal| author=Willcutts MD, Felner E, White PC| title=Autosomal recessive familial neurohypophyseal diabetes insipidus with continued secretion of mutant weakly active vasopressin. | journal=Hum Mol Genet | year= 1999 | volume= 8 | issue= 7 | pages= 1303-7 | pmid=10369876 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10369876 }} </ref><ref name="pmid19897608">{{cite journal| author=Abu Libdeh A, Levy-Khademi F, Abdulhadi-Atwan M, Bosin E, Korner M, White PC et al.| title=Autosomal recessive familial neurohypophyseal diabetes insipidus: onset in early infancy. | journal=Eur J Endocrinol | year= 2010 | volume= 162 | issue= 2 | pages= 221-6 | pmid=19897608 | doi=10.1530/EJE-09-0772 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19897608 }} </ref><ref name="pmid9350817">{{cite journal| author=Barrett TG, Bundey SE| title=Wolfram (DIDMOAD) syndrome. | journal=J Med Genet | year= 1997 | volume= 34 | issue= 10 | pages= 838-41 | pmid=9350817 | doi= | pmc=1051091 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9350817 }} </ref> | ||
<small><small> | <small><small> | ||
Revision as of 21:14, 27 October 2017
|
Diabetes insipidus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Differentiating Diabetes insipidus from other diseases On the Web |
|
American Roentgen Ray Society Images of Differentiating Diabetes insipidus from other diseases |
|
FDA on Differentiating Diabetes insipidus from other diseases |
|
CDC on Differentiating Diabetes insipidus from other diseases |
|
Differentiating Diabetes insipidus from other diseases in the news |
|
Blogs on Differentiating Diabetes insipidus from other diseases |
|
Risk calculators and risk factors for Differentiating Diabetes insipidus from other diseases |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Omodamola Aje B.Sc, M.D. [2]
Overview
The most important differential diagnosis for diabetes insipidus include: Central diabetes insipidus, acquired, Trauma (surgery, deceleration injury), Vascular (cerebral hemorrhage, infarction, anterior communicating artery aneurysm or ligation, intra-hypothalamic hemorrhage), Neoplastic (craniopharyngioma, meningioma, germinoma, pituitary tumor or metastases), Granulomatous (histiocytosis, sarcoidosis), Infectious (meningitis, encephalitis), Inflammatory/autoimmune (lymphocytic infundibuloneurohypophysitis), Drug/toxin-induced (ethanol, diphenylhydantoin, snake venom), hydrocephalus, Idiopathic, congenital, Congenital malformations, nephrogenic diabetes insipidus: Acquired, drug-induced (demeclocycline, lithium, cisplatin, methoxyflurane, etc.), Hypercalcemia, hypokalemia, infiltrating lesions (sarcoidosis, amyloidosis, multiple myeloma, Sjogren's disease), Vascular (sickle cell disease), congenital, X-linked recessive, primary polydipsia,Psychogenic, dipsogenic (downward resetting of thirst threshold), gestational diabetes insipidus, Diabetes mellitus.
Differentiating diabetes insipidus based on the type of diabetes insipidus caused
The most important differential diagnosis for diabetes insipidus include:[1][2][3]
| Type of DI | Subclass | Disease | Defining signs and symptoms | Lab/Imaging findings |
|---|---|---|---|---|
| Central | Acquired | Histiocytosis |
|
 |
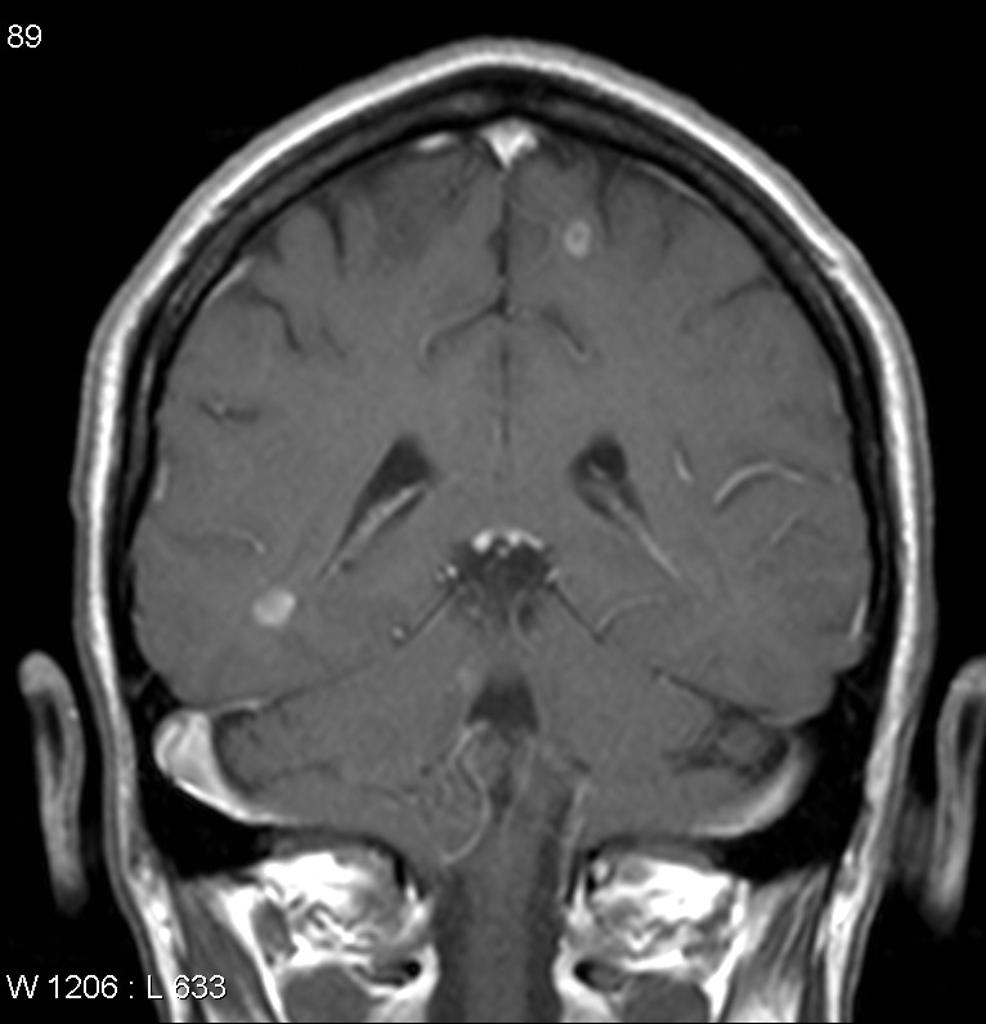
| Craniopharyngioma |
|
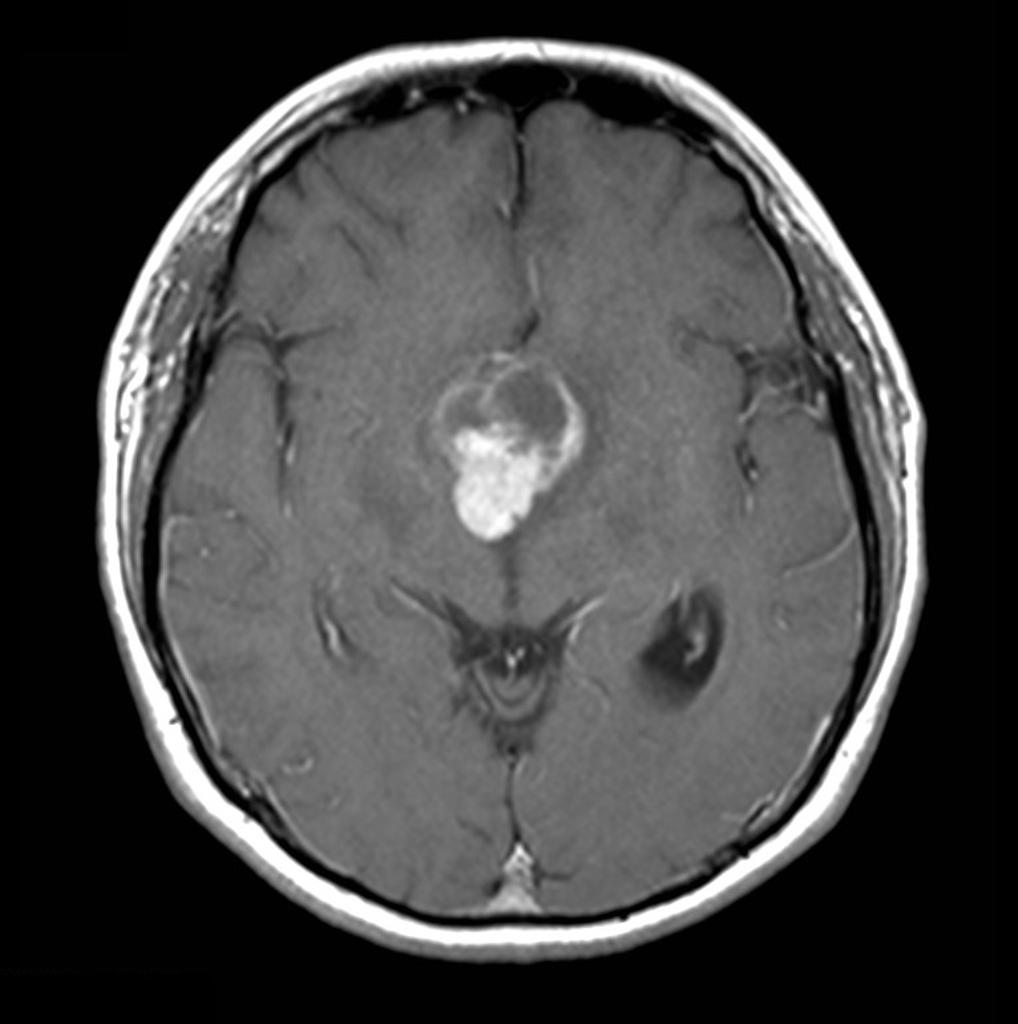 | ||
| Sarcoidosis |
|
 | ||
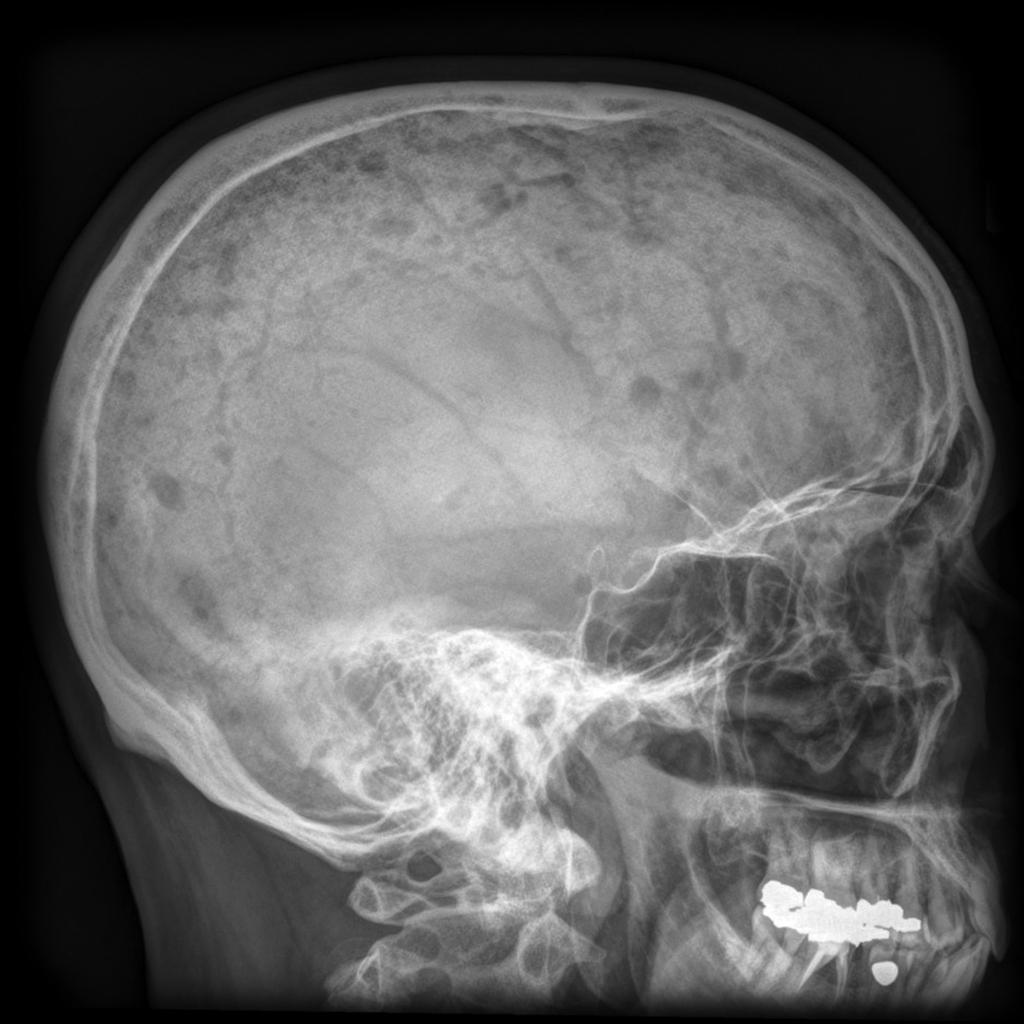
| Congenital | Hydrocephalus |
|
Dilated ventricles on CT and MRI
 | |
| Wolfram Syndrome (DIDMOAD) |
| |||
| Nephrogenic | Acquired | Drug-induced (demeclocycline, lithium) |
| |
| Hypercalcemia |
| |||
| Hypokalemia |
| |||
| Multiple myeloma |
|
 | ||
| Sickle cell disease |
|
 | ||
| Primary polydipsia | Psychogenic |
| ||
| Gestational diabetes insipidus |
| |||
| Diabetes mellitus |
| |||
References
- ↑ Willcutts MD, Felner E, White PC (1999). "Autosomal recessive familial neurohypophyseal diabetes insipidus with continued secretion of mutant weakly active vasopressin". Hum Mol Genet. 8 (7): 1303–7. PMID 10369876.
- ↑ Abu Libdeh A, Levy-Khademi F, Abdulhadi-Atwan M, Bosin E, Korner M, White PC; et al. (2010). "Autosomal recessive familial neurohypophyseal diabetes insipidus: onset in early infancy". Eur J Endocrinol. 162 (2): 221–6. doi:10.1530/EJE-09-0772. PMID 19897608.
- ↑ Barrett TG, Bundey SE (1997). "Wolfram (DIDMOAD) syndrome". J Med Genet. 34 (10): 838–41. PMC 1051091. PMID 9350817.
- ↑ Ghosh KN, Bhattacharya A (1992). "Gonotrophic nature of Phlebotomus argentipes (Diptera: Psychodidae) in the laboratory". Rev Inst Med Trop Sao Paulo. 34 (2): 181–2. PMID 1340034.